The standard therapy for advanced stage cervical cancer is combined pelvic radiation and chemotherapy. The benefit of incorporating extended field radiation is less well-defined. The rationale for extended field radiation is that as many as 30% of patients with advanced stage cervical cancer have metastatic disease to the para-aortic lymph nodes.42 Typically, extensive clinical staging is performed using noninvasive techniques such as computed tomography, magnetic resonance imaging, and lympangiogram to document metastatic disease in the para-aortic lymph nodes. However, clinical staging has been reported to underestimate the extent of disease in 29% to 48% of patients with advanced disease.43–45 Because the proportion of patients without metastatic para-aortic lymph nodes in stage III disease can be as high as 70%, most patients are subjected to extended field radiation unnecessarily.46 Therefore, surgical staging has been advocated in advanced stage cervical cancer to document the extent of disease and assist in treatment planning. Traditionally, this constitutes sampling of pelvic and para-aortic lymph nodes via celiotomy either transperitoneally or extraperitoneally.47–49 One of the disadvantages to surgical staging is that the transperitoneal approach, when followed by radiation, is associated with significant bowel adhesions and enteric morbidity. Although the extraperitoneal approach results in fewer postradiation bowel complications, it still requires a major incision and prolonged hospitalization. Thus, it is easy to understand why, in this group of patients, the use of laparoscopy for pretreatment staging might result in significant patient benefit. If laparoscopy is used for pretreatment surgical staging, it is imperative that the para-aortic lymph nodes be sampled. More extensive studies are required to show that there is a clear advantage of laparoscopic pretreatment staging over the conventional pretreatment celiotomy.
Laparoscopy may have other applications in the management of cervical cancer. Plante and Roy50 have reported using laparoscopy to rule out intra-abdominal disease or metastatic disease before an exenterative procedure, although transposition of ovaries laparoscopically certainly can be achieved while avoiding unnecessary laparotomy.51
Technique of Total Laparoscopic Type III Radical Hysterectomy and Pelvic and Aortic Lymphadenectomy
PREOPERATIVE PREPARATION.
It is essential to retract the bowel away from the pelvis into the upper abdomen. This greatly improves the visual exposure of the operative field and minimizes the potential for inadvertent bowel injury. Several strategies for achieving this are used:
- Mechanical bowel preparation begins 48 hours before surgery with a clear
liquid diet. At 24 hours before surgery, patients ingest 4 L of balanced
electrolyte solution. Fleet's enemas are given on the morning
of surgery until clear. This preparation eliminates bowel contents and
decreases active peristalsis during the procedure; thus, manipulating
the intestines becomes easier and surgical exposure is enhanced.
- An epidural anesthetic is used for splanchnic sympathetic blockade. The
resultant parasympathetic override causes additional contraction of the
bowel. In addition, less-general anesthetic agents are needed during
surgery.
- Nitrous oxide can accumulate in the bowel and increase distension. Thus, the
anesthesiologist is instructed to avoid its use after induction.
- An oral gastric tube is passed into the stomach after intubation and before
any laparoscopic instruments are placed. This decreases the distention
of the upper gastrointestinal tract.
OPERATING ROOM PERSONNEL.
Because this surgery is very dependent on complex machinery and instruments, it is important to have a dedicated team that allows surgery to proceed smoothly. This team must possess expertise for problem solving and on-the-spot equipment maintenance. The scrubbed technician directly participates in the procedure by manipulating the cervix and uterus; by wiping, cleaning, and adjusting the laparoscope during the case; and by handling all sterile troubleshooting measures. This individual can reduce operative times significantly by staying actively involved in the case. The scrubbed technician typically is positioned between the patient's legs with the instrument table just behind him or her. The circulating nurse should also be part of the laparoscopic team and be responsible for stocking necessary supplies. This nurse must be trained and responsible for all nonsterile troubleshooting measures.
INSTRUMENTATION AND EQUIPMENT.
Operating room tables, whether manual or electric, need to provide a Trendelenburg position of approximately 30 to 40 degrees. However, most operating tables do not have this capability. Allen stirrups (Allen Medical Systems, Bedford Heights, OH) are used to secure the lower extremities with the knees bent at right angles and the legs separated. The hips are not flexed. The arms are tucked to the patient's sides, and padded shoulder braces are used at the surgeon's discretion.
Virtually all dissection is performed with a 10-mm argon beam coagulator (ABC) (Conmed Corp, Utica, NY). Because the use of argon gas can lead to high intra-abdominal pressures, one trocar vent is left opened while the ABC is being used. Thus, either one or two high-flow carbon dioxide insufflators, instilling at least 30 L/min, are necessary to maintain adequate pneumoperitoneum during the procedure. Laparoscopic pieces of equipment needed include four 12-mm trocars, two 5-mm graspers with serrated jaws, 5-mm and 10-mm toothed graspers, and two flat-surfaced graspers (used for suturing). The video system includes a Stryker 888 three-chip camera and a Q-5000 light source (Stryker Endoscopy, Santa Clara, CA). Both gauze Raytec sponges (Johnson and Johnson Medical, Arlington, TX) and vaginal “baby” laparotomy tapes with radio-opaque markings can be inserted through a trocar into the peritoneum; these are counted systematically by the operating room staff. Disposable laparoscopic devices required include a LIGACLIP clip applier (Ethicon Endo-surgery, Cincinnati, OH), an EndoGIA vascular stapler (US Surgical, Norwalk, CT) with six to eight reloads, as well as an EndoStitch (US Surgical) suturing device for closing the vagina and an EndoClose device (US Surgical) to close the trocar sites. Finally, a general instrument set with vascular instruments is in the room or immediately outside the door for possible conversion to laparotomy.
