During transvaginal hysterectomy, the uterosacral-cardinal ligament complex must be reattached to the vagina. The following steps can be performed at the beginning or the end of the procedure. I perform these steps at the beginning of a transvaginal hysterectomy so that the sutures are not cut by mistake later in the procedure, and so that these steps are not forgotten if the procedure becomes difficult or complicated. If the support is defective at the beginning of the case, I use a more proximal attachment of the uterosacral ligament to the cuff at the end of the procedure.
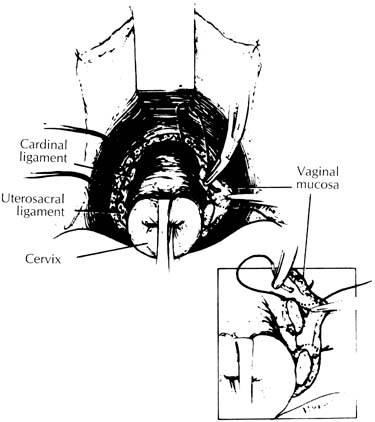
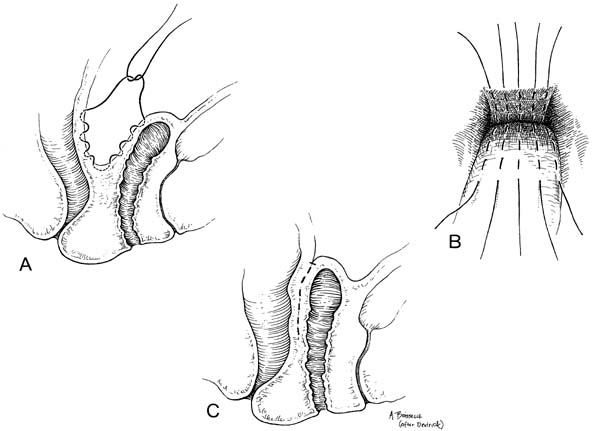
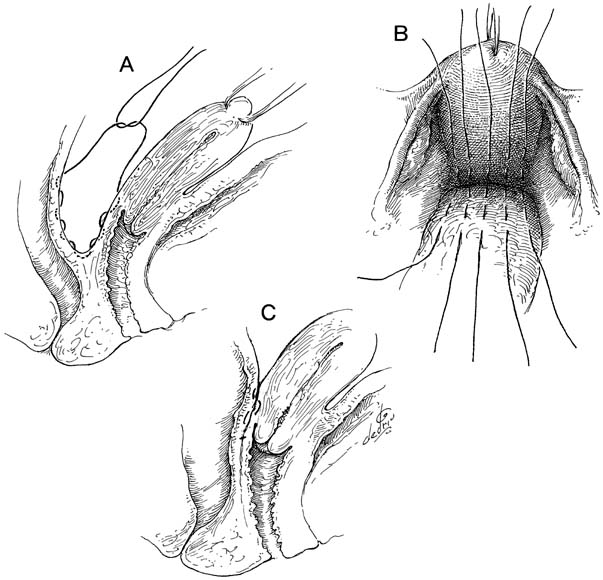
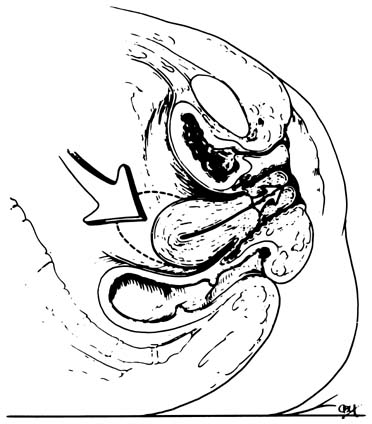
After the anterior and posterior cul-de-sacs are entered, the uterosacral and cardinal ligaments are cut and ligated. If these supporting structures are not frail or attenuated, the pedicles are sutured to the vaginal membrane (Fig. 1). By securing the pedicles to the lateral angles of the vagina, the vault is supported and the lateral angles of the vaginal cuff are readily sutured. Care must be taken because these are common sources of postoperative bleeding. These steps are completed during any transvaginal hysterectomy. If the indication for hysterectomy includes uterovaginal prolapse, these ligaments must be shortened to eliminate any laxity that is present. Shortening can be accomplished at the beginning of the procedure as long as the anterior cul-de-sac has been entered and the bladder retracted. This step elevates the bladder and ureters out of harm's way. If the uterosacral-cardinal ligaments need shortening but hysterectomy must be performed without entering the anterior cul-de-sac, the shortening steps should be performed after the uterus is removed and the bladder and ureters are elevated. A recent study showed that in all patients except those with severe uterovaginal prolapse or procidentia, the ureter actually is protected by the cutting of the cardinal ligaments at the start of the procedure.4 This step allows the ureters to fall laterally and retract toward the lateral pelvic sidewall.
