Not surprisingly, analysis demonstrates that patients who are well informed
about potential side effects prior to insertion are most likely to
be more satisfied than less well informed women, whether or not they
actually experience any problems.33,51 Table 2 summarizes the significant clinical events that led to discontinuation
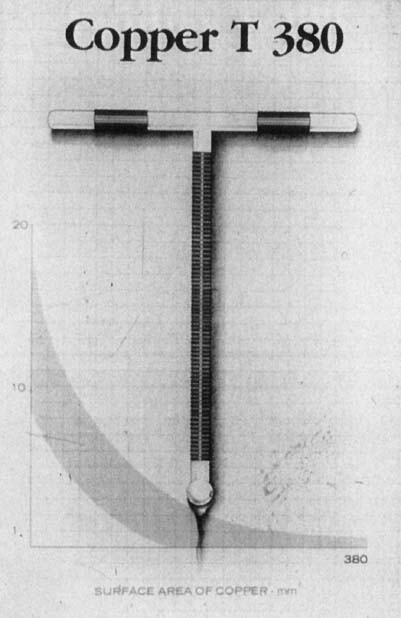
of the copper IUD over the 10-year period of clinical trials. Table 3 displays 5-year cumulative discontinuation rates by cause for the LNG-IUS. TABLE 2. Gross Annual Termination and Continuation Rates Per 100* Users for All Copper T 380A IUD Acceptors (Parous and Nulliparous): Combined
Population Council and WHO Studies1
Year |
Rate of Item |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
Pregnancy |
0.7 |
0.3 |
0.6 |
0.2 |
0.3 |
0.2 |
0.0 |
0.4 |
0.0 |
0.0 |
Expulsion |
5.7 |
2.5 |
1.6 |
1.2 |
0.3 |
0.0 |
0.6 |
1.7 |
0.2 |
0.4 |
Bleeding/pain |
11.9 |
9.8 |
7.0 |
3.5 |
3.7 |
2.7 |
3.0 |
2.5 |
2.2 |
3.7 |
Other medical |
2.5 |
2.1 |
1.6 |
1.7 |
0.1 |
0.3 |
1.0 |
0.4 |
0.7 |
0.3 |
Continuation |
76.8 |
78.3 |
81.2 |
86.2 |
89.0 |
91.9 |
87.9 |
88.1 |
92.0 |
91.8 |
*Rates were calculated by weighing the annual rates by the number of subjects
starting each year for each of the Population Council (3536 acceptors) and
the World Health Organization (1396 acceptors) trials.
TABLE 3. Cumulative Gross Rates of Termination for the Levonorgestrel-Releasing
Intrauterine System per One Hundred Women For Five Years of Use52
Pregnancy |
0.5 |
Expulsion |
5.8 |
Bleeding problems |
13.7 |
Amenorrhea |
6.0 |
PID |
0.8 |
Hormonal side effects |
12.1 |
Other medical |
9.2 |
Continuation |
45–65 | Pregnancy-Related Events The pregnancy rate in the first year of use in the clinical trial with
the copper T-380A was 0.7%. Parous women had lower rates (0.5% to 0.8%), and nulliparous women had slightly higher rates
of failure (0.8% to 1.2%). The cumulative 8-year pregnancy
rates in various studies ranged from 1.4% to 1.8%. International
studies indicate a 10- to 12-year cumulative rate of 2.7% for
all women, with no pregnancies occurring after the eighth
year of use.3 For the LNG-IUS, the pregnancy rate in the first year of use was 0.14%. The
cumulative 5-year pregnancy rate was 0.71%. Meta-analysis
shows that there is no significant difference in efficacy between
the two types of IUDs.10 If a woman becomes pregnant while using the IUD, it is recommended that
the IUD be removed if she is in the first trimester, the IUD tail strings
are visible, and the removal can be accomplished without difficulty. Such
removal significantly reduces the risk of septic abortion and
reduces the risk of spontaneous abortion. However, women who undergo
early removal still have a higher risk of preterm delivery (i.e., before 37 weeks’ gestation).53 Women with IUDs without visible tail strings who become pregnant have twice
the risk of preterm birth,54,55 but apparently no increased risk for spontaneous abortion. The prevailing
recommendation is to provide women information about early signs and
symptoms of preterm labor and chorioamnionitis, but not to attempt
to remove the IUD in those who desire to continue their pregnancies. Some
investigators have reported small series of ultrasound-guided IUD
removals56 and of hysteroscopic IUD removals57,58 during the first trimester, but these procedures are still considered
experimental. There is no evidence that IUDs increase the risk of congenital anomalies
in children conceived by women using modern IUDs.59 The IUD is generally implanted at the border of the placenta and is physically
separated from the fetus by the amniotic sac. Despite the high
intrauterine concentration of LNG, in the few pregnancies that have
been reported with the LNG-IUS, there is no report of masculinizing effects
on the fetus or of any other unexplained congenital anomalies. The risk of ectopic pregnancy varies by IUD type. Noncontraceptive users
have a background ectopic pregnancy rate of 3.0 per 1000 woman-years. The
copper IUD significantly reduces a woman’s risk for ectopic
