Contemporary Use of the Pessary
Authors
INTRODUCTION
Pelvic organ prolapse and urinary incontinence are common and distressing conditions. About 200,000 women each year undergo surgery for pelvic organ prolapse.1 Urinary incontinence is more common among women than men. In fact, 9–39% of women over the age of 60 report 'daily urinary incontinence'.2 These disorders are also associated with significant impairments in quality of life3, 4 as well as depression.5 The management of prolapse and incontinence is varied and encompasses a wide range of treatment options. While some women desire definitive surgical management, others opt for more conservative measures. These women, along with those whose medical comorbidities confer a significant risk of surgical morbidity, may benefit most from more conservative therapies including pessaries. In this chapter, the development of pessaries, the types of device in common use, and their indications, management, complications, and contraindications are discussed.
HISTORY
The Egyptians were the first to describe pelvic organ prolapse, and the pessary was a known treatment.6 The word pessary frequently appears in both Greek and Latin literature, but in most instances it refers to a mechanical device in no way like the modern one. For example, Hippocrates mentioned the use of half a pomegranate introduced into the vagina in instances of prolapse. Soranus likewise suggested the use of this fruit as a pessary and reported that Diocles was in the habit of supporting a prolapsed uterus by the introduction of half a pomegranate previously treated with vinegar.7 Aurelius Cornelius Celsus (27BC–AD50) wrote of the use of pessaries in De Medicina.8 A bronze cone-shaped vaginal pessary with a perforated circular plate at its widest end was found at Pompeii. Supposedly, a band was attached to these openings and tied around the body to keep the device in place.7
Around AD1050, Trotula, the wife of Joannes Platearious, was the first recorded female practitioner of gynecology. She originated the use of a ball pessary that was made of strips of linen and filled the vagina in cases of prolapse.6 Caspar Stromayr of Lindau, Germany, recommended in 1559 that a sponge tightly rolled and bound with string, dipped in wax, and covered with oil or butter be substituted for a pomegranate as a pessary9 (Figs. 1 and 2).
|
|
Ambrose Pare, late in the 16th century, devised oval-shaped pessaries of hammered brass and waxed cork for uterine prolapse. He made an apparatus of gold, silver, or brass that was kept in place by a belt around the waist. He also designed pear-shaped and ring pessaries10 (Fig. 3).
|
Hendrik Van Roonhuyse, born in 1622, made a remarkable contribution to 17th century gynecology when in 1663 he published Heelkonstige Aanmerkkingen Betreffende de Grebrecken der Vrouwen. This book often has been referred to as the first textbook on operative gynecology. Van Roonhuyse discussed the etiology and treatment of prolapse. An accepted procedure for treatment of prolapse was the use of cork with a hole in it to allow passage of discharges, plus wax pessaries or cork dipped in wax.
Goodyear's discovery of the vulcanization of rubber was a boon to the purveyors and wearers of pessaries and greatly enhanced the popularity of the devices. Hugh Lenox Hodge, Professor of Gynecology at the University of Pennsylvania, was dissatisfied with the shapes of the existing pessaries. He set out to design a new one using Goodyear's newly patented material. The lever pessary was designed especially for cases of uterine retroversion. Hodge explained in 1860:
The important modification consists in making a ring oblong, instead of circular, and curved so as to correspond to the curvature of the vagina. Great advantages result from this form; the convexity of the curve being in contact with the posterior wall of the vagina, corresponds, with more or less accuracy, to properly arrange, there is no pressure against the rectum; and the higher the instrument rises, the superior extremity, instead of impinging against the rectum, passes upward and behind the uterus—between this organ and the intestine—giving a proper position to the womb, and yet allowing its natural pendulum-like motion to remain unrestrained.11, 12 (Fig. 4)
Albert Smith of Philadelphia later narrowed the anterior portion and widened the posterior end of the Hodge pessary.13
The most significant advance in the art and science of pessaries was the replacement of hard rubber with polystyrene plastics in the 1950s and recently by silicone-based materials.14
DEVICES
A variety of pessaries can be used to successfully manage pelvic organ prolapse. The ultimate goal of a pessary is that of prolapse reduction, which can be achieved by either supporting the prolapse with an appropriate pessary or filling the vagina with a space-occupying pessary.15 Many studies have shown that increased support and reduction of the prolapse ultimately allows for symptomatic relief and improved quality of life.16, 17, 18 Currently available pessaries are generally made of silicone and thus are very well tolerated. They are non-allergenic, durable, autoclavable, and generally easy to remove and replace. The choice of pessary depends on a variety of factors including type and degree of prolapse (e.g. anterior compartment, apical, uterovaginal), the type of pessary the clinician has available (i.e. one pessary for all), and whether the patient desires to manage her pessary at home, as some pessaries cannot be self-removed.
