Syphilis is classified in sequential clinical stages to guide patient treatment, management
of sexual partners, and, in the case of pregnant
women, newborn care. Despite their clinical and public health utility, these
stages are neither precise nor mutually exclusive. Symptoms and
signs of early syphilis often are missed or confused with manifestations
of other diseases. The temporal distinction between early and late
latent infection is somewhat arbitrary. Furthermore, in individual patients, stages
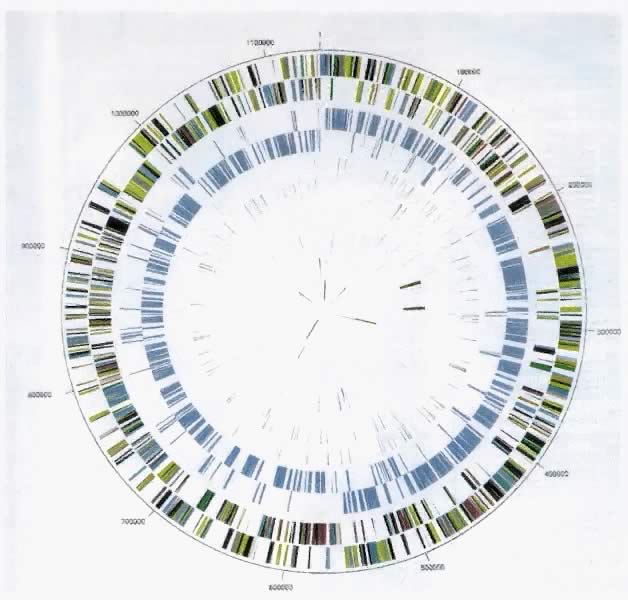
may overlap (Fig. 7). However, the stages discussed in this section offer a critical conceptual
framework for clinical management decisions.  Fig. 7. Clinical course of untreated syphilis. The approximate proportion of persons
developing clinical disease is indicated in parentheses. The actual
proportion of infected persons who develop primary or secondary manifestations
is not known.(Modified from Zabriskie V, Lukehart S: Syphilis. In Sciarra JJ [ed]: Gynecology
and Obstetrics. Philadelphia, JB Lippincott, 1985; as
originally modified from Morgan HJ: Comments on the syphilis problem
in the United States. South Med J 26:18, 1933. Courtesy of Kathy Dry
and Diane Vitro, Division of STD Prevention, NCHSTP, CDC, Atlanta, GA.) Fig. 7. Clinical course of untreated syphilis. The approximate proportion of persons
developing clinical disease is indicated in parentheses. The actual
proportion of infected persons who develop primary or secondary manifestations
is not known.(Modified from Zabriskie V, Lukehart S: Syphilis. In Sciarra JJ [ed]: Gynecology
and Obstetrics. Philadelphia, JB Lippincott, 1985; as
originally modified from Morgan HJ: Comments on the syphilis problem
in the United States. South Med J 26:18, 1933. Courtesy of Kathy Dry
and Diane Vitro, Division of STD Prevention, NCHSTP, CDC, Atlanta, GA.)