pregnancy by a factor of 15, to a rate of 0.2 per 1000 woman-years.60,61 Ectopic pregnancy rates with the LNG-IUS are low. Despite the fact that
the IUDs decrease a woman’s overall risk for ectopic pregnancy, if
a woman does become pregnant while using an IUD, the risk of an
ectopic implantation is approximately 4% to 50% (depending
on the type of IUD). Past use of an IUD does not increase a woman’s
overall subsequent risk for ectopic pregnancy.62,63 However, Bouyer and colleagues64 found that in IUD users who had an ectopic pregnancy, tubal damage, IUD
use for more than 2 years, and a history of problems within the first
month after IUD insertion were associated with higher risk of subsequent
ectopic pregnancy. Expulsion Expulsion rates are highest in the first few months after insertion and
depend on insertion technique and timing of insertion within the menstrual
cycle.34 Overall, first-year expulsion rates with the copper T-380A are 5.7% among
all users and 2.3% among parous women. After the first
year, expulsion rates decline. Walsh and coworkers44 found the expulsion rate after 3 months to be 3.5%. Fewer than 10% of
the expulsions were complete; most were partial expulsions. Many
of these expulsions were clinically silent, so the authors recommended
that a routine follow-up visit be scheduled at 3 months to detect
this problem and to prevent pregnancies. The 5-year expulsion rate
for the LNG-IUS was 5.9%.52 A woman who has expelled one IUD has a 30% chance of expelling
a subsequent IUD.65 The current recommendation is to remove IUDs located in the endocervical
canal and those that are suspected of having relocated lower in the
uterine cavity. If the woman is not pregnant, another IUD can be inserted
immediately. Petta and associates66 concluded that routine ultrasound screening for IUD placement is inappropriate. However, ultrasound can be used to identify the position of
an IUD when dislocation is suspected because of elongated strings, thus
avoiding unnecessary IUD removals. Faundes and colleagues67 noted that IUDs appear on ultrasound to migrate into the correct position
after insertion and move throughout the woman’s cycle, so that
if the T is within 1 to 2 cm of the fundus midcycle, it can be assumed
to be in the correct position.68 Infection Historically, the risk of infection with IUD use has been a significant
concern that resulted in considerable medicolegal activity in the late 1970s
and early 1980s, and ultimately led to the virtual loss of IUDs
in the United States for many years. With a better perspective today, we
can identify the issues relating to serious infection to reduce that
risk. The risk of PID is significantly increased with use of the Dalkon Shield
IUD and with use of any IUD by women at risk for STDs. The risk posed
by the Dalkon Shield was caused by its polyfilament tail, which facilitated
entry of vaginal pathogens into the endometrial cavity by wicking
or capillary action through the interstices between the filaments
in the tail string.69 Modern IUDs, which have monofilament tails, have eliminated this risk; when
monofilament tails are cultured, no growth of either anaerobic or
aerobic organisms is observed. Most studies have shown that IUDs with
monofilament tails pose no higher risk for PID than stringless IUDs.70,71,72,73 Appropriate selection criteria for IUD candidates and thorough screening
for potential infections have significantly reduced the risk of infection
among IUD users. In a study by Farley and associates,74 of 23,000 IUD users worldwide, PID risk was inversely related to age and
number of live births and varied by region. In the Americas, the rates
were the second lowest (1.3/1000 woman-years); China had the lowest
rates, with no reported cases of PID among the 4301 Chinese IUD users. Worldwide, Farley
and coworkers74 noted that PID rates after 1980 were considerably lower than in previous
years. Importantly, Buchan and colleagues75 found no statistically significant increase in the risk of PID in current
users of medicated IUDs or in former IUD users from 1981 to 1989 in
the Oxford–Family Planning Association study. In the United States, Lee
