Basic Tenets Safe and effective performance of open laparoscopy is based on four tenets: - Dissection of the minilaparotomy incision in layers and elevation of the
fascia and deeper layers during incision: Entering the abdomen using a knife without proper dissection and fascial
elevation increases the risk of complications. Bartsich and Dillon12 report cutting the superior mesenteric vein during the initial subumbilical
skin incision of an intended closed laparoscopy procedure.
- After visual confirmation of abdominal entry, insufflation of gas into
the abdomen directly through the cannula with the blunt obturator in place: This eliminates preperitoneal insufflation and shortens the time needed
to establish the pneumoperitoneum. The blunt obturator should not be
withdrawn until the abdomen is partially distended to avoid injury to
internal structures by the sharp edge of the bare cannula.
- Blocking the escape of gas from the abdomen: Loss of the pneumoperitoneum through gas leaks exposes the surgeon to
the risk of inadequate visualization and potential complication.
- Proper closure of the fascial defect at the end of the procedure: Proper fascial repair minimizes the occurrence of postoperative herniation.
Procedure When satisfactory anesthesia has been achieved, the surgeon applies two
Allis clamps on the lateral margins of the umbilicus and makes a vertical
incision at the 6-o'clock position of the lower umbilical margin, extending
inferiorly for a distance of 1 to 2.5 cm (Fig. 6). The Allis clamps are repositioned on the skin edges to be used for retraction. Closed
scissors are introduced into the incision, and the blades
are separated several times to dissect connective tissue fibers
found between the skin and deep fascia. The surgeon directs a Kocher clamp
toward the upper angle of the incision and grasps the inferior margin
of the umbilical ring where the fascia is fused with the skin. The
surgeon lifts and everts the fascia and applies a second Kocher clamp
on it more inferiorly (Fig. 7). The fascia is clearly identified by separating it from surrounding fibrous, adipose, and
areolar tissue with blunt or sharp dissection. The
first Kocher clamp can be reapplied on the fascia to realize a more
secure purchase, as indicated.  Fig. 6. Stretching the skin and making a vertical incision. Fig. 6. Stretching the skin and making a vertical incision.
|
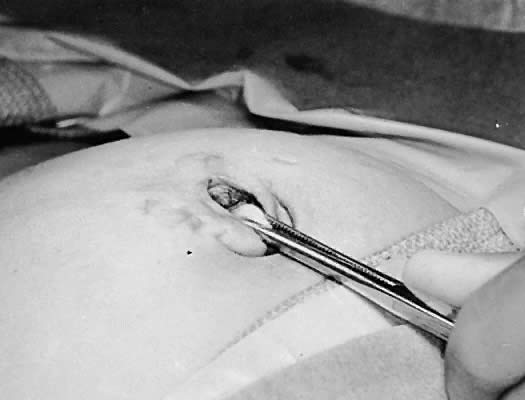
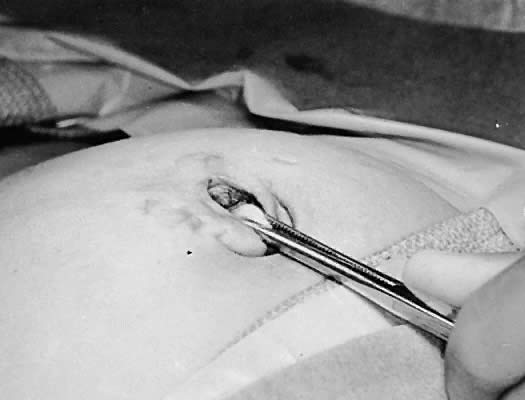 Fig. 7. Grasping the deep fascia close to its attachment to the skin and lifting
it upward and superiorly. Fig. 7. Grasping the deep fascia close to its attachment to the skin and lifting
it upward and superiorly.