|
Primary Syphilis The ulcer, or “chancre” (see Figs. 5 and 6), which is the defining manifestation of primary syphilis, usually develops
from a painless papule about 3 weeks after exposure, with the range
of the 10- to 90-day incubation period being directly related to the
size of the T. pallidum inoculum.69,116 Even in the absence of therapy, syphilitic chancres resolve spontaneously
in 2 to 6 weeks. Although traditionally characterized as a single, painless (unless secondarily
infected), indurated, clean-based ulcer that often is associated
with regional adenopathy, syphilitic chancres probably occur as multiple
lesions at least as frequently and meet this classic description
in less than half of cases.14 In one study, the classic constellation of chancre signs was 98% specific
but only 31% sensitive for a diagnosis of syphilis in men.117 Ulcers from syphilis usually range from 0.3 to 3.0 cm in diameter and
occur at the site of infectious contact.14 Chancre location and degree of associated discomfort are important determinants
of whether and when ulcers are detected by patients, thus triggering
them to seek care. In female patients, the most common chancre
locations are the labia majora, labia minora, fourchette, cervix, and
perineum.76,118,119 In pregnant women, cervical chancres are common, with deposition of treponemes
on the often-friable cervix.120 As a result, signs of primary syphilis often go unrecognized in women. Extragenital
lesions also may occur on the lips, oropharynx, nipples, and
fingers, although these are uncommon, occurring in approximately 2% of
patients in one large series.118,119 A history of oral or anal intercourse always should prompt examination
for chancres in these locations. In the United States, genital ulcers are most commonly caused by infection
with herpes simplex virus (HSV), followed by syphilis and chancroid.121 In different areas and clinical settings, however, the relative importance
of specific etiologies varies substantially.117 Both because of the limited sensitivity of clinical diagnosis of genital
ulcer disease for distinct infectious etiologies and because mixed
infections (e.g., HSV and syphilis) are common, all genital ulcers should be tested for T. pallidum infection, regardless of ulcer morphologic features.117,121 Other considerations in the differential diagnosis of genital ulcers are
summarized in Table 2. TABLE 2. Differential Diagnosis of Genital Ulcers
| Infectious Agent | Classic Ulcer Characteristics | Laboratory Diagnosis | Treatment |
Genital herpes | Herpes simplex virus type I or type II | Multiple pustules and vescicles coalesce to form painful ulcers | Culture of lesion or herpes simplex virus serology | Acyclovir or famciclovir or valacyclovir |
Syphilis | Treponema pallidum | Single, painless papule, which necroses to an indurated, clean-based chancre | Darkfield examination or direct immunofluorescence test for T. pallidum; serology | Benzathine penicillin |
Chancroid | Haemophilus ducreyi | Ragged edges, without induration; purulent exudate at ulcer base | Culture for H. ducreyi | Azithromycin or ceftriaxone or ciprofloxacin or erythromycin base |
Granuloma inguinale | Calymmatobacterium granulomatis | Vascular, painless, progressive, ulcerative lesions without regional adenopathy | Visualization of dark-staining Donovan bodies on tissue crush preparation
or biopsy | Trimethoprim-sulfamethoxazole or doxycycline |
Lymphogranuloma venereum | Chlamydia trachomatis serovars L1, L2, or L3 | Small, nonindurated, genital papule, which ulcerates quickly; associated
with acute lymphadenitis | Complement-fixation test, with titer of  1:64, and absence of other causes 1:64, and absence of other causes | Doxycycline or erythromycin base | Secondary Syphilis Lesions of secondary syphilis result from systemic, hematogenous spread
of organisms and usually follow by 4 to 10 weeks the development of primary
chancres.109 Overlap between the two stages therefore occurs, with as many as a third
of patients with secondary syphilis having a chancre present.118,119 In untreated patients, the lesions of secondary syphilis usually resolve
within 3 to 12 weeks but can persist for several months.76,122 Secondary syphilis is manifested by highly variable skin and mucous membrane
lesions, constitutional signs and symptoms, and local organ involvement.76,116,118,122 An evanescent macular eruption, which evolves into a maculopapular or
papular rash on the trunk and extremities (Fig. 8), is the most common finding in secondary syphilis, occurring in at least 90% of
patients in some series.118,119 Lesions often are particularly noticeable on the palms and soles and are
traditionally described as resembling “copper pennies” because
of their round, red, or reddish brown appearance118,119 (Fig. 9). Papules vary from 0.5 to 2 cm in diameter, often cause pruritus, and
can be confused with the lesions of psoriasis, pityriasis rosea, and
drug eruptions.113 These skin lesions may heal with scarring or altered pigmentation, although
most heal without any sequelae.118,119  Fig. 8. Secondary syphilis—papulosquamous rash. Fig. 8. Secondary syphilis—papulosquamous rash.
|
 Fig. 9. Secondary syphilis—rash on palms of hands. Fig. 9. Secondary syphilis—rash on palms of hands.
|
Other manifestations of secondary syphilis include condyloma lata, which
occur in 10% to 15% of patients118 (Fig. 10). These large, raised, white or gray lesions are highly infectious, often
occur in an area near a primary chancre, and may result from the direct
spread of treponemes from the primary lesion in the anogenital region.122 Condyloma lata are readily confused with condyloma acuminatum, the warty
genital lesions that are caused by human papillomavirus, making it
important to screen for syphilis when any ambiguous condylomatous genital
lesions are identified. Mucus patches—shallow, painless, aphthous
ulcer-like plaques that occur in as many as one in five patients—typically
are found on the tongue, buccal mucosa, lips, and cervix.118,122 Secondary syphilis also is an important curable cause of alopecia.  Fig. 10. Secondary syphilis—condyloma lata. Fig. 10. Secondary syphilis—condyloma lata.