and colleagues76 found that among women with one sexual partner (married or cohabiting), women
who used IUDs had no statistically significant increase in the
incidence of PID compared to those who used no method of birth control. Tsandis
and colleagues77 recently demonstrated that routine culture of removed IUDs and treatment
of women with positive cultures are not recommended in women who are
asymptomatic for PID. In women at low risk for STDs, however, there is still a transient increase
in the risk for PID due to endometrial contamination at the time
of insertion. Older studies reported that an elevated infection risk persisted
for 3 to 4 months after insertion.78 More recently, Farley and colleagues74 re-evaluated their data and found that the increased risk for infection
was limited to the first 20 days after insertion. The latter findings
support the classic observations of Mishell and associates79 that the endometrial cavities of IUD users were contaminated by bacteria
at the time of IUD insertion, but they were sterile 30 days after IUD
insertion except in women who had developed clinical evidence of infection. In international studies, Farley and colleagues74 reported that PID developed at a rate of 9.7 per 1000 woman-years during
the first 20 days after insertion. Many of these women, however, were
not routinely screened for cervical or vaginal infections before insertion. In
more recent studies from developed countries, the incidence
of PID associated with insertion has been reported to be 1 per 1000 woman-years. No
cases of PID were reported in a series of 975 Norwegian
women inserted with IUDs.80 Interestingly, these latter authors tested for infection on the day of
insertion and found that 5 patients tested positive for chlamydia. The
researchers contacted the patients immediately, initiated treatment
within 14 days, no cases of clinical PID developed. In the study by Walsh
and co-workers44 on antibiotic prophylaxis for insertion of IUDs (primarily the copper
T 380A), the absolute incidence of PID in the first 3 months of use was
approximately 1 in 1000. They also found that the incidence of removal
in the first 3 months for reasons other than expulsion, such as increased
bleeding or other possible indications of subclinical infection, was 3.4% to 3.8%. It has been suggested that the rates
of infection could be lower with progestin IUDs. In a randomized multicenter
European trial, the discontinuation rates for PID were significantly
lower in the LNG-IUS users compared to the Nova T users.81,82 However, a study by Sivin and colleagues83 comparing the copper T 380 to the LNG-IUS failed to show any difference
in PID rates by IUD type. If upper genital tract infection develops in an IUD user, she should be
treated following CDC guidelines for PID. Most experts would recommend
IUD removal after a loading dose of antibiotics to reduce risk of septicemia. If
possible, the IUD should be cultured for Actinomyces or its
scraping should be examined for cytologic evidence of that organism. If
infection with Actinomyces is suspected, penicillin should be added
to her antibiotic regimen until the test results are available. Older
studies have suggested that removal of the IUD in women with PID may
not be mandatory, because the severity of the pelvic infection is not
related to the use of an IUD.84 Soderberg and Lindgren85 conducted a small randomized trial of treatment of upper genital tract
infection and found that clinical response as measured by erythrocyte-sedimentation
rate was not changed by removal of the IUD. However, because
of the limited numbers of patients in these older reports, Grimes86 recommends that more evidence is needed to allow routine IUD retention
in a woman with PID. Other Infectious Issues Actinomyces-like organisms are occasionally detected on routine Pap smears. On
careful examination, one study found that the Pap smears of one
third of plastic IUD users had sulfur granules indicative of the presence
of Actinomyces-like organisms, but copper IUD users had much lower
rates of involvement (1% to 6%).87,88,89 On the other hand, Merki-Feld and colleagues90 reported that the Multiload Copper IUD had 20% incidence of Actinomyces-like