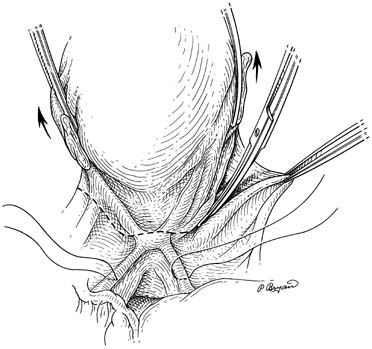
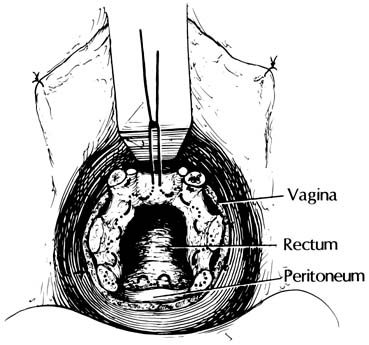
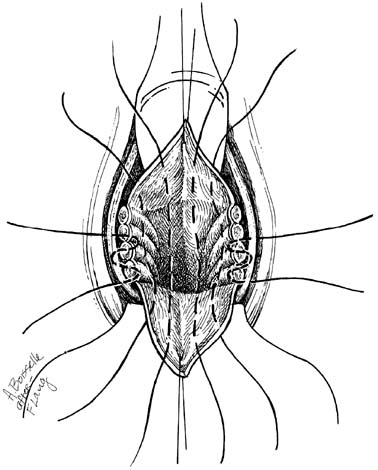
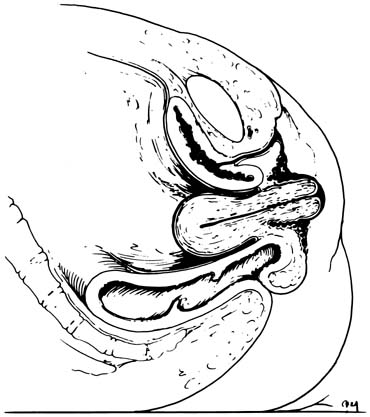
The McCall culdoplasty or a modification of this procedure is another means of supporting the vaginal cuff during transvaginal hysterectomy.5,6,7 This procedure incorporates the uterosacral and cardinal ligaments to the peritoneal surface. The sutures are attached so that when tied, the uterosacral-cardinal ligaments are drawn toward the midline, thereby helping to close off the cul-de-sac. In addition, when the suture is tied, it draws the posterior vaginal apex up to the supporting structures, elevating it to a normal position. This maneuver can be performed with one or more sutures (Fig. 2). The only drawback to this type of culdoplasty is a possible increased incidence of kinking or ligating the ureter, because it is so close to the uterosacral ligament.
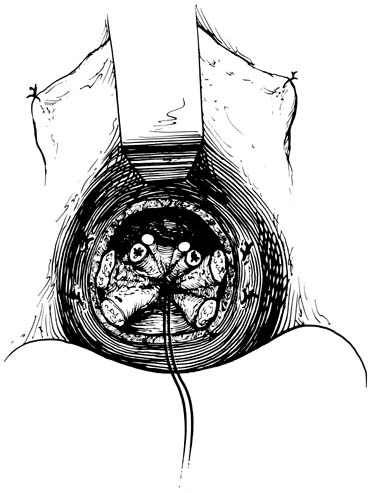
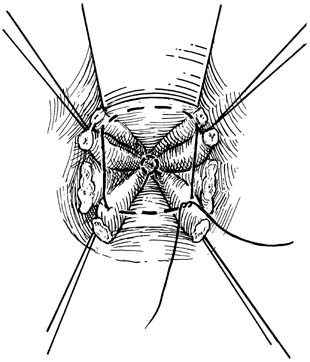
Any modification of these procedures to attach the supporting structures (uterosacral cardinals) to the vagina will work. The important point is to perform these steps during the transvaginal hysterectomy. During an abdominal hysterectomy, the cardinal and uterosacral ligaments also should be attached to the vaginal cuff. As soon as the uterus and cervix are removed, the uterosacral pedicles are sewn to the lateral angles of the vagina. They may be incorporated as part of the lateral angle stitch or separately. There is no need to incorporate the round ligaments to the cuff, because they do not aid in cuff suspension and, in fact, may draw the ovaries to a position overlying the vaginal apex, predisposing the patient to dyspareunia.
Emphasis should be given to preventing posthysterectomy vault prolapse. Prolapse of the vagina results from the loss of normal pelvic support or occurs as a result of omitting the steps that use these pelvic support tissues during hysterectomy. This complication occurs after either transvaginal or transabdominal hysterectomy; hysterectomy alone will not cure uterovaginal prolapse. Hysterectomy permits the surgeon to visualize and use the supportive structures, attaching them to the vaginal membrane.
Several methods of vaginal fixation at the time of hysterectomy are currently recognized. Surgeons should attempt to prevent posthysterectomy prolapse by using the cardinal-uterosacral complex as described.