|
Systemic signs and symptoms associated with secondary syphilis include
fever, generalized lymphadenopathy, malaise, headache, weight loss, and
myalgia.118,119 Some lymph node enlargement is present in 70% to 85% of patients; the
most commonly involved nodes are inguinal, axillary, posterior cervical, femoral, and
epitrochlear.118,119 Asymptomatic meningitis occurs in as many as 40% of secondary syphilis
patients, subclinical hepatitis in roughly 20%, and jaundice, glomerulonephritis, ocular
complications, and sensorineural deafness in smaller
but significant proportions.122–125 Latent Syphilis After spontaneous resolution of secondary syphilis, the untreated patient, for
a variable period of time, is completely free of symptoms and
signs of the persistent infection being harbored. This state, in which
only serologic evidence of infection can be found, is called latent syphilis. It
is arbitrarily further classified into early and late latent
stages to guide therapy in light of data indicating that 24% of patients
with latent syphilis experience at least one relapse to infectious, secondary
disease and that about 90% of these relapses occur within
the first year of latency.116,122,126,127 Patients with latent syphilis of less than 1 year's duration are, therefore, considered
by the Centers for Disease Control and Prevention
to have early latent infection and to be potentially infectious, whereas
patients with latent syphilis of more than 1 year's duration
carry a diagnosis of late latent infection and are deemed relatively
noninfectious, as well as increasingly immune to reinfection. The World
Health Organization uses a 2-year cutoff to distinguish between early
and late latent infection. Roughly two thirds of untreated patients
with latent syphilis maintain this status for the rest of their lives, but
patients often remain reactive to treponemal tests, even if nontreponemal
test results become negative in the latent stage of syphilis.89 Tertiary Syphilis The three late manifestations of untreated syphilis are called tertiary
syphilis and include neurosyphilis, cardiovascular, and gummatous disease. In
the preantibiotic era, tertiary syphilis was recognized in 15% to 40% of
large cohorts of patients with untreated infection, resulting
in estimates that almost a third of untreated patients may develop
these potentially fatal complications and that about 20% died as a direct
result of them.127–130 Tertiary syphilis may occur from months to many years after initial infection, and
patients frequently experience more than one of the three
syndromes. However, with the advent of both antibiotics and HIV infection, the
incidence and timing of the manifestations of tertiary syphilis
appear to have changed. Neurosyphilis currently is the most important of the tertiary complications
of syphilis, both because it is probably the most common and because
it is frequently severe, when it does occur. However, neurologic involvement
from syphilis is not restricted to late-stage disease. Many
patients with syphilis have cerebrospinal fluid (CSF) invasion by treponemes
during the first year but remain asymptomatic, with CSF abnormalities
such as elevated leukocyte count and protein, and reactive CSF
Venereal Disease Research Laboratory (VDRL) test in the absence of clinical
disease.131–133 In these patients, the degree of CSF abnormality correlates with the risk
of subsequent development of symptomatic neurosyphilis.134,135 Symptomatic disease ranges from meningitis, which generally occurs within
the first year, to meningovascular and parenchymous involvement, which
usually present 4 to 12 years and 15 to 20 years after initial infection, respectively.116,134 Thus, neurosyphilis should be considered a continuum that includes tertiary
manifestations but that can and does occur at any time during the
life of a patient with untreated syphilis. Syphilitic meningitis often presents with headache, nausea, vomiting, confusion, and
nuchal rigidity.135,136 Cranial nerve palsies are frequent and most commonly cause visual disturbances, sensorineural