|
The surgeon raises the deep fascia with the Kocher clamps and incises the
fascia carefully between the clamps while maintaining fascial elevation. Raising
the fascia separates the abdominal wall from the bowel and
omentum and minimizes the possibility of inadvertent damage during
fascial incision. The initial size of incision need not exceed 0.5 cm. The
incision then is enlarged using a spreading hemostat. Usually, the
peritoneum is entered by the spreading hemostat. Otherwise, the flat
end of one S-shaped retractor is introduced into the incisional gap and
is pressed against the peritoneum for abdominal entry (Fig. 8). The surgeon passes a suture through each fascial edge and tags it. The
S-shaped retractor lodged within the incision acts as a backstop to
the needle. The second S-shaped retractor then is placed through the
fascial gap into the peritoneal cavity, and the abdominal wall is raised
with both retractors to confirm peritoneal entry by viewing the bowel
and omentum. If the surgeon discovers that the abdominal cavity had
not been entered, the surgeon identifies and retracts the rectus muscle, exposes
the peritoneum, and enters it with a thrust of a small hemostat. The
hemostat is opened inside the peritoneal cavity, and a retractor
is placed in the abdomen between the open jaws of the hemostat. The
hemostat is removed, and the other retractor is applied on the opposite
side. Occasionally, abdominal entry is not possible with the previously
described procedures because of the presence of a well-developed
Richet's fascia. In this case, the surgeon should lift Ricket's
fascia and peritoneum with two hemostats and incise them carefully
to avoid nicking the small bowel. In any case, the surgeon must confirm
peritoneal entry through visualization of the small bowel or omentum.  Fig. 8. Enlarging the fascial incision with the spread of a hemostat and placement
of an S-shaped retractor. Fig. 8. Enlarging the fascial incision with the spread of a hemostat and placement
of an S-shaped retractor.
|
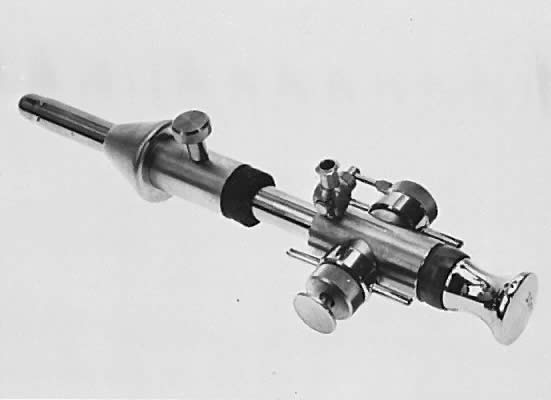
The surgeon prepares the open laparoscopy cannula for insertion by sliding
the cone sleeve over the shaft and locking the cone in a position
consistent with the individual thickness of the abdominal wall. The cannula
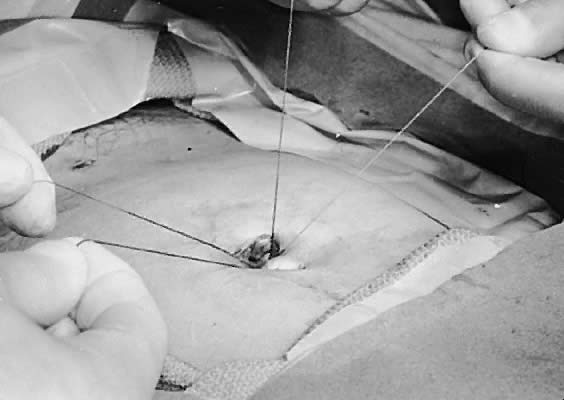
then is introduced between the retractors into the abdominal cavity (Fig. 9). The fascial tag sutures are held tensely upward and threaded into the
V-shaped suture holders (Fig. 10). This maneuver fixes the cannula on the abdominal wall and pulls the
fascia against the cone to prevent escape of the gas (Fig. 11). Gas insufflation is initiated during threading of the fascial tag sutures
into the suture holders. The blunt obturator is removed to permit
a rapid flow of the gas.  Fig. 9. Introducing the open laparoscopy cannula into the abdomen, guided by the
S-shaped retractors. Fig. 9. Introducing the open laparoscopy cannula into the abdomen, guided by the
S-shaped retractors.
|
 Fig. 10. Fixing the fascial tag sutures into the V-shaped suture holders. Fig. 10. Fixing the fascial tag sutures into the V-shaped suture holders.
|
 Fig. 11. Creation of an airtight seal following pulling of the sutures snugly into
the holders. Fig. 11. Creation of an airtight seal following pulling of the sutures snugly into
the holders.
