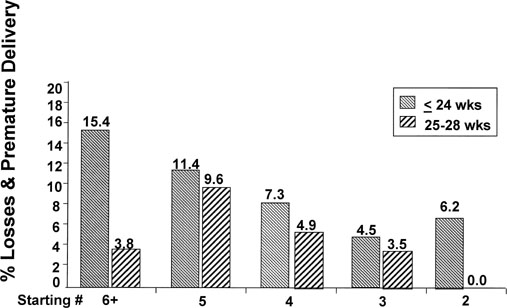
Several centers with the world’s largest experience with MFPR have collaborated to leverage the power of their data. In 1993, the first collaborative report showed a 16% pregnancy loss rate through 24 completed weeks.12 This rate was a major improvement compared with expectations of higher order multiple pregnancies, particularly of quadruplets and more. In 1994, 1996, and 2001, multicenter reports showed continued dramatic improvements in the overall outcomes of such pregnancies (Table 3).13,14,15 The 2001 collaborative data show that the outcomes of triplets reduced to twins and quadruplets reduced to twins are essentially as if they started as twins (Fig. 1).1 Even with the tremendous advances in neonatal care for premature infants, the 95% take-home baby rate for triplets and the 92% take-home baby rate for quadruplets are dramatic improvements over natural statistics. The pregnancy loss rate and the rate of very early prematurity have been reduced substantially. The loss and the prematurity rates continue to be a direct function of the starting number. There still is a price to be paid for overaggressive infertility therapies.
TABLE 3. Multifetal Pregnancy Reduction—Losses by Years
Losses (wk) | Deliveries (wk) | ||||||
Total | <24(%) | >24(%) | 25–28(%) | 29–32(%) | 33–36(%) | >37(%) | |
1986–90 |
508 |
13.2 |
4.5 |
10.0 |
21.1 |
15.7 |
35.4 |
1991–94 |
724 |
9.4 |
0.3 |
2.8 |
5.4 |
21.1 |
61.0 |
1995–98 |
1356 |
6.4 |
0.2 |
4.3 |
10.2 |
31.5 |
47.4 |
Evans MI, Berkowitz R, Wapner R, et al: Multifetal pregnancy reduction (MFPR): Improved outcomes with increased experience. Am J Obstret Gynecol 184:97, 2001.
|
Finishing number data also showed lowest pregnancy loss rates for cases reduced to twins with increasing losses for singletons followed by triplets. The rate of early premature delivery was highest, however, with triplets followed by twins and lowest with singletons. Mean gestational age at delivery was also lower for higher order cases.
Birth weights after MFPR decreased with starting and finishing numbers reflecting increased prematurity. Analysis of birth weight percentiles, particularly for singletons, reflects falling percentiles with starting number, from 51.75 for 2 decreased to 1 to 31.26 for 4 decreased to 1. In remaining twins, the rate of birth weight percentile discordancy among the twins increased from 0.57% for starting triplets to 4.86% for starting quintuplets and higher. For remaining triplets, the percentile differences were even greater. Analysis of the data suggests that the improvements in MFPR outcomes are a function of extensive operator experience combined with improved ultrasound.
Most observers except those completely opposed to intervention on religious grounds accepted MFPR with quadruplets or more and saw no need at twins.16 The debate concerns triplets. Although there are conflicting data in the literature, our experience suggests that triplets reduced to twins do much better in terms of loss and prematurity than unreduced triplets. We believe that if a patient’s primary goal is to maximize the chances of healthy children, reduction of triplets to twins achieves the best results.
Several previous articles argued whether triplets have better outcomes, “reduced” or not. Yaron and colleagues17 looked at triplets reduced to twins and compared these data with unreduced triplets and with two large cohorts of twins. The data showed substantial improvement of reduced twins compared with triplets. The data from the most recent collaborative series suggest that pregnancy outcomes for cases starting at triplets or quadruplets reduced to twins do fundamentally as well as starting at twins and support some cautious aggressiveness in infertility treatments to achieve pregnancy in difficult situations. When higher numbers occur, good outcomes clearly diminish. A 2001 study suggested that reduced tiplets did worse than continuing ones. Analysis of that series showed, however, a loss rate after MFPR twice that seen in our collaborative series18 and worse outcome data in every other category for remaining triplets. One must use extreme caution in choosing comparison groups. Many other reports have compared reduced versus unreducedtriplets. The data show better outcomes with reduction (Table 4).
TABLE 4. Reduced Versus Unreduced Triplets Comparison
|
Multifetal Pregnancy Reduction Cases |
||||||
|
Deliveries (wk) |
||||||
|
Years |
Losses |
<24 wk |
24–28 (%) |
29–32 (%) |
33–36 (%) |
>37 (%) |
|
1980s |
6.7 |
6.1 |
9.1 |
36.9 |
47.9 |
|
|
1990–94 |
5.7 |
5.2 |
9.9 |
39.2 |
45.2 |
|
|
1995–98 |
4.5 |
3.2 |
6.9 |
28.3 |
55.1 |
|
|
1998–2002 |
5.1 |
4.6 |
10.8 |
41.8 |
37.6 |
|
|
Mean GA, 35.5; *PMR, 10.0/1000 |
||||||
|
1998–2002(3≥ 1) |
8.0 |
4.0 |
12.0 |
4.0 |
72.0 |
|
|
Mean GA, 39.5; *PMR, 0/1000 |
||||||
|
Nonreduced Triplets |
|||
|
1998(Leondires)21 |
9.9% |
Mean GA, 33.3; |
PMR, 55/1000 |
|
1999(Angel)22 |
8.0% |
Mean GA, 32.3; |
PMR, 29/1000 |
|
2001(Lipitz)23 |
25.0% |
Mean GA, 33.5; |
PMR, 109/1000 |
|
2002(Francois)24 |
8.3% |
Mean GA, 31.0; |
PMR, 57.6/1000 |
*GA, gestational age; PMR, perinatal mortality rate.
Pregnancy loss is not the only poor outcome. Very early premature delivery correlates with the starting number. The data on diminishing birth weight percentile in singletons and discordancy in twins are of concern, consistent with a belief that there is perhaps a fundamental “imprinting” of the uterus early in pregnancy that is not completely undone by MFPR.15,18
The subset of patients in the 2001 collaborative report reduced from two to one (not for fetal anomalies) included 154 patients. Nine patients lost their pregnancies before 24 weeks, and two delivered between 25 and 28 weeks. Although, in absolute terms, the numbers are not large compared with other categories, they suggest a loss rate comparable to 3 to 2. In an earlier series, in about one third of the two reduced to one cases, there was a medical indication for the procedure (e.g., maternal cardiac disease, prior twin pregnancy with severe prematurity, or uterine abnormality).14 In more recent years, most such cases are from women in their 40s or 50s who are using donor eggs, who, more for personal reasons than medical, want only a singleton pregnancy.19 The effect of maternal age per se is negligible, however, explaining only 3.5% of the variance, suggesting that with reduction, “older” gravidas do nearly as well as their younger counterparts.14,19