hearing loss, or facial weakness. Meningovascular syphilis refers to central nervous system (CNS) ischemia
or infarction as a result of syphilitic endarteritis. It occurs in approximately 3% of
untreated syphilis patients and accounts for about 10% of
neurosyphilis cases.127–131 Any part of the CNS may be involved, and symptoms reflect lesion location. They
may include hemiparesis or hemiplegia, aphasia, seizures, headaches, impaired
memory, apathy, vertigo, and insomnia.131,134 Involvement of the third cranial nerve may result in a characteristic
small, fixed Argyll Robertson pupil.134,137 Parenchymous neurosyphilis includes both general paresis and tabes dorsalis. Older
studies suggest that together these syndromes occurred in
about 5% of individuals with untreated syphilis and that general paresis
accounted for about 10% of neurosyphilis, whereas tabes dorsalis was
diagnosed in about a third of neurosyphilis cases.127–131,134 General paresis is a progressive dementia caused by treponemal invasion
of the cerebrum and evidenced by gradual impairment of memory and cognitive
functions, irritability, personality changes, psychosis, and, ultimately, death.136 Seizures, tremors, and impaired speech or handwriting may be the presenting
complaint. Tabes dorsalis is characterized by demyelinization of
the dorsal ganglia, dorsal roots, and posterior columns. Early clinical
features include sensory ataxia, lightning pains of the lower extremities (75% to 90% of
patients), autonomic disturbances, paresthesia, and
altered pupillary light responses.131,132,136 Pains with hyperesthesia worsen as the disease progresses.127 Patients may experience severe epigastric pain, nausea, vomiting, ataxia, bladder
disturbances, impotence, and impaired position and vibration
sense.131,132,136 Argyll Robertson pupils and Charcot's joints (trophic degeneration) also
are reported.136,137 Cardiovascular syphilis is rarely diagnosed currently but may have accounted
for 10% to 15% of all clinical cardiovascular disease in the preantibiotic
era.76,134,138,139 Studies from that period suggest that at least 10% to 30% of patients
with untreated syphilis developed cardiovascular complications, with autopsy
series producing estimates ranging from 30% to 80%.127–130 Cardiovascular problems usually occur 15 to 30 years after primary infection
and result from local inflammation caused by the multiplication
of treponemes within the wall of the aorta.134,140 The ascending aorta is most commonly involved in the aortitis of cardiovascular
syphilis, with endarteritis obliterans of the vasa vasorum producing
medial necrosis and resulting, most frequently, in aneurysms
of the aorta or other large vessels, aortic insufficiency, and congestive
heart failure.134,138,141–143 Although syphilitic aortitis often is uncomplicated and asymptomatic, about 20% of
patients with aortitis have symptoms of substernal dull, aching
pain, and 25% experience heart failure.76,139 Like cardiovascular syphilis, the incidence of gummatous syphilis has declined
substantially from as high as 15% of untreated syphilis patients
in the preantibiotic era to a relatively rare diagnosis.127,134,140 The gummas of tertiary syphilis probably result from delayed-type hypersensitivity
reactions to treponemal antigens and are locally destructive, recurrent
lesions of varying size that usually occur in the skin
and bones but also may involve mucous membranes of the oropharynx, visceral
organs such as the liver, heart or brain, ocular structures, and
muscles, with the symptoms and severity of the consequences being related
to the location81,144 (Fig. 11). Most gummas develop 2 to 45 years after initial infection, with most
occurring after 10 to 15 years.145 Skeletal gummas commonly cause nocturnal pain and local swelling because
of the associated periostitis.134 Because gummas contain few treponemes and respond rapidly to antibiotic
treatment, this late manifestation of syphilis also is called late benign
syphilis, despite the lethal consequences of myocardial and nervous
system lesions.81,140  Fig. 11. Tertiary syphilis—ulcerating gumma. Fig. 11. Tertiary syphilis—ulcerating gumma.