Support pessaries
RING PESSARIES
In a survey of the members of the American Urogynecologic Society, the most common pessaries utilized included the ring, Gellhorn, and donut.19 The ring pessary is similar in its appearance to a contraceptive diaphragm (Fig. 5I and 5J). It is useful in supporting milder forms of prolapse (stage I and II) of all compartments (cystoceles, uterovaginal, vaginal vault) as well as treating stress urinary incontinence. The advantages of the ring pessary include ease of insertion and removal by both the physician and the patient. The ability of the patient to remove and replace the pessary on her own also makes coitus possible. This pessary is fitted very similarly to a contraceptive diaphragm. It is folded such that the arc points downward and is directed past the cervix into the posterior fornix; the anterior aspect rests against the posterior aspect of the pubic symphysis.
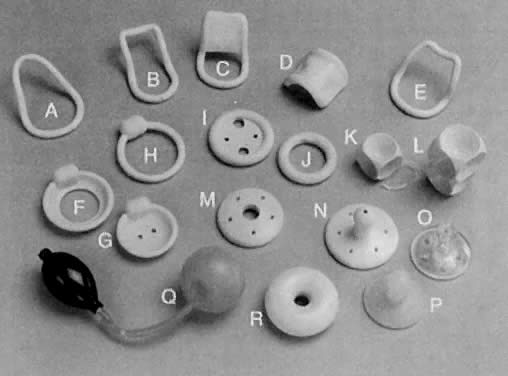
Lever pessaries are variations on the design by Hodge and include the Smith and Risser pessaries.11 They were initially intended to treat uterine retroversion by posteriorly displacing the cervix and anteverting the uterus.14, 20 The Smith pessary has a narrower anterior limb for application in a patient with a narrow pubic arch (Fig. 5A). The somewhat broader anterior limb of the Hodge pessary prevents the pessary from turning and precludes pressure on the urethra (Fig. 5B and 5C). The Risser pessary is a further modification, for an even flatter pubic arch21 (Fig. 5E). These pessaries are rarely used now. The pessary is inserted by first manually elevating a retrodisplaced uterus. The pessary is then folded and pushed into the vagina by the index finger, pressing on the posterior bar until it is behind the cervix, with the anterior bar behind the pubic notch22 (Fig. 6). This pessary (Fig. 5D) is designed to treat cystoceles and rectoceles. SHAATZ PESSARY This pessary (Fig. 5M) is very similar to a Gellhorn pessary (see below) and can be used for uterine and vaginal vault prolapse. Space-filling pessaries GELLHORN PESSARY The Gellhorn pessary (Fig. 5N, 5L, 5M, 5N, 5O, and 5P)23 provides both support of prolapse and occupation of space. Thus, it is very suitable for treatment of stage III and IV prolapse. The cervix or more apical part of the prolapse (if the patient has had a hysterectomy) rests behind the wide, concave surface of pessary which allows for some suction to form against the vagina as well. The stem prevents turning the support within the vagina and points towards the posterior vagina and introitus. It requires a relatively capacious vagina so that the base is broad enough to rest above the levators. It is inserted by turning the disk portion obliquely; then the base is rotated over the perineal body and into position24 (Fig. 7). In order to remove the device, the stem is grasped (either manually or with the aid of a clamp such as a ring forceps) and suction broken by inserting another finger in a sweeping motion around the base. Unlike the ring pessary, which functions by lifting up or supporting various compartmental prolapses, the donut and inflatoball pessaries work more as space occupiers. The donut is made of silicone, and the inflatoball of latex. These bulkier pessaries (Fig. 5Q and Fig. 5R), not surprisingly, work better for more severe stages of prolapse (stage III and IV), especially those where the uterus is still in situ. They can also be used to reduce bothersome rectoceles, which are generally not amenable to pessaries that support anterior and apical prolapse. Similarly, given their girths, they can often be useful in reducing prolapse in a patient with a large genital hiatus. Also, because of the shape and size, these pessaries are more difficult to remove, especially by the patient. Thus, in a patient who is sexually active, donuts and inflatoball pessaries are not an ideal choice. One advantage of the inflatoball is that it can be insufflated once it is in situ, thus making insertion more comfortable for some patients. CUBE PESSARY As a last resort in a very select group of patients, the