The causes of proximal tubal obstruction include salpingitis isthmica nodosa, obliterative
fibrosis, endometriosis, and follicular salpingitis. Endotubal
synechiae, mucus, debris, and cornual spasm can simulate
organic proximal tubal obstruction. Attempts to overcome proximal tubal obstruction date from the middle of
the 19th century. Metal probes were inserted transcervically until it
was felt that the intramural tubal segment was reached and then presumably
these probes were advanced until the “obstruction” was
overcome (Fig. 2). Until the use of the HSG became a part of the infertility work-up, the
diagnosis of proximal tubal obstruction could only be suspected. In
this condition the intramural (interstitial) segment that connects the
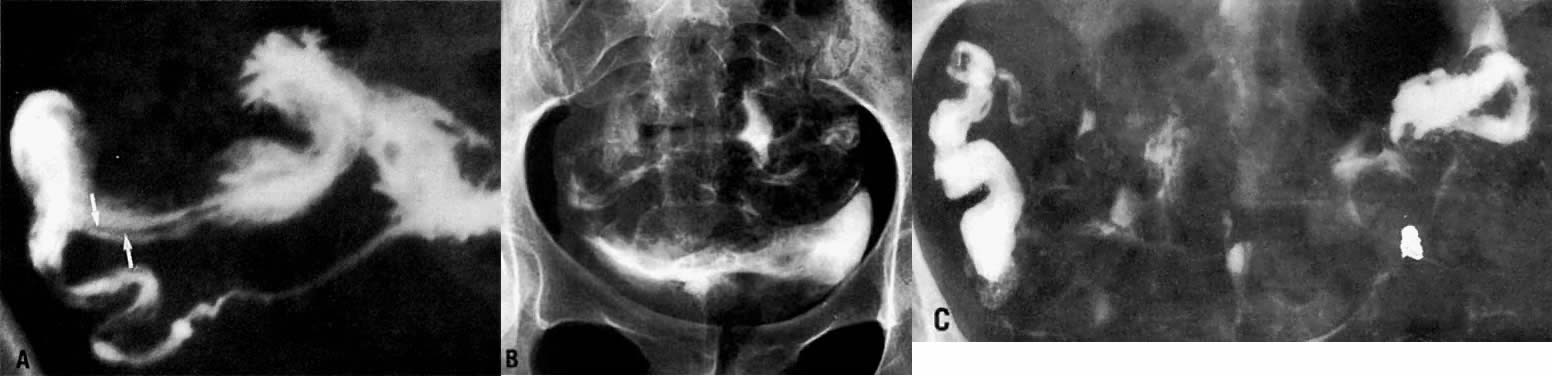
cornua to the isthmus usually is patent. On the HSG, the contrast material
should show pointed rather than rounded ends (Fig. 3); failure of the tubes to opacify with contrast material is presumptive
evidence of proximal obstruction, but tubal spasm, synechiae, and “debris” can
simulate organic occlusion. In analyzing the HSG, it
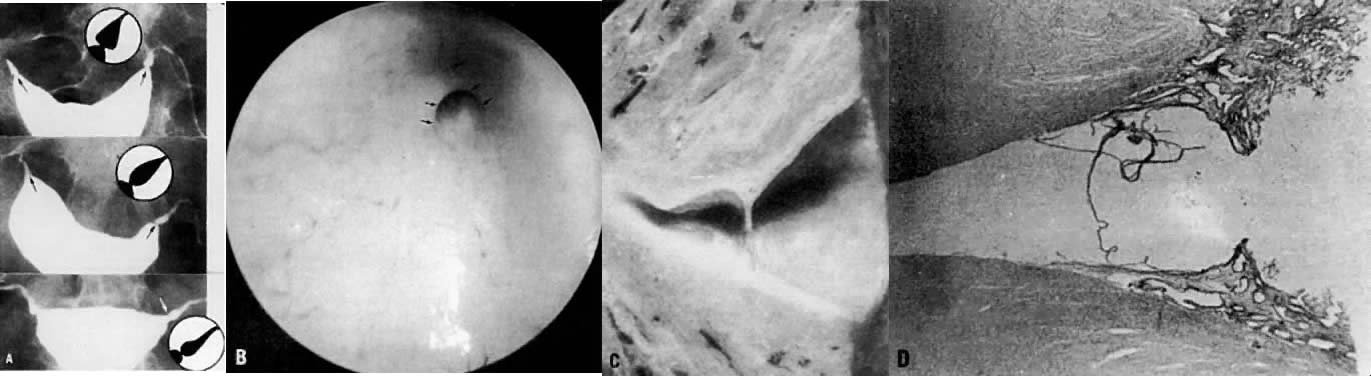
is important to remember that the length of the intramural segment
is about the width of the thumb. A thumb placed at the cornua on the
radiograph will cover the width of the myometrium (Fig. 4).11  Fig. 2. Schematic representation illustrates a wire guided through the intramural
segment.(Gardner AK: The Causes and Curative Treatment of Sterility with a Preliminary
Statement on the Physiology of Generation. New York, DeWitt and
Davenport, 1856) Fig. 2. Schematic representation illustrates a wire guided through the intramural
segment.(Gardner AK: The Causes and Curative Treatment of Sterility with a Preliminary
Statement on the Physiology of Generation. New York, DeWitt and
Davenport, 1856)
|
 Fig. 3. Rounded cornua suggest either incomplete uterine filling or uterotubal
spasm. Fig. 3. Rounded cornua suggest either incomplete uterine filling or uterotubal
spasm.
