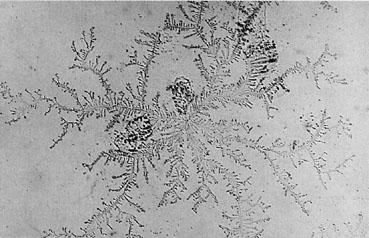
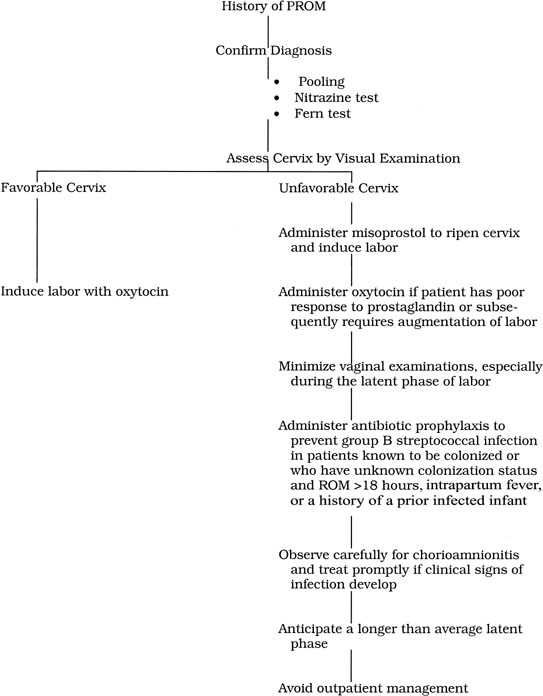
Once the diagnosis of PROM is confirmed, the next step in clinical management
is to determine whether the cervix is favorable for induction of
labor. In most instances, this assessment can be made by visual inspection
of the cervix during a sterile speculum examination. The rationale
for this recommendation is based on the twin issues of reliability
and safety. With respect to reliability, Munson and colleagues14 prospectively compared the results of a digital and visual cervical examination
in 133 women with spontaneous ROM. The coefficient of correlation
for the two examinations was 0.74 with respect to assessment of
cervical effacement and dilatation. The degree of correlation did not
differ significantly depending on the level of training of the examiner. From the perspective of safety, several authors have demonstrated an association
between even a single digital examination and increased risk
of neonatal infection. In an earlier investigation, Schutte and coworkers15 evaluated 189 term patients who experienced spontaneous ROM at least 24 hours
before delivery. When the interval between the first vaginal examination and delivery also exceeded 24 hours, 4 of 17 (24%) infants
developed infection. When the interval between the first examination and delivery was less than 24 hours, only 1 of 172 (0.6%) neonates
became infected (p < .0001). Similarly, Wagner and associates16 also observed an increased risk of neonatal infection in women who had
a single digital examination at admission and then underwent delayed
induction of labor. On visual examination, if the cervix is posterior in the vagina, thick, and
closed, it should be considered “unfavorable.” If it
is midposition to anterior within the vagina, moderately effaced, and
approximately 2 cm dilated, it should be considered “favorable.” If
the visual examination is problematic, a sterile digital
examination should be performed and a Bishop score assigned. A Bishop
score of 6 or more should be considered favorable for induction. Favorable Cervix If the patient’s cervix is favorable, little is to be gained by
delay. Accordingly, labor should be induced as soon as possible by administration
of oxytocin. Vaginal examinations should be minimized, especially
during the latent phase of labor. If the total length of ROM is
expected to exceed 18 hours, or any other risk factor for group B streptococcal
infection is present, prophylactic antibiotics should be administered
intrapartum unless the patient has recently been tested and
is known to have a negative culture for this organism.17 Unfavorable Cervix The standard textbook guidelines for management of PROM in term patients
originally were based on a series of alarming reports published in the
period 1950 to 1980. In 1952, Calkins18 demonstrated that perinatal mortality increased threefold when the fetal
membranes had been ruptured for longer than 24 hours. In 1962, Russell
and Anderson19 argued convincingly that this mortality could be reduced if patients with
PROM were managed by prompt induction of labor. These authors observed 131 cases
of intrapartum infection in 2644 women (5%) of varying
gestational ages with PROM. Sixty-three percent of infections were
in term patients, and 5 (3.8%) of these infections resulted
in maternal deaths. Four of the deaths occurred in the first phase of
the study when patients were not routinely managed by prompt induction
of labor. In the same period, 10 of 52 infants (19%) born to
mothers with intrapartum infection died. In 1965, Lanier and coworkers20 showed that perinatal mortality doubled in patients with prolonged ROM. Twenty-eight
percent of these women developed intrapartum or postpartum
infection. In patients with intrapartum infection, the perinatal mortality
was 50%. Bryans21 noted equally ominous results in a series of 192 patients with PROM. Thirty-one
percent of women with prolonged ROM developed intrapartum infection; 47% of
their babies died as a result of complications
of infection. Shubeck and colleagues22 reviewed data from the Collaborative Perinatal Project and analyzed the
outcome of 4868 patients with spontaneous ROM. Their investigation included
patients who experienced spontaneous ROM while in labor and women
with PROM. They observed that perinatal mortality increased as duration
of ruptured membranes increased and cautioned that “with
rupture of membranes, the clock of infection starts to tick; from this
point on, isolation and protection of the fetus from external microorganisms
virtually ceases.” In 1967, Webb23 affirmed this ominous prediction with a grim survey of 54 cases of maternal
death associated with PROM. Thirty-one deaths occurred in women at 36 weeks’ gestation or greater, and most were the direct result