cube pessary (Fig. 5K) can be effective. This pessary has six suction cups that adhere to the vaginal epithelium. Thus, in a patient who is unable to retain any other pessary (e.g. prolapse too large, genital hiatus too widened), the cube provides an alternative. Unfortunately, the design of the suction cups predisposes the vagina to ulcerations as well as to development of a bothersome vaginal discharge. This mandates close out-patient follow-up. It is also impossible for the patient to remove this pessary on her own, thus coitus is not possible. It is inserted by merely compressing the cube and placing it as high up in the vagina as possible. In order to remove the device, it must be grasped and the suction broken between it and the vaginal epithelium. INCONTINENCE PESSARIES A few pessaries are available for the treatment of stress urinary incontinence (Fig. 5F, 5G, and 5H). These pessaries are inserted such that the urethra is compressed against the pubic symphysis. This allows for an increase in urethral resistance as intrabdominal pressure rises (i.e. with laughing, lifting, coughing), thus preventing leakage of urine.
LEVER PESSARIES
GEHRUNG PESSARY
DONUT/INFLATOBALL PESSARIES
INDICATIONS
Relief of prolapse symptoms
The most common application of a pessary is that of relieving the symptoms associated with pelvic organ prolapse in women who desire non-surgical therapy, those who are poor surgical candidates, and those who have not completed childbearing. Symptoms most commonly associated with pelvic organ prolapse include a bothersome sensation of a vaginal bulge, difficulty emptying the bladder and/or rectum with a need to push on the vaginal walls or perineum to facilitate emptying, urinary leakage, and sexual dysfuntion.25, 26, 27 Most studies have shown that prolapse symptoms result in significant bother in women;28, 29 thus, reduction of prolapse with a pessary can effectively alleviate this bother.
Preoperative diagnostic aid in patient with pelvic organ prolapse
Pessaries can be used as a diagnostic aid in a variety of preoperative situations. For example, if a patient complains of a symptom not commonly associated with prolapse (i.e. pelvic pain), placement of a pessary may reveal whether reduction of the prolapse alleviates that pain. Similarly, in patients with anterior or apical vaginal prolapse, reduction of the prolapse preoperatively with a pessary can often unmask urinary incontinence. These patients will complain of new-onset urinary leakage with various activities including laughing, coughing, and sneezing. If this occurs, an anti-incontinence procedure at the time of prolapse surgery may be indicated.30 In patients with significant anterior vaginal prolapse, urinary retention can occur concurrently. In a study by Lazarou et al., 75% of women normalized their postvoid residual volume to less than 100 ml after a pessary was placed; this was highly predictive of postoperative resolution of urinary retention.31
Preoperative preparation
In some patients who ultimately desire definitive management of their prolapse, surgery may need to be delayed for various reasons. A pessary can be a very useful temporizing measure. For example, in a patient with procidentia, ulcers may develop on the most dependent part of the prolapse. The ulceration and inflammation can compromise tissue planes intraoperatively and can also increase the risk of infection and impair healing postoperatively. Reduction of the prolapse with an appropriately fitted pessary along with topical estrogens (in patients without contraindications to hormonal therapy) allows the inflammation to subside and ulcers to heal. This promotes maturation of the vaginal epithelium, and subjectively improves surgical planes. Rarely, uterovaginal prolapse causes ureteral obstruction and hydronephrosis. Pessary application has been shown to relieve obstruction and improve renal function so that patients can undergo surgical correction.32, 33, 34
Stress urinary incontinence