organisms in Pap smears compared to 2.9% incidence
reported in LNG-IUS users. The risk of colonization with Actinomyces
increases with the duration of IUD use. If Actinomyces is detected on the Pap smear of an asymptomatic woman with
no signs of upper genital tract disease, it is reasonable to follow
her with routine Pap smears and pelvic examinations. The patient should
be made aware of her colonization and given PID precautions. Some providers
prefer to treat women who have Pap smears suggestive of colonization. Several
approaches are acceptable. Women with cytologic evidence
of colonization may have cervical cultures to confirm the diagnosis
before treatment to reduce the number of women treated, because only 40% of
women with Actinomyces-like organisms found on Pap smears
are actually colonized. In this approach, treatment with oral penicillin
G or tetracycline for 10 to 14 days would be given to those women
who test positive. Others have advised that all asymptomatic women whose
Pap smears demonstrate the presence of Actinomyces-like organisms
be treated with antibiotics and that women whose infections are refractory
to treatment undergo IUD removal. This approach reduces the cost
of testing, but significantly overtreats unaffected women. Routine IUD
removal in the face of cytologic evidence of Actinomyces is not routinely
recommended today. Joesoef and colleagues91 reported that, in a low-risk population, the rate of STDs in IUD users
compared to other methods of contraception were no different, but that
bacterial vaginitis was more common amount IUD users, even after controlling
for age, education, douching practices, and STDs. Menstrual Changes Increased menstrual bleeding, often combined with cramping, is the most
common medical reason for removing IUDs. On average, copper IUDs increase
menstrual flow 35% to 55% above baseline levels, increase
menstrual cramps, and extend the duration of menses by 1 to 2 days
per cycle. In the first few months after insertion, spotting and cramping
can also occur between menses. These changes prompt 5% to 15% of
women to discontinue IUD use. Once partial expulsion
has been ruled out, treatment with NSAIDs is very effective in reducing
these problems.92 NSAIDs should be started at the beginning of menses and continued through
the heavy flow days (usually 3 days). Because of the profound antiproliferative impacts that the LNG-IUS has
on endometrial cells,93 on estrogen and progestin receptors in the endometrium,94 and on the basal lamina,95 virtually every woman who uses the LNG-IUS will experience pronounced
changes in her menstrual cycling. Women should be counseled to expect
more days of spotting and bleeding than bleeding-free days in the early
months of use. However, after 4 to 6 months, women experience significant
reductions in menstrual blood loss. At 12 months, 20% of
women are amenorrheic. The remaining women average 0 to 1 days of bleeding
and 1 to 3 days of spotting per month. Overall, at 1 year, women
experience an 80% reduction in blood loss compared to baseline. Hemoglobin
levels increase and dysmenorrhea decreases at 1 year. Hormonal Side Effects Circulating plasma concentrations of LNG with the LNG-IUS are 150 to 200 pg/mL, which
is only 10% of the peak concentration of 0.75 mg
levonorgestrel-only oral contraceptives and are consistently lower than
those seen with LNG implants. Ovarian steroidogenesis is not impacted; estradiol
levels remain well within normal range for reproductive
aged women, both for amenorrheic LNG users and for those experiencing
menstrual bleeding. Other adverse events, such as mastalgia, headache, acne, nausea, nervousness, abdominal pain, vaginitis, back pain, depression, decreased
libido, abnormal Pap smears, and sinusitis were reported
by at least 5% of women using the LNG-IUS. Most of the hormonally
related events were concentrated in the first 3 months of use. Progestin
slows atresia of ovarian follicles; 12% of women were
diagnosed with persistent functional cysts that generally resolved spontaneously.96 Weight gain attributable to LNG-IUS has not been reported. |