of overwhelming infection. Eighty percent of the infants of these mothers
died. Gunn and associates24 also pointed with alarm to the high frequency of infection in patients
with PROM. Overall, 9% of the women in this survey with PROM developed
intrapartum infection. In term patients, 24% of those
with ROM of longer than 24 hours became infected. Sixteen percent of infants
delivered to mothers with intrapartum infection died. The authors
concluded that, in term patients with PROM, early induction of labor
was indicated to reduce the risk of ascending infection. In a subsequent investigation, Johnson and coworkers25 evaluated 8320 women of varying gestational ages who had PROM. In women at 37 weeks’ gestation or greater with prolonged ROM, the incidence
of intrapartum fever was increased significantly compared with that
in the general obstetric population. When duration of membrane rupture
was greater than 72 hours, there was also an increase in perinatal mortality
due, primarily, to stillbirths in patients with intrapartum infection. The reports summarized previously clearly argue in favor of an aggressive
approach to term patients with PROM. When interpreting these observations, however, several
caveats must be observed. First, these investigations
were retrospective and, largely, uncontrolled. Therefore, treatment
groups were not necessarily comparable with respect to other obstetric
and medical complications that might have influenced outcome. Most
of the reports were published at a time when the microbiology of
intrapartum infection was not well understood and when some of the newer, broad-spectrum
antibiotics were not available. Moreover, neonatal
intensive care has improved dramatically in recent years, and the prognosis
for infected neonates is not so unfavorable as previously reported. Many
of the early investigations included both term and preterm patients, and
clearly, the outcomes for these individuals are not comparable. The
definitions of maternal and neonatal infection were neither
uniform nor precise. The time of onset of maternal infection usually was
not specified, nor was the timing of maternal antibiotic administration
noted. Few of the authors employed a standardized management plan
for patients with PROM. Finally, and most important, none of the authors
examined maternal and neonatal outcome in the specific group of term
patients who had a cervix unfavorable for immediate induction of labor. Kappy and colleagues26 were the first group of investigators to challenge the doctrine that all
term patients with PROM required immediate induction of labor, regardless
of the cervical examination. In 1979, they published the results
of a retrospective, uncontrolled survey of 78 term women who had PROM
and whose cervix was unfavorable for induction of labor. Fifteen of
these women (19%) were electively induced at the discretion of
the attending physician; 63 (81%) were observed expectantly for
the onset of spontaneous labor. Of the latter individuals, 85% were
in labor within 24 hours of ROM. Fifteen percent of patients had
latent periods that exceeded 24 hours, and in 4%, the latent period
exceeded 7 days. Seven of the patients (47%) undergoing induction required cesarean
delivery. In each instance, the indication was lack of progress in
labor, although the authors did not distinguish between failed induction
and true arrest of progress in the active phase of labor. Twenty-one
women (33%) who initially were managed expectantly required abdominal
delivery, 9 (43%) for “lack of progress.” This
observed difference in frequency of cesarean delivery was statistically
significant. Moreover, the reduction in frequency of surgery
was achieved without increasing the risk of neonatal or maternal infection. Three years later, Kappy and associates27 provided an additional assessment of the management of PROM in term patients
with a cervix unfavorable for induction of labor. In this second
retrospective investigation, the authors added 72 patients to their
original series of 78. Patients were included in the study if they were
at term and had documented ROM, and the Bishop score by visual inspection
was less than 8. During the period of this investigation, 38 patients (26%) were
managed by immediate induction of labor. Most
of these women were private patients of attending physicians who did not
approve of conservative management. One hundred twelve women (74%) were
observed expectantly for spontaneous onset of labor. Of the 38 women managed by immediate induction of labor, 15 (39%) delivered
abdominally. Twelve cesareans were performed for “lack
of progress” and 3 for fetal distress. Of the 112 patients
who were allowed to enter labor spontaneously, 21 subsequently had cesareans
before labor was well established for reasons such as “breech