In patients with stress or mixed urinary incontinence, pessary use can be an alterative to surgical management.35 Specifically, pessaries such as the incontinence dish or a ring with a knob can provide the urethrovesical junction the support that is lacking in these patients. In the Ambulatory Treatment for Leakage Associated with Stress Incontinence (ATLAS) study, 446 women with stress urinary incontinence were randomized to three treatment groups: pessary, behavior therapy (pelvic floor muscle training), or both pessary and behavioral therapy. At 3 months, 49% of women in the behavioral group reported having no bothersome incontinence symptoms; this was significantly more than the pessary group (33%, p=0.006). Similarly, combination therapy was better than pessary alone. At 12 months, however, there were no differences between the groups and more than 50% of all the women in each group remained satisfied.36
Incarcerated uterus
Retrodisplacement of the uterus in early pregnancy occurs in about 15% of pregnancies. It almost always is self-limited because the enlarging uterus rises into the abdomen. Incarceration occurs rarely when a retroverted pregnant uterus becomes entrapped in the sacral hollow, probably as a result of adhesions or endometriosis. The uterus presses against the rectum and fails to rise into the abdomen as it enlarges. Patients present after 12 weeks of gestation with pain and urinary and rectal complaints. Examination shows a posterior cul-de-sac mass with the cervix rotated anteriorly high up in the vagina behind the pubic symphysis, impinging on the bladder trigone.37 Gibbons and Paley reported that patients who were treated with uterine repositioning and pessary support before 15 weeks did well, but that those beyond that gestation aborted despite treatment.38 The appropriate lever pessary, typically the Hodge, displaces the cervix posteriorly, anteverting the uterus and allowing it to rise out of the pelvis (see Fig. 4). It has been used successfully to treat mobilized incarceration and to prevent recurrences in subsequent pregnancies.38, 39
Incompetent cervix with premature labor
The use of the pessary as a nonsurgical alternative to cervical cerclage has been reported in the past, however, it is generally no longer practiced in the US. Cross, of the Rotunda Hospital in Dublin, was the first to report the use of Bakelite ring pessaries in 13 patients with a history of only seven term deliveries in 54 pregnancies (13%) before treatment. After application of the pessary, the patients delivered 11 of 13 viable infants (85%).40 In the US, Vitsky studied 21 patients with a pregnancy history of only 23% viable deliveries; this improved to 87% with the use of a Smith pessary.41, 42, 43 In the US, the Hodge pessary has been used successfully to treat cervical incompetence owing to defective connective tissue in Ehlers-Danlos syndrome.44 The incompetent cervix points anteriorly in the axis of the vagina (Fig. 8). The lever pessary directs the cervix to point posteriorly, as in a normal pregnancy. Direct pressure on the cervical os is reduced and brought to bear on the lower uterine segment.45 A randomized prospective placebo-controlled study evaluating pessaries for the treatment of the incompetent cervical os has yet to be accomplished.
MANAGEMENT
Selecting a pessary
Selecting the most appropriate pessary requires an understanding of the devices and their indications. However, the pessary should be fitted to the patient. Different devices often are used to treat the same process in different patients. In a survey of members of the American Urogynecologic Society, it was found that most responders chose the type of pessary to be fitted based on the support defect found in the patient.46 In general, anterior defects tend to be best managed with ring or lever pessaries. Similarly, mild to moderate prolapses of the uterus or vaginal vault can also be treated with ring pessaries. More severe uterovaginal and vaginal vault prolapse is best treated with a space occupying pessary such as a Gellhorn, donut or cube; as these pessaries generally cannot be removed by the patient, if she is sexually active, a ring or other device (which patients can remove) should be tried first.
