Hormone Therapy ESTROGEN THERAPY Estrogen therapy has many advantages. Recently, however, The National Institute
of Health halted a longitudinal hormone replacement study on
the basis that there was increased risk for heart disease, breast cancer, and
ovarian cancer.43,44,45,46 As a result, patients are now closely involved in the decision-making
process, and it is the responsibility of the physician to thoroughly
discuss the options and risks with patients and help them make informed
decisions. In many instances, a safer and more effective medication could be prescribed
in lieu of HRT, such as raloxifene or a bisphosphonate for bone
demineralization, statins for lipid disorders, and aspirin for coronary heart disease and stroke prevention. It is important to educate
patients about the level of increased risks. A 26% increase
in the risk of breast cancer means that if 10,000 women were using
HRT for 1 year, eight more will have breast cancer.47 The bottom line is that the doctor must help each woman weigh the risks
and benefits of HRT. Estrogen may relieve hot flashes, improve clitoral
sensitivity, increase libido, and decrease pain and burning during
intercourse. Local or topical estrogen application relieves symptoms of
vaginal dryness, burning, and urinary frequency/urgency. In perimenopausal, menopausal, or
oophorectomized women, reports of vaginal irritation, pain, or
dryness may be relieved locally with low-dose
topical estrogen cream, vaginal estradiol rings, or vaginal estradiol pellets, which may help to minimize the risks of estrogen. TESTOSTERONE The only FDA-approved testosterone replacement available to women is methyltestosterone, indicated for menopausal
women, used in combination with estrogen (Estratest), for
symptoms of inhibited desire, dyspareunia, or lack of vaginal lubrication, as
well as for its vasoprotective effects. A testosterone patch is presently being tested, and early trials indicate that the patch
may improve sexual activity and help create overall sense of well
being.48 According to the Princeton Consensus Panel on Female Androgen Insufficiency, if
a woman exhibits symptoms of low testosterone (e.g., low libido and decreased energy and well-being), it
is important to first determine an alternative explanation for these
symptoms. This means ruling out major depression, chronic fatigue
symptoms, and the range of other emotional and relationship conflicts
that may impact on a patient's desire and happiness. The next step
is to determine if the patient is in an adequate estrogen state and, if
not, to consider the pros and cons of replacement.49 The physician should measure the patient's testosterone levels, which should include at least two to three measures of total and
free testosterone. Normal value range for total testosterone is 49 to120 ng/dL, and for free testosterone it is 3.0 to 8.5 pg/mL for premenopausal women. Normal value range
for total testosterone for postmenopausal women is 3.0 to 6.7 pg/mL. If the patient has a
treatable cause for the androgen deficiency (e.g., oral estrogens
or contraceptive use), treat the specific causes by changing medications. If
not, consider a trial of androgen replacement therapy. There are conflicting reports regarding the best way to use testosterone, in
particular, in premenopausal women. Any premenopausal woman treated
with testosterone must be on some form of reliable birth control and understand the risks. Topical
vaginal testosterone is often used in premenopausal women as a first step because it is delivered
locally and is also used for treatment of vaginal lichen planus. Topical testosterone (methyltestosterone or testosterone propionate) preparations can be compounded in 1% to 2% formulations
and should be applied up to three times per week. The
suggested dose of oral testosterone (pill or sublingual spray or lozenge) for premenopausal and
postmenopausal women range from .25 to 1.25 mg/day. The dose should
be adjusted according to symptoms, free testosterone levels, cholesterol levels, triglyceride levels, HDL levels, and LFT. The
potential side effects of testosterone include weight gain, clitoral enlargement, increased facial hair, and
hypercholesterolemia. Testosterone can also be converted into estrogen, so
physicians should take this risk into account when counseling their
patients. Increased clitoral sensitivity, decreased vaginal dryness, and
increased libido have been reported with the use of a 2% testosterone cream. Preliminary studies on the effectiveness of dehydroepiandrosterone (DHEA) as