presentation, prior cesarean, twin gestation-abnormal lies, suspicion
of infection, and infertility.” Of the 91 women who were
allowed to continue in labor, 11 (12%) required cesareans for either
lack of progress (7) or fetal distress (4). Eighty-seven percent
of patients managed expectantly went into labor within 48 hours. Only 3.6% had
a latent period that exceeded 7 days. In this investigation, the authors defined “lack of progress” as “lack
of cervical effacement and dilation despite good
labor for at least one and one-half hours.” As previously noted, they
did not distinguish between arrest of progress in the latent versus
the active phase of labor. Despite this caveat, the observed difference
in frequency of cesarean delivery in the two groups was highly
significant (p < .01). Moreover, there were no neonatal or fetal deaths and no
instances of proven septicemia or meningitis in either an infant or a
mother. As expected, the frequency of febrile morbidity was higher in
patients who delivered by cesarean. The two reports by Kappy and coworkers26,27 were the impetus for a subsequent report by Duff and colleagues.1 Their investigation was the first prospective comparison of “aggressive” versus “conservative” management in term
patients with PROM and an unfavorable cervix. Their study group was
composed predominantly of indigent patients at _ 36 weeks’ or
longer gestation. For the purpose of the study, the status of the
cervix was assessed by a single sterile digital examination and was
considered unfavorable for induction of labor if effacement was less than 80% and
dilatation less than 2 cm. Patients were assigned to treatment on the basis of their day of admission
to the hospital. One group of women was managed expectantly by awaiting
the spontaneous onset of labor or the development of infection. The
second group underwent induction of labor within 12 hours of admission. An
internal fetal heart rate electrode and uterine pressure catheter
were inserted before infusion of oxytocin was begun. For women in
this group, “failed induction” was defined as failure to
enter the active phase of labor after 12 hours of regular uterine contractions
documented by internal uterine monitoring. Seventy-five patients were managed expectantly, and 59 underwent early
induction of labor. Fifty-two percent of women managed conservatively
were in labor within 12 hours, and 75% were in labor within 24 hours. Nine
women (12%) had latent periods that exceeded 48 hours. The
longest latent period was 161.5 hours. Patients managed by intervention
had a higher frequency of intrapartum infection (16% versus 4%, p < .05). They also had a higher frequency of cesarean delivery (20% versus 8%, p < .05). Fifty-eight percent of the cesareans in the intervention
group were for failed inductions. There were no differences in the frequency
of neonatal infection or duration of maternal hospitalization. After publication of these reports, many clinicians began to adopt a more
conservative approach to the management of PROM at term, especially
in patients whose cervix was unfavorable for induction of labor. However, in 1989, Wagner
and associates16 injected a new note of caution into the debate concerning management of
this difficult clinical problem. These authors studied a group of 182 uncomplicated, term
women who received prenatal care at a large health
maintenance organization (HMO) in California. The diagnosis of unfavorable
cervix (<80% effacement, <2 cm dilatation) was
assessed by visual inspection in 156 patients and by a single sterile
digital examination in 26 women. On admission, patients were assigned
to one of two treatment groups. One group underwent induction of
labor within 6 hours of ROM. The second group was observed for up to 24 hours, awaiting
the onset of spontaneous labor or infection. If labor
did not ensue within 24 hours, oxytocin was administered. In the group managed by early induction, 90% delivered within 24 hours
of ROM. In the delayed group, only 60% delivered within 24 hours (p < .001). Thirty-eight percent of the latter patients
required induction after a latent period of 24 hours. There were no
differences between the two groups in the frequency of cesarean delivery
or maternal infection. However, 48% of infants in the delayed
induction group required diagnostic evaluations for sepsis compared
with only 8% in the early intervention group (p < .001). Significantly more infants in the delayed induction group
received antibiotics pending the result of the evaluation for sepsis. In
addition, there was an increased incidence of proven infection (p = .06) among
the neonates delivered to mothers in the delayed
induction group. The findings of Wagner and associates16 are similar to those subsequently reported by Guise and coworkers.28 In the latter investigation, 112 uncomplicated term patients with an unfavorable