Fitting a pessary
In general, the largest pessary that a patient can comfortably accommodate should be fitted. Often, fitting a pessary involves trial and error, as measures of genital hiatus and total vaginal length have not been found to be helpful in sizing.47 Ring and lever pessaries should fit snugly behind the pubic symphysis and posterior to the cervix. As when fitting a contraceptive diaphragm, the examiner's finger should easily pass between the vagina and the circumference of the pessary. After the pessary has been inserted, the labia should be separated and the patient should perform a Valsalva maneuver. A properly fitted pessary descends to where the lower bar is visible and then ascends with relaxation.21 The patient should be able to stand, sit, squat, urinate, and defecate comfortably without dislodging the device. Coitus is possible with the ring, lever, and Gehrung pessaries in place.21, 48, 49
Follow-up
Physicians must consider a patient as being under their active care as long as she wears the device. The patient and her family should be instructed about the management plan with the pessary. After placement of the pessary, the patient should return in 1–2 weeks for re-evaluation consisting of palpation of the pessary in place, removing it, carefully inspecting the vagina for excoriations, lacerations, or ulcerations, cleaning and inspecting the pessary, and ultimately replacing it if appropriate. If the patient cannot remove the pessary on her own, after this initial visit, she should be seen every 3–6 months for examination. In patients who self-manage their pessaries, the frequency of removal can be based on their preference; some patients opt to remove pessaries every night, while others leave it in situ for several weeks or months.
COMPLICATIONS
The most common complaint of patients wearing pessaries is an increase in vaginal discharge and odor. One study found that pessaries can increase the risk of bacterial vaginosis.50 If the patient is symptomatic and bothered by the discharge, the bacterial vaginosis may be treated. As many patients who are fitted with a pessary have concurrent vaginal atrophy, vaginal estrogen is often prescribed as well in order to decrease the potential rate of vaginal ulceration. Generally, using 0.5–1 g of intravaginal estrogen daily for 2 weeks followed by maintenance therapy 2–3 times a week is recommended. In women who are not candidates for estrogen therapy, Trimo-San vaginal cream (MilexTM, Cooper Surgical, Trumbull, CT, USA) can be used instead. Sometimes, if ulceration occurs even in the setting of vaginal estrogen use, a pessary 'holiday' for 2 weeks with subsequent re-examination and possible reinsertion of the pessary (if the vaginal epithelium has healed) is necessary. Complications such as spontaneous pessary expulsion and difficulty with defecation can be easily managed by changing the type and size of pessary used; with expulsion, a larger pessary may be necessary, while difficulty with defecation can signal that a smaller or less space-occupying pessary is in order. If de novo stress urinary incontinence develops with prolapse reduction, one can consider placement of an incontinence ring or dish pessary to increase support of the urethrovesical junction.
If pessaries are neglected and remain in situ for long periods of time (generally more than 4 months), serious complications can occur. General anesthesia and surgical procedures have been required to remove embedded pessaries.51, 52, 53, 54, 55, 56 Incarceration can occur when the cervix and uterus or intestines herniate through the center of a poorly fitted ring pessary and become strangulated.57, 56 Patients with embedded or incarcerated pessaries sometimes can have them removed on an outpatient basis, using improved vaginal hygienic measures and topical estrogens to mature epithelium and diminish inflammation.58 Surprisingly, fistula formation secondary to pessary use is quite unusual.7, 52, 56, 59, 60
CONTRAINDICATIONS
The contraindications to pessary placement include primary vaginitis, active pelvic inflammatory disease, latex sensitivity (if an inflatoball pessary is going to be utilized), a noncompliant patient, and lack of assured follow-up.