a form of testosterone replacement are promising as well.50 Pharmacological Therapy Aside from hormone replacement therapy, all medications listed here, although
used in the treatment of male erectile dysfunction, are still in
the experimental phases for use in women. Currently, we have limited
information regarding the exact neurotransmitters that modulate vaginal
and clitoral smooth muscle tone. Recently, nitric oxide (NO) and
phosphodiesterase type 5 (PDE5), the enzyme responsible
for both the degradation of cGMP and NO production, have been identified
in clitoral and vaginal smooth muscle.2 In addition, organ bath studies of rabbit clitoral cavernosal muscle strips
demonstrate enhanced relaxation in response to the nitric oxide
donors, sodium nitroprusside, L-arginine, and sildenafil. SILDENAFIL Functioning as a selective type 5 (cGMP specific) phosphodiesterase
inhibitor, sildenafil decreases the catabolism of cGMP, which is
the second messenger in nitric oxide-mediated relaxation of clitoral
and vaginal smooth muscle. Sildenafil may prove useful alone or
possibly in combination with other vasoactive substances for treatment
of female sexual arousal disorder. Phase two clinical studies assessing
safety and efficacy of this medication for use in women are currently
in progress. A recent study demonstrated that sildenafil is successful
in treating female sexual arousal disorder in hormonally replete
women without psychosexual causal factors in a placebo-controlled
study.51,52 Other studies have found that sildenafil helps to alleviate arousal problems
associated with aging and menopause and secondary to SSRI use.30,32 L-ARGININE This amino acid functions as a precursor to the formation of nitric oxide, which
mediates the relaxation of vascular and nonvascular smooth muscle. L-arginine
has not been used in clinical trials in women. However, preliminary
studies in men appear promising. A combination
of L-arginine and yohimbine (an alpha-2 blocker) is
currently undergoing investigation in women. YOHIMBINE Yohimbine is an alkaloid agent that blocks presynaptic alpha-2 adrenoreceptors. This
medication affects the peripheral autonomic nervous
system, resulting in a relative decrease in adrenergic activity and
an increase in parasympathetic tone. There have been mixed reports of
its efficacy for inducing penile erections in men, and no formal clinical
studies have been performed in women to date, nor have potential
side effects been effectively determined. PROSTAGLANDIN E1 (MUSE) An intraurethral application, absorbed via mucosa (MUSE), is
now available for male patients. A similar application of prostaglandin
E1 delivered intravaginally is currently undergoing investigation for use
in women. Clinical studies are necessary to determine the efficacy of
this medication in the treatment of female sexual dysfunction. PHENTOLAMINE Currently available in an oral preparation, this drug functions as a nonspecific
alpha-adrenergic blocker and causes vascular smooth muscle
relaxation. This drug has been studied in male patients for the
treatment of erectile dysfunction. A pilot study in menopausal women with
sexual dysfunction demonstrated enhanced vaginal blood flow and subjective
arousal with the medication.53 APOMORPHINE Apomorphine is a short-acting dopamine agonist that facilitates
erectile responses in normal males and males with psychogenic erectile
dysfunction or organic impotence. Data suggest that dopamine is involved
in the mediation of sexual desire and arousal. The physiologic effects
of this drug are currently being tested in women with sexual dysfunction. NITROGLYCERIN Nitroglycerin (glyceryl trinitrate) has been used for more than
a century to relieve anginal symptoms associated with coronary artery
disease. It has been administered to humans via oral, sublingual, intravenous, and
transdermal routes. Nitroglycerin has been found to relax
most smooth muscle, including bronchial, gastrointestinal tract, urethral, and
uterine muscle. It also produces dilation of both arterial
and venous vascular beds. Metabolism of nitroglycerin leads to the formation of the reactive free radical nitric oxide. Recent
evidence suggest that application of nitroglycerin to painful areas, including the genitals, may provide analgesia to the
affected areas.23,54 More work needs to be performed in this area, but many experts are finding