cervix, defined as a Bishop score of 4 or less, were managed in a uniform manner. Patients initially were observed
for approximately 24 hours for evidence of spontaneous labor or
infection. Patients who did not enter labor within 24 hours were induced
with oxytocin. The decision to intervene at this time was based on
two factors: (1) the previous observations of other investigators that
at least 75% to 85% of women were in spontaneous labor
within 24 hours, and (2) the recognition that, in an era of increasing
concern about cost containment, a more extended period of observation
and hospitalization was difficult to justify to third-party payers. Thirty-nine patients(35%) did not enter labor spontaneously and, therefore, required
induction. Twenty-nine (26%) began labor spontaneously
but then required oxytocin augmentation. Forty-four women (39%) began
labor spontaneously and required no intervention. The
frequency of maternal infection for the entire group was 24/112 (21%). Intrapartum
infection was significantly more common in the
women who required induction of labor. Cesarean delivery was more frequently
performed in women who needed induction or augmentation compared
with patients who had no intervention (p < .05). Patients who required induction of labor had a longer hospitalization
than women in the other two groups. Finally, infants born
to mothers in the induction group were significantly more likely to
undergo evaluations for sepsis than infants delivered to mothers who
required no intervention (p < .05). Two other investigators reached different conclusions concerning the effect
of delayed induction. Cammu and colleagues29 evaluated 105 middle-class nulliparas with uncomplicated singleton pregnancies. Once
the diagnosis of PROM was confirmed, the women were observed
for up to 24 hours. Patients were not stratified on the basis of
their cervical examination. If spontaneous labor did not ensue within 24 hours
or by the early morning following admission, oxytocin was administered. The
outcome of these patients was compared with controls who
had artificial ROM and spontaneous or induced labors. Seventy-six women (72%) managed conservatively entered labor within 24 hours, and 38 of
these patients (50%) required augmentation
with oxytocin. Twenty-nine women (28%) were induced. Of these
women, the longest interval from ROM until delivery was 43 hours. The
frequency of infection in study patients and controls was very low, a
fact that reflects the affluent nature of the patient population. There
were no differences between study and control patients in the frequency
of maternal or neonatal infection. Grant and associates30 reported similar findings in a study of 444 term nulliparas. Patients
had a single sterile speculum examination at the time of admission and
then were randomized to immediate induction of labor with oxytocin (n = 219) versus
an initial period of observation (n = 225). Patients
initially managed expectantly received oxytocin if they were
not in labor on the morning after admission. In these patients, the
range in time from admission to induction was 9 to 33 hours. In the conservatively
managed group, the cesarean delivery rate was 11.1% compared
with 17.4% in the immediate induction group (p = .06). More spontaneous vaginal deliveries occurred in the former
group, and these patients had fewer requests for analgesics during
labor. There were no significant differences in the length of labor, the
frequency of maternal or neonatal infection, or the requirement for
therapeutic antibiotics. Shalev and colleagues31 conducted a prospective, but nonrandomized, investigation of 566 women
who were not in labor within 6 hours of ROM. Patients were assigned to
induction at the end of 12 hours (n = 298) versus induction after 72 hours (n = 268). In the former group, 164 (55%) required
oxytocin induction versus 47 (17.5%) in the 72-hour group (p < .001). There were no significant differences in the frequency
of cesarean delivery or maternal and neonatal infection. The overall
length of hospitalization was prolonged in the second group (5 versus 6 days). The
authors concluded that an extensive delay in induction offered
no measurable benefit to mother or infant and increased the expense
and duration of hospitalization. Several features unify the reports reviewed previously. All authors confined
their analysis to patients with an unfavorable cervix. All investigators
routinely excluded from assessment patients who had any medical
or obstetric complication of pregnancy that warranted immediate intervention, such
as hypertension, insulin-dependent diabetes, postdates
pregnancy, malpresentation, or fetal anomaly. All investigators observed