REFERENCES
Boyles SH, Weber AM, Meyn L: Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol. 2003 Jan;188(1):108-15. |
|
Buckley BS, Lapitan MC: Prevalence of Urinary Incontinence in Men, Women, and Children-Current Evidence:Findings of the Fourth International Consultation on Incontinence.factors of urinary incontinence in order to provide a concise reference sourcefor clinicians, health researchers, and service planners. Urology. 2010 Aug;76(2):270-1. |
|
Jelovsek JE, Barber MD: Women seeking treatment for advanced pelvic organ prolapse have decreased bodyimage and quality of life. Am J Obstet Gynecol. 2006 May;194(5):1455-61. |
|
Coyne KS, Zhou Z, Thompson C et al: The impact on health-related quality of life of stress, urge and mixed urinaryincontinence. BJU Int. 2003 Nov;92(7):731-5. |
|
Melville JL, Delaney K, Newton K et al: Incontinence severity and major depression in incontinent women. Obstet Gynecol. 2005 Sep;106(3):585-92. |
|
Morice P, Josset P, Colau JC: Gynecology and obstetrics in ancient Egypt. J Gynecol Obstet Biol Reprod (Paris) 23: 131, 1994 |
|
Ricci JV: Genealogy of Gynecology, p. 350. Philadelphia, Blakiston, 1950 |
|
Cianfrani T: Short History of Obstetrics and Gynecology. Springfield, IL, Charles C. Thomas, 1960 |
|
Stromayr C: Die Handschrift des Schnitt-und Augenarztes Caspar Stromayr. Berlin, Brunn, 1925 |
|
Emge LA, Durfee RB: Pelvic organ prolapse, four thousand years of treatment. Clin Obstet Gynecol 9: 997, 1966 |
|
Hodge HL: On Disease Peculiar to Women, Including Displacements of the Uterus. Philadelphia, Blanchard & Lea, 1860 |
|
Speert H: Obstetrics and Gynecologic Milestones. New York, Macmillan, 1958 |
|
Speert H: Obstetrics and Gynecology in America: A History. Baltimore, Waverly Press, 1980 |
|
Robertson DNS, Stoff FD: Advantages of “polythene” ring pessaries. Br Med J 2: 30, 1958 |
|
Trowbridge ER, Fenner DE: Practicalities and pitfalls of pessaries in older women. Clin Obstet Gynecol. 2007 Sep;50(3):709-19. |
|
Patel M, Mellen C, O'Sullivan DM et al: Impact of pessary use on prolapse symptoms, quality of life, and body image. Am J Obstet Gynecol. 2010 May;202(5):499.e1-4. Epub 2010 Feb 20. |
|
Fernando RJ, Thakar R, Sultan AH et al: Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006 Jul;108(1):93-9. |
|
Clemons JL, Aguilar VC, Tillinghast TA et al: Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2004 Apr;190(4):1025-9. |
|
Cundiff GW, Weidner AC, Visco AG et al: A survey of pessary use by members of the American urogynecologic society. Obstet Gynecol. 2000 Jun;95(6 Pt 1):931-5. |
|
Smith AA: A golden opportunity. J Med Assoc GA 53: 349, 1964 |
|
Risser JA: Symptomatic Descensus Uteri (Prolapse Syndrome). Chicago, Milex Products, 1957 |
|
Crossen RJ: Disease of Women, 10th ed. St. Louis, CV Mosby, 1953 |
|
Sulak PJ, Kuehl TJ, Shull BL: Vaginal pessaries and their use in pelvic relaxation. J Reprod Med 38: 919, 1993 |
|
Gellhorn G: A new pessary for the treatment of inoperable prolapse of the uterus. Am J Obstet Gynecol 29: 737, 1935 |
|
Ghetti C, Gregory WT, Edwards SR et al: Pelvic organ descent and symptoms of pelvic floor disorders. Am J Obstet Gynecol. 2005 Jul;193(1):53-7. |
|
Gustilo-Ashby AM, Paraiso MF, Jelovsek JE et al: Bowel symptoms 1 year after surgery for prolapse: further analysis of arandomized trial of rectocele repair. Am J Obstet Gynecol. 2007 Jul;197(1):76.e1-5. |
|
Pauls RN, Segal JL, Silva WA et al: Sexual function in patients presenting to a urogynecology practice. Int Urogynecol J Pelvic Floor Dysfunct. 2006 Nov;17(6):576-80. |
|
Ellerkmann RM, Cundiff GW, Melick CF et al: Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001 Dec;185(6):1332-7; discussion 1337-8. |
|
Rortveit G, Brown JS, Thom DH et al: Symptomatic pelvic organ prolapse: prevalence and risk factors in a Obstet Gynecol. 2007 Jun;109(6):1396-403. |
|