this to be an effective treatment for helping women manage vulvar
pain, especially when in combination with topical estrogen and testosterone creams and vaginal physical therapy. Medical Devices EROS-CTD Eros-CTD is the first FDA-approved treatment on the market
for arousal and orgasmic disorders in women. It is a small, hand-held
medical device that works by applying a genital vacuum to the
clitoris, increasing blood flow to the clitoris and surrounding tissue. Initial
clinical trials showed improvement in premenopausal and postmenopausal
women with female sexual arousal disorder or female orgasmic
disorder.55,56 INTERSTIM THERAPY InterStim therapy was designed to treat urinary incontinence. The therapy
involves placing a lead in the S-2 to S-4 region. The
lead is passed to a neurostimulator, which sends mild electrical pulses
to the sacral nerve. Many women who have undergone this procedure have
anecdotally reported that their sexual arousal and ability to achieve
orgasm increased. More retrospective and prospective research testing
this device for orgasmic improvement is currently underway. Other Therapies GYNECOLOGIC PHYSICAL THERAPY Pelvic pain, vaginismus, and vaginal atrophy can often be treated with
physical therapy. When muscle tension or spasm appears to be a factor, a
physical therapist, through gentle massage, biofeedback, or other techniques, can
help restore normal muscle balance. Physical therapy can
also be helpful for women who have vaginal, rectal, or uterine prolapse, and
can be helpful to those women with incontinence and weak Kegel
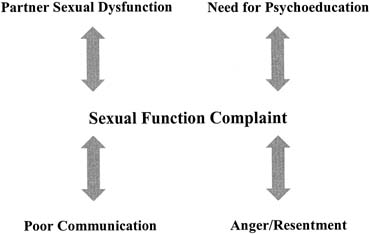
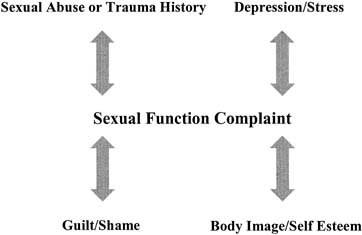
muscles. TALK THERAPY More often than not, there are psychological and relationship factors contributing
to a sexual problem. Even if the primary etiologic domain
is physical, there are emotional and relationship outgrowths to the problem
that cannot be ignored. Similarly, not all women are candidates
for medical intervention and are better suited for other psychological
or couples therapies.19,56,57 Usually the best treatment is a combination of medical and talk therapy. It
should be noted here that beginning talk therapy without evaluating
the potential medical causes for female sexual dysfunction is not
recommended. Extensive talk therapy with a woman with undiagnosed medical
issues can be a frustrating experience for the patient and caregiver. The ideal way to determine candidates for medical intervention in a clinical
setting is to collaborate with a trained sex therapist. If the medical
practitioner has access to a therapist on site, evaluation and
diagnosis are optimized. Unfortunately, not all physicians have access
to or facilities for incorporating a sex therapist into their practice. In
this case, it is crucial for the physician to perform an extensive
assessment of the sexual symptoms and the context in which they are
experienced. This process not only entails a good global history but
also includes clarification of the sexual concern in a way that allows
psychosexual “red flags” to be identified so that an appropriate
therapy referral can be made (Table 4). Table 4. Psychosexual Red Flags for Further Assessment*
| The symptoms are life-long, not acquired |
| The symptoms are situational (e.g. do not exist when stress removed
or when with another partner) |
| The patient has a history of sexual abuse or trauma |
| The patient has a psychiatric history |
| The patient has a history of or is presently experiencing depression and/or
anxiety or stress |
| The couple experiences relationship conflicts (e.g. lack of intimacy, conflict, etc.) |
| The partner has a sexual dysfunction |
*None of these factors guarantee the problem is psychosexually based
but simply point to a need for further clarification by a trained sex
therapist.
The key to making a therapy referral is helping the patient understand
how talk therapy fits into the treatment equation. It may need to be clarified
that although you do not think her problems are “all in
her head,” she would benefit from talk therapy as well as medical
treatment. Often if the physician supports the role of talk therapy
and helps the patient understand how it will be incorporated into her
treatment plan, rather than feeling “pawned off” to someone
else, she will feel validated and encouraged. Even if the physician
refers the patient to a sex therapist, if it is discussed as part of
the treatment plan, the patient will usually respond positively. |