|
FIGO defines microinvasive carcinoma of the cervix primarily by depth
of stromal invasion. Stage Ia1 disease is limited to those cervical cancers
with 3 mm or less of invasion. Lesions with invasion to a depth of greater
than 3 mm but no more than 5 mm are considered stage Ia2. Notably, this
definition does not address lymphovascular space involvement. Significant
controversy surrounds the prognostic significance of this histologic finding
and whether it should guide treatment planning if it is known to exist.53,54,55,56,57,58,59,60,61,62,63,64,65,66,67
Whether or not lymphovascular space involvement is present, surgical therapy
for stage Ia disease is curative for nearly all patients.49,67,68,69,70,71,72,73,74,75,76,77,78,79,80
Extrafascial hysterectomy is generally considered adequate treatment
for stage Ia1 cervical cancer. Ostor's review of the literature reveals
that in spite of a 3.7% risk of lymphovascular space involvement,
the risk of recurrence and lymph node metastases is approximately 1%
and the risk of cancer death is only 0.2%.76
Nonetheless, some gynecologic oncologists advocate the same treatment
for stage Ia1 cervical cancer with extensive lymphovascular space involvement
as for stage Ia2 disease. If fertility is to be preserved, a cervical
conization may suffice, provided the surgical margins and postconization
endocervical curettage are negative for carcinoma and dysplasia.72,78
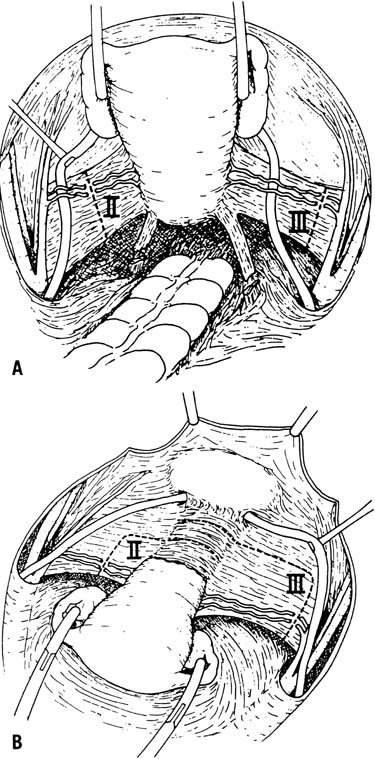
Stage Ia2 cervical cancer is usually treated with a type 2 modified radical
hysterectomy with pelvic lymphadenectomy. Hacker summarized the data on
invasive lesions of 3- to 5-mm depth and found that nodal metastases occur
in 7.3%, recurrences occur in 3.1%, and cancer death occurs
in 2.3%.49 Lymphovascular involvement
may be seen in as many as 18.4% of these patients,76
thus reinforcing the questionable significance of this finding in microinvasive
disease. When future childbearing is desired, cervical conization72,78 or radical trachelectomy80
may be combined with extraperitoneal or laparoscopic lymphadenectomy.
Macroscopic early-stage tumors are also treated successfully with surgery.
The type 3 radical hysterectomy with pelvic and para-aortic lymphadenectomy
is used for patients with stage Ib and IIa cervical cancer. Numerous authors
have found that cure rates approach 85% to 90% and are comparable
with the outcomes of patients treated with primary radiotherapy.81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105
Although these studies show that a majority of patients with stage Ib
carcinoma of the cervix are cured with radical hysterectomy, it became
evident that patients with large tumors had significantly worse outcomes.
It is now well established that primary surgical therapy for bulky (tumor
diameter >4 cm) or barrel-shaped stage Ib disease is associated
with a greater risk of lymph node metastases, local and distant recurrence,
and cancer death.101,106,107,108,109,110,111 Unfortunately,
stage Ib patients treated with primary radiotherapy also tend to have
poorer outcomes as tumor size increases112, 113,114,115 because the high
doses of radiation required to sterilize large tumors exceed the amount
of radiation tolerated by normal tissues.
FIGO acknowledged this survival difference by modifying the staging system.
There is a distinction between smaller Ib1 lesions and larger stage Ib2
tumors. However, in a review of patients with stage Ib cervical cancer
who had been treated with radical hysterectomy, Finan demonstrated that
stage was not an independent predictor of poor outcomes. Rather, he showed
that stage imparted a worse prognosis vis-à-vis nodal metastases,
and that patients with stage Ib2, node-negative disease had significantly
better survival than stage Ib2, node-positive disease.116
Furthermore, the Gynecologic Oncology Group (GOG) and others have studied
patients with “intermediate-risk” stage Ib tumors (including
stage Ib2) treated with primary radical hysterectomy and have yet to demonstrate
a survival benefit with adjuvant radiation in the absence of nodal metastases
or positive surgical margins.117,118
In light of this, it is not surprising that the optimal treatment for stage
Ib2 cancer of the cervix remains controversial. Currently, the treatment
options include radical hysterectomy with adjuvant radiation, radical
hysterectomy with neoadjuvant chemotherapy, radical hysterectomy
with neoadjuvant brachytherapy, primary radiotherapy followed by extrafascial
hysterectomy, primary chemoradiation, and primary chemoradiation
followed by extrafascial hysterectomy.49
In select situations, recurrent or advanced cervical can be managed surgically.
Five-year survival in patients with small pelvic recurrences (<2
cm) confined to the cervix treated with radical hysterectomy has been
reported to be as high as 84% to 90%119,120; however, the incidence of major postoperative
morbidity is 31% to 44%.119,120,121 Conservative surgical treatment of larger
recurrences is ill advised, because as tumor size increases, the overall
survival decreases and the incidence of surgical complications rises dramatically.121
|