patients in the hospital under a strict protocol that provided for
fetal heart rate testing and surveillance for maternal infection. Cultures
of the lower genital tract, assessment of the peripheral white blood
cell count, and evaluation of maternal temperature were the measures
most consistently employed to detect maternal infection. The authors
intervened promptly by inducing labor if evidence of maternal infection
developed. They also recognized that their study patients were likely
to have very long latent phases and made a determined effort to minimize
the number of vaginal examinations in the early portion of labor. Finally, none
of the authors used laminaria, dilapan, or topical prostaglandin
preparations as cervical-ripening agents. A number of reports have appeared in the literature describing use of prostaglandin
preparations in management of patients with PROM and an unfavorable
cervix. Taken together, these publications have highlighted
and refined a valuable new approach to patients with this troublesome
complication. Granstrom and associates32 were among the first to evaluate the efficacy of prostaglandin E2 (PGE2) for cervical ripening and labor induction in patients with PROM and an
unfavorable cervix. They treated 29 nulliparas and 32 multiparas with
a 3-mg PGE2 vaginal suppository approximately 6 hours after ROM. The cervical examination
was reassessed 5 and 24 hours later. If the cervix was favorable
but no contractions were present, labor was induced with oxytocin. If
the cervix was still unfavorable, a second suppository was administered. Twelve
of the nulliparous women and 21 of the multiparous women
were in labor within 5 hours of application of the first suppository. The
mean application–to–regular contractions interval and
onset of labor–to–delivery interval were 11 and 5.3 hours
in the first group and 5.0 and 4.6 hours in the second group. No maternal
or neonatal infections occurred. van der Walt and Venter33 subsequently assigned 60 uncomplicated term patients with an unfavorable
cervix (Bishop score 5) to three treatment groups: expectant management, immediate
oxytocin induction, and intravaginal PGE2 (two 0.5-mg tablets). The dose of prostaglandin was repeated every 6 hours
up to a maximum of three doses. The mean duration of labor was longest
in the oxytocin group, and all 6 cesarean deliveries were in these
patients. There was no significant difference in the frequency of maternal
or neonatal infection. Women in the prostaglandin group had the
shortest length of hospitalization. Goeschen34 conducted a clinical trial comparing induction of labor with oxytocin
versus PGE2. He initially enrolled 60 women who were at 36 weeks’ gestation or longer and had PROM and a Bishop score of 7 or less and assigned them to receive oxytocin (n = 25) or PGE2 gel (n = 35). The gel was applied intracervically in a dose of 0.4 mg. The
interval from PROM to delivery and the duration of labor were
significantly shorter in the PGE2 group. In addition, the incidence of operative delivery and the frequency
of neonatal infection were lower in the prostaglandin group. Ray and Garite35 reached similar conclusions in a prospective study of 140 women with uncomplicated
pregnancies at greater than 36 weeks’ gestation and
cervical dilatation less than 3 cm. Patients were randomly assigned
to placebo suppository versus 3-mg PGE2 suppository vs. immediate oxytocin infusion. The dose of PGE2 was repeated in 6 hours if the patient was not in labor. Oxytocin was
administered after 12 additional hours if the patient was still not in
labor. Patients who received PGE2 subsequently had a decreased requirement for oxytocin compared with the
placebo group. Patients in the PGE2 and oxytocin group had a significant decrease in the mean time to delivery
compared with the placebo group (16.3 hours, 13.9 hours, and 21.2 hours, respectively). Significantly, the lowest incidence of chorioamnionitis
and endometritis was in the women who received PGE2. There also was a trend toward decreased frequency of cesarean delivery
in the prostaglandin group. A subsequent report by Chua and coworkers36 differed significantly from the findings of van der Walt and Venter,33 Goeschen,34 and Ray and Garite.35 These authors treated 94 women admitted to the National University in
Singapore with PROM at 36 weeks’ gestation or greater. Patients
were assigned to treatment with oxytocin versus PGE2, administered in the form of two 3-mg vaginal pessaries, followed by oxytocin
induction. The mean cervical score was 3.5 in the first group
and 3.6 in the second (p = NS). The length of labor and incidence of operative delivery
did not differ in the two groups. Interestingly, however, the experience with this investigation did not