|
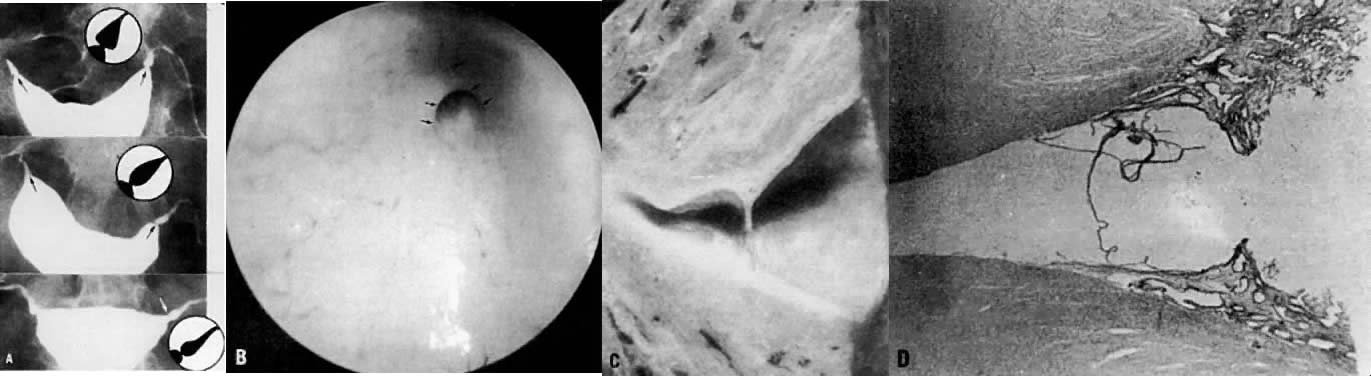 Fig. 4. A. The arrows point to the intramural segment. The inset depicts this part
of the tube and generally represents the width of the myometrium. B. The cause of the pretubal bulge is a membrane at the uterotubal ostium (arrows) seen during hysteroscopy. C. Cut section shows cornu, pretubal bulge, and small membrane. D. Histologic examination reveals endometrium ending at this membrane. Fig. 4. A. The arrows point to the intramural segment. The inset depicts this part
of the tube and generally represents the width of the myometrium. B. The cause of the pretubal bulge is a membrane at the uterotubal ostium (arrows) seen during hysteroscopy. C. Cut section shows cornu, pretubal bulge, and small membrane. D. Histologic examination reveals endometrium ending at this membrane.
|
Laparoscopy with chromopertubation is required to prove the diagnosis. The
next procedure to be undertaken at this juncture is a transcervical
tuboplasty. Most reports have documented the feasibility of transcervical
tubal cannulation as a diagnostic and therapeutic procedure that
in some cases could replace an abdominal tuboplasty.12 This procedure does not require extensive preoperative preparation or
laboratory evaluation. It can be done under analgesia, intravenous sedation, or
a paracervical block. Fluoroscopic, sonographic, or endoscopic
control (Fig. 5) can be used. Grow and colleagues13 reviewed the published series on transcervical tubal cannulation until 1993, describing
its success in establishing patency and pregnancy rates. They
also noted its use for deposition of gametes and embryos and
for direct observation of the endosalpinx.  Fig. 5. Tubal cannulation done under hysteroscopic control. Fig. 5. Tubal cannulation done under hysteroscopic control.