|
Congenital Syphilis Congenital syphilis manifestations are divided into two stages—early (less
than 2 years), and late (more than 2 years). Early clinical
signs may include lesions seen in cases of secondary syphilis, pneumonia, or
failure to thrive.76,79,80 Most manifestations develop within the first 3 months of life and include
persistent rhinitis (snuffles) consisting of a highly infectious, profuse, purulent
or blood-tinged nasal discharge, hepatosplenomegaly, palmar
and plantar bullae, glomerulonephritis, generalized lymphadenopathy, erythematous
maculopapular rash, petechia, anemia, jaundice, abnormal
bone radiographs, and pseudoparalysis.103,146 CSF abnormalities in the absence of other symptoms occur in up to 80% of
infected infants.147 Osteochondritis in the long bones affects more than 80% of infected infants148 and most often is diagnosed radiographically in the femur, tibia, and
radius.149 It causes a painful, flaccid pseudoparalysis, usually within 8 months
of life.149 Radiographic findings for osteochondritis are specific and require approximately 5 weeks
to become demonstrable: a classic “celery stick” appearance
is caused by proliferative and destructive changes
in the affected bones, usually in areas of rapid bone growth such as
the periosteum.150 Another bone lesion, diaphyseal periostitis, is asymptomatic, does not
produce radiologic signs until after 12 to 16 weeks of age, and most
commonly affects the tibias, the tubular bones of the hands and feet, and
the clavicles and skull.2,150 Late CS is preventable by diagnosis and treatment of early infection. Late
manifestations of CS are not infectious because they are the delayed
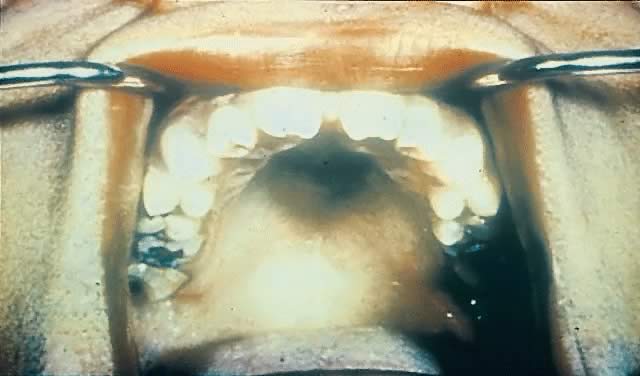
consequences of earlier treponemal inflammatory processes.151,152 They often occur near puberty and include Hutchinson's triad of interstitial
keratitis, peg-shaped upper incisors, and eighth cranial nerve
deafness.153 Keratitis is the most common manifestation of the triad (20% to 50%)154 and involves unilateral photophobia, pain, excess tearing, and blurred
vision.76,154 Its onset usually is between 5 and 16 years of age and occurs more commonly
in female than male patients.76 The peg-shaped upper incisors (Hutchinson's teeth) result from misshapen
and hypoplastic permanent teeth in late CS155 (Fig. 12). Hearing loss, the least common symptom of Hutchinson's triad, often
occurs by age 10 and results from osteochondritis causing cochlear
degeneration.156 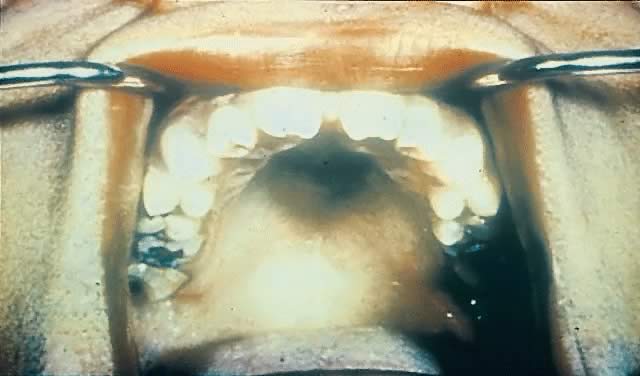 Fig. 12. Congenital syphilis—Hutchinson's teeth. Fig. 12. Congenital syphilis—Hutchinson's teeth.
|
Other characteristic findings of late CS include frontal bossing, short
maxillae, saddle nose, palatal deformations, bilateral knee effusions, sternoclavicular
thickening, flaring scapulas, mental retardation, hydrocephalus, and
neurosyphilis.147,156,157 Syphilis in HIV-Infected Persons Clinical manifestations of syphilis are largely unchanged in persons with
HIV infection. However, a few human and animal studies suggest more
rapid and more severe manifestations of syphilis with concurrent HIV
infection, likely because of compromise of immune function.157a–157c Patients with HIV infection may be more likely to present in the secondary
stage of syphilis.157a Those with secondary syphilis may more often have concurrent manifestations
of primary disease, such as chancres or ulcerating skin lesions.157b In addition, an increased incidence of neurologic sequelae, such as meningitis
and ocular syphilis, has been reported in patients coinfected
with syphilis and HIV.157d |



 1:64, and absence of other causes
1:64, and absence of other causes