|
The surgeon introduces the laparoscope, with or without an attached camera, through
the open laparoscopy cannula and performs the intended procedure. When
the endoscopic procedure is completed, the surgeon deflates
the distended peritoneal cavity, withdraws the cannula, and closes
the abdominal wall in two layers. The fascial tag sutures are used to
approximate the fascia. The surgeon positions the sutures in parallel
alignment (Fig. 12), ties a square knot on one side (Fig. 13), pulls the tied suture against the fascia, and ties a second knot on
the opposite side of the fascia (Fig. 14). The skin is approximated loosely. 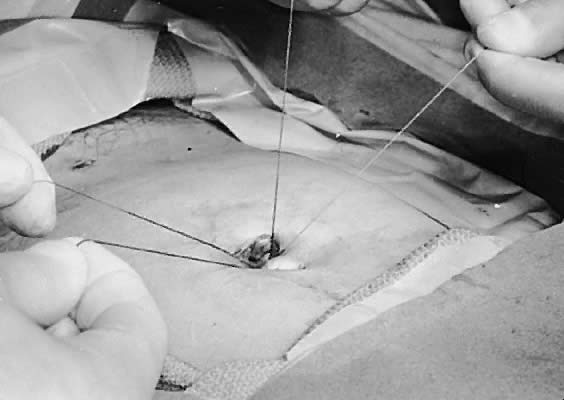 Fig. 12. Alignment of the superior and inferior tag sutures parallel to each other. Fig. 12. Alignment of the superior and inferior tag sutures parallel to each other.
|
 Fig. 13. Tying the first knot combining fascial tag sutures on the left side of
the patient. Fig. 13. Tying the first knot combining fascial tag sutures on the left side of
the patient.
|
 Fig. 14. Tying the second knot combining fascial tag sutures on the right side of
the patient, effecting closure of the fascia. Fig. 14. Tying the second knot combining fascial tag sutures on the right side of
the patient, effecting closure of the fascia.
|
Technical Pitfalls Although open laparoscopy is a simple operation, there are several pitfalls
that increase technical difficulty. These are outlined in Table 1. TABLE 1. Technical Pitfalls in Open Laparoscopy
Pitfall | Reason | Remedy |
Skin incision is made too small for degree of surgeon's experience
or patient obesity. | Ease of operation is inversely related to size of skin incision. | To improve exposure, enlarge skin incision to maximum of 2.5 cm |
Retraction is applied upward on angle greater than 60 degrees. | Such upward retraction increases distance to operative site and diminishes
view. | To improve exposure, apply retraction force at projected angle of 45 degrees
or less. |
Failure to raise fascia during incision | Possible injury to deeper structures | To increase safety, maintain fascial elevation during incision |
Fascial incision is not enlarged with hemostat. | It is difficult to pass sutures into fascial edges that are not clearly
visible. | To clearly expose the fascial edges and peritoneum, enlarge the fascial
gap |
| It is also difficult to expose or enter peritoneum through minute fascial
gap. | |
Use of weak needles and sutures or use of large needles | Needle may break inside operative field. | To avoid breakage and to enhance ease of manipulation, use a small, strong
needle attached to suture of adequate tensile strength |
| Sutures may break while being threaded in suture holders. Large needle
is awkward to use in small operative field. | |
Failure to stabilize cannula while threading the fascial sutures into suture
holders | Cannula may be dislodged into properitoneal space while fascial sutures
are being pulled upward. | To prevent cannula from being displaced, press it gently against abdominal
wall as fascial sutures are being pulled upward |
Failure to pull fascial sutures tensely into suture holders | Lax fascial sutures do not pull fascial edges snugly against cone of cannula. Gas
may excape. | To create an airtight seal, hold fascial sutures taut as they are wedged
into suture holders | Other Procedures Using Similar Concepts Several operations applying similar concepts of abdominal entry for laparoscopy
have been proposed. These procedures use a standard laparoscopic
cannula, not the open laparoscopy cannula. The modified techniques
of open laparoscopy are safe and effective to the extent that they observe
the basic tenets of the procedure and succeed in providing an airtight
seal around the cannula. Additionally, care must be exercised while
introducing the cannula into the abdomen without a protective blunt
obturator to avoid internal injury by the sharp edge of the bare cannula. Examples of methods described to block escape of the gas around a standard
cannula include using a purse-string suture in the fascia (with or
without a rubber tube choker)13, 14 or in the subcutaneous tissue,15 and applying towel clips,16-18 Allis clamps,19 or suture20 to the skin and subcutaneous tissue surrounding the cannula. |