Liang CC, Chang YL, Chang SD et al: Pessary test to predict postoperative urinary incontinence in women undergoing hysterectomy for prolapse. Obstet Gynecol. 2004 Oct;104(4):795-800. |
|
Lazarou G, Scotti RJ, Mikhail MS et al: Pessary reduction and postoperative cure of retention in women with anteriorvaginal wall prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2004 May-Jun;15(3):175-8. Epub 2004 Feb |
|
Hildreth TA, Stewart W, Cass AS: Uterine prolapse and upper urinary tract obstruction. Minn Med 59: 450, 1976 |
|
Jurascheck J, Salti A, Fernandex R et al: Bladder retention and blockage of urinary tract caused by prolapse. Acta Urol Belg 54: 391, 1986 |
|
Jay GD, Kinkead T, Hopkins T, Wollin M: Obstructive uropathy from uterine prolapse: a preventable problem in the elderly. J Am Geriatr Soc 40: 1156, 1992 |
|
Donnelly MJ, Powell-Morgan S, Olsen AL et al: Vaginal pessaries for the management of stress and mixed urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004 Sep-Oct;15(5):302-7. Epub 2004 Aug |
|
Richter HE, Burgio KL, Brubaker L et al: Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010 Mar;115(3):609-17. |
|
Weinberger MW, Julian TM: Voiding dysfunction and incontinence caused by uterine retroversion: A case report. J Reprod Med 40: 387, 1995 |
|
Gibbons JM Jr, Paley WB: The incarcerated gravid uterus. Obstet Gynecol 33: 842, 1969 |
|
McGann KP, Griffin WT: Recurrent classical sacculation of the pregnant uterus. J Fam Pract 26: 339, 1988 |
|
Cross RG: Treatment of habitual abortion due to cervical incompetence. Lancet 2: 127, 1959 |
|
Vitsky M: Simple treatment of the incompetent cervical os. Am J Obstet Gynecol 81: 1194, 1961 |
|
Vitsky M: The incompetent cervical os and the pessary. Am J Obstet Gynecol 87: 144, 1963 |
|
Vitsky M: Pessary treatment of the incompetent cervical os. Obstet Gynecol 31: 732, 1968 |
|
Leduc L, Wasserstrum N: Successful treatment with the Smith-Hodge pessary of cervical incompetence due to defective connective tissue in Ehlers-Danlos syndrome. Am J Perinatol 9: 25, 1992 |
|
Javert CT: Further follow-up on habitual abortion patients. Am J Obstet Gynecol 84: 1149, 1962 |
|
Cundiff GW, Weidner AC, Visco AG et al: A survey of pessary use by members of the American urogynecologic society. Obstet Gynecol. 2000 Jun;95(6 Pt 1):931-5. |
|
Nager CW, Richter HE, Nygaard I et al: Incontinence pessaries: size, POPQ measures, and successful fitting. Int Urogynecol J Pelvic Floor Dysfunct. 2009 Sep;20(9):1023-8. Epub 2009 Jun 16. |
|
Melody GF: The use and abuse of pessaries. West J Surg 55: 544, 1947 |
|
Colmer WM: Use of the pessary. Am J Obstet Gynecol 65: 170, 1953 |
|
Alnaif B, Drutz HP: Bacterial vaginosis increases in pessary users. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(4):219-22; discussion 222-3. |
|
Pommerenke WT: The neglected pessary. Obstet Gynecol 1: 226, 1953 |
|
Russell JK: The dangerous vaginal pessary. Br Med J 2: 1595, 1961 |
|
Pritchard JG: A watchspring pessary retained for 62 years. Lancet 1: 172, 1961 |
|
Thornton CA, Harrison RF: Brief report: Unusually rapid incarceration of a polyvinyl ring pessary. Ir J Med Sci 146: 116, 1977 |
|
Sivasuriya M: Cervical entrapment of a polythene vaginal ring pessary—A clinical curiosity. Aust NZ J Obstet Gynaecol 27: 168, 1987 |
|
Summers JL, Ford ML: The forgotten pessary: A medical oddity. Am J Obstet Gynecol 111: 307, 1991 |
|
McElin TW, Paalman RJ: Pessary complications in the management of uterine prolapse. Am J Obstet Gynecol 78: 643, 1959 |
|
Poma PA: Management of incarcerated vaginal pessaries. J Am Geriatr Soc 29: 325, 1981 |
|
Knight DG, Kernohan N: The “forgotten” vaginal ring pessary—An unusual cause of rupture of the urinary bladder. Br Med J 292: 992, 1986 |
|
Arias BE, Ridgeway B, Barber MD: Complications of neglected vaginal pessaries: case presentation and literaturereview. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Aug;19(8):1173-8. Epub 2008 Feb 27. |