|
Macrosurgery has been replaced by microsurgical techniques, the latter
requiring a laparotomy to achieve the best results. Once it is clear that
the proximal obstruction cannot be overcome by transcervical cannulation
and that the distal tubal segment is grossly normal, the surgeon
can elect to do a tubal anastomosis by resecting the occluded portion
of the tube. Proximal obstructions occur mostly either at the junction
of the interstitial and isthmic segments or in the tubal isthmus. Tubotubal
anastomoses are made between equal or unequal tubal segments, and
each type requires special consideration.14 The intramural segment has the smallest lumen and the ampullary the widest, with
a thin myosalpinx. Only after patency has been established
in the remaining resected segments and their ends examined microscopically
to ensure that they are normal can the anastomosis begin. To reduce
tension on the anastomosis, a suture in the myosalpinx is used to approximate
the tubal segments. When the anastomosis involves the intramural
segment, four mucosal folds should be identified and free-flowing
indigo carmine is expected. Injection of a dilute solution of vasopressin
into the cornual region with a fine-gauge needle helps to reduce
the oozing from this region. The posterior 6 o'clock suture is placed
initially in the distal segment from the serosal side toward the edge
of the lumen. Then it is sutured to the proximal segment so that the
knot is external to the lumen. Usually a two-layered anastomosis is done
and tubal patency tested. Some leakage may be seen at the site of the
anastomosis, although a true test of patency is observation of dye
at the fimbriated end. These general principles apply to most types of
anastomoses. There is evidence to suggest that tubal length is related
directly to a successful outcome, and there is an inverse relationship
between the final length and the rapidity of conception. Although laparoscopists
have done tubotubal anastomoses, the results are not as
good as those reported from microsurgical procedures. A study of microsurgical
anastomosis on the rat uterine horn, in which two, four, and
eight sutures were used, compared the results after 60 days. Since no
differences were noted in the serosal, muscularis, or endosalpingeal layers
in any of the groups, it would appear that two sutures were adequate
for tissue repair.15 Tubo-uterine Implantation If fibrosis replaces the entire interstitial tubal segment, then implantation
is required. This condition is rare, so implantations are done
infrequently. The advent of the surgical microscope has made tubocornual
anastomosis the preferred procedure for the management of proximal
tubal obstruction involving the interstitial isthmic segments, such that
a tubal implantation procedure has become of historic interest. The
advantages of tubocornual anastomosis over tubal implantation are as
follows: There is less bleeding.
Less uterine and tubal tissue is removed.
There is a reduced chance of uterine rupture should pregnancy result.
Cesarean delivery is not needed because the uterine wall is not weakened.
Implantation remains a possibility should tubocornual anastomosis fail.
Reversal of Tubal Sterilization The fundamental operation for reversal of a tubal sterilization is a microsurgical
anastomosis. Success of the procedure depends on the extent
of tubal destruction and the length of the repaired tubal segments. If
the reconstructed tube has a length of at least 4 cm with an ampullary
length of 1 cm, live birth rates of 60% to 80% can be achieved. The
tubal pregnancy rates vary, but average 2% to 5%. Kroener sterilization (fimbriectomy) has been considered irreversible, but
if at least 50% of the ampulla has been preserved an ampullary salpingoneostomy
will yield a significant live birth rate. Experimental studies to evaluate the effectiveness of several types of
anastomoses including the use of fibrin adhesive,16,17,18 tissue-adhesive cyanoacrylate,19 and laser welding20 have been used on animals to evaluate the efficacy of the procedures. The
time required for the procedures, the degree of adhesion formation, and
the patency of the anastomosis were evaluated, and the quality of
the scars were examined grossly and histologically. Each procedure appeared
to have severe limitations, either because of foreign body granulomatous
reactions or because it was unsuitable for certain types of
anastomoses, notably the tubocornual procedures. Laparoscopic tubal anastomosis
was done on five previously sterilized patients, and patency
was documented in 5 of the 10 tubes. The crude pregnancy rate was 50%.21 The most frequent reason to do a tubal anastomosis is to reverse a previous
sterilization. Careful screening with the inclusion of a preliminary
laparoscopy is essential if the type of sterilization is not known, if
there is no pathology report of an extirpated specimen, or if electrosurgery
was used to sterilize the patient. Most patients become pregnant
within 2 years after the reversal. If pregnancy does not occur
within 6 months of the operation, an HSG is suggested to detect the patency
of the anastomosis. There is evidence to show a direct relationship
between the length of the repaired tube and the time required for
a postoperative conception. Pregnancy rates seem to be better in patients
who have undergone removal of mechanical devices used for sterilization (e.g., clip or falope ring) than in patients who have undergone reversal of
electrosurgical sterilization. |