deter the authors from further use of PGE2 in the same clinical setting.37 They subsequently conducted a double-blind, randomized trial comparing
a 3-mg PGE2 vaginal pessary with placebo for induction of labor in 155 nulliparous
women at greater than 36 weeks with PROM and a modified Bishop score
of less than 6 of 10. If patients did not begin labor within 12 hours, oxytocin
was administered. Compared with women in the placebo group, those
who received PGE2 were less likely to require oxytocin at the end of the 12-hour observation
period (37% versus 58%, p < .002). In addition, they had a significantly shorter interval
from admission to onset of labor, a shorter latent period from ROM to
onset of labor, and shorter interval from admission to delivery. The
overall incidence of maternal and neonatal infection was very low and
did not differ significantly between the two groups. Meikle and colleagues38 provided additional information concerning the safety of PGE2 preparations in term patients with PROM. They reported a retrospective
survey of 148 women who were at 37 weeks’ gestation or greater and who had cervical dilatation
less than 2 cm. In the first phase of the investigation, patients received
PGE2 gel, 4 mg every 12 hours for two doses, and in the second phase, 3-mg
PGE2 vaginal suppositories, every 4 to 6 hours, for a maximum of three doses. Patients
not in labor after the maximum dose of prostaglandin received
oxytocin. Interestingly, 55 women (37%) entered labor spontaneously
following administration of PGE2. None developed chorioamnionitis or endometritis. Only 3 instances (2%) of
hypertoxicity occurred; each of these patients subsequently
delivered vaginally. The cesarean delivery rate in the study group was
relatively low, 18/148 (12%). Two thirds of the cesareans were
for failure to progress. The largest and probably best designed trial of management for term patients
with PROM was published by Hannah and associates.39 These authors randomly assigned over 5000 women to one of four treatment
groups: immediate induction with oxytocin or PGE2 vaginal gel or expectant management followed by induction with oxytocin
or prostaglandin gel if labor did not ensue in 4 days. The overall frequency
of cesarean delivery was very low and did not differ among the
four groups. Women in the expectant management (oxytocin) group had
a significantly higher frequency of infection than women in the induction-with-oxytocin
group—a finding consistent with previous reports. The
rates of neonatal infection were comparably low in all groups, but
neonates in the induction-with-oxytocin group were significantly
less likely to receive antibiotics than those in the expectant management (oxytocin) or
induction-with-prostaglandin group. Women in the study
expressed a greater preference for induction of labor than expectant
management. Of note, 4 perinatal deaths occurred, all in the expectant
management groups. Two of the deaths occurred in infants of women
who were treated as outpatients. In a subsequent investigation, Gafni and coworkers40 assessed the economic impact of the four methods of management used in
the aforementioned trial by Hannah and associates.39 Immediate induction with oxytocin was less expensive than immediate induction
with PGE2 gel or expectant management followed by oxytocin induction after 4 days. The
cost difference ranged from $30 to $49 (American
dollars). Misoprostol, an analog of PGE1, has also been shown to be effective in inducing labor in patients with
an unfavorable cervix, and it offers a marked cost savings compared
with commercially available preparations of PGE2.41,42 In a prospective trial in 99 patients, Sanchez-Ramos and associates42 compared misoprostol tablets (50 μg) administered intravaginally
to intravenous oxytocin for induction of labor in term patients with
PROM and an unfavorable cervix. Oxytocin was used to augment labor as
needed in the misoprostol group. Patients in the misoprostol group required
lower total doses of oxytocin, although there were no significant
differences in time interval to delivery. Fewer patients in the misoprostol
group required operative vaginal delivery (23% versus 33%, relative
risk [RR] 0.76, 95% confidence interval [CI] 0.46 to 1.28). There
were no significant differences in the frequency
of cesarean delivery or maternal and neonatal complications. In another investigation, Varaklis and colleagues43 compared intravaginal misoprostol (25 μg every 2 hours) to intracervical
PGE2 gel (0.5 mg every 6 hours for two doses) for induction of labor in women
with intact membranes and a Bishop score of 5 or less. Women in the misoprostol group had a significantly shorter
mean time from initial administration of the drug to onset of regular
uterine contractions (p = .007) and a corresponding decrease in the mean time to delivery (p = .006). |