SURGICAL TECHNIQUE.
Initially in our experience, radical pelvic surgery using minimally invasive techniques was limited to patients with a Quetelet index of less than 30.52 We currently use an index of 40 as a general limit for radical hysterectomies, but this is not the sole factor in determining whether a patient should undergo laparoscopic radical hysterectomy.
After epidural and general anesthetics are administered, the oral gastric tube is placed. The placement of ureteral stents is optional at this time. Historically, the arguments against placing ureteral stents include (1) increased anesthesia time and (2) the stiffness of the stent, which makes the ureteral dissection more difficult to perform. In our 6-year experience, a concern has arisen that the improved visualization afforded by performing this procedure laparoscopically may result in vascular compromise of the ureter. We hypothesize that periureteral blood vessels, not typically visible to the naked eye during a standard laparotomy, are now clipped or cauterized when dissecting the ureter through the tunnel. This results, on occasion, in an apparent color change of the distal ureter. Whether this change in color is clinically significant is a moot point, as it seems safer to place bilateral ureteral stents prophylactically and remove them in 6 to 12 weeks. Since beginning this practice, our patients have had no ureterovaginal fistulae, and the dissection has not proved as difficult as anticipated.
In addition, placing the stent after the ureter is dissected off of the attached peritoneum can be more difficult because of the loss of countertraction from the surrounding tissue. This has necessitated two “open cystostomies” to pass ureteral stents after having completed the radical hysterectomy laparoscopically. Without question, if stent placement were to be considered, one would be well-advised to place them before surgery. We recently have begun inserting 5-French Infravision ureteral catheters (Stryker Endoscopy), which, when attached to an infrared light source, are easily visualized in the operative field. The bladder is catheterized and an intrauterine sound is placed and taped to a single-toothed tenaculum attached to the cervix.
Four 12-mm trocars typically are used in this procedure. The lateral port sites are located approximately 1 cm medial to the iliac crests, and midline ports are placed at the symphysis pubis and 2 to 3 cm above the umbilicus. A fifth port can be placed for additional retraction or placement of the laparoscopic stapler; this can be positioned either 8 to 10 cm above the umbilicus or just lateral to the periumbilical port. If previous surgical scars are present on the anterior abdominal wall, the procedure is started by placing a Verres needle in the left upper quadrant, just beneath the left costal margin in the midclavicular line. The Verres needle is then replaced with a 2- or 5-mm trocar after insufflating the peritoneum to approximately 14 to 15 mmHg. Using a smaller laparoscope, the surgeon explores the peritoneal cavity for adhesions to the periumbilical region. If present, they are sharply lysed with laparoscopic scissors that are inserted through a trocar placed close to one of the four prospective trocar sites. Vascular adhesions are dissected with the ABC.
Once the anterior adhesions are removed, the periumbilical trocar is placed and the camera is attached to a 10-mm 0-degree laparoscope. The patient is then placed in Trendelenburg, followed by placement of the lateral ports. The suprapubic port is placed while graspers placed through the lateral ports are used to elevate the anterior abdominal wall to prevent tenting of the peritoneum. All trocars are secured to the skin with 0-Vicryl (Ethicon) suture.
In general, if the operating surgeon is right-handed, he or she should stand on the left side of the patient when working in the pelvis and on the right side when operating on the upper abdomen or performing the aortic lymph node dissection or both. The opposite positions are recommended for the left-handed surgeon. We also recommend that when using the ABC, it should be used through a midline port and held in the dominant hand with a grasper in the nondominant hand, just as a surgeon would use scissors in the dominant hand during surgery. The assistant is responsible for the camera and should concentrate on maintaining the tip of the ABC or scissors into center of the video screen while using a grasper in the opposite hand to provide countertraction at the point of dissection. Two video monitors are placed at 45-degree angles at the foot of the bed to allow the surgeon and assistant to stand in a natural, comfortable position. The operating table is also dropped to the lowest position to reduce any additional stress on the surgeon's shoulders during the procedure.
The “baby” laparotomy sponges are placed intra-abdominally at the beginning of the surgery. These are used to absorb small amounts of blood and lymph fluid throughout the case. If any significant bleeding is encountered, the sponge can be used to tamponade the affected area. The sponge also aids with the suction device to prevent unwanted tissue from being aspirated. In addition to using sponges as noted, the liberal use of the ABC, Trendelenburg position, and the modest increases in intraperitoneal pressure result in a surprisingly dry operative field, which is no small part of the success of laparoscopic radical surgery.
Once the trocars are placed, systemic inspection of the peritoneal cavity is performed. The order of the inspection is as follows: (1) diaphragm; (2) liver and gallbladder; (3) spleen; (4) omentum; (5) small and large intestine, which are inspected as they are packed into the upper right quadrant; and (6) the reproductive organs.
DEVELOPMENT OF THE PARAVESICAL AND PARARECTAL SPACES.
With the camera in the periumbilical port, the round ligament is transected at the pelvic side wall with the ABC by use of traction/countertraction. The peritoneum is then incised in an inferior direction. After ensuring the superior vesical artery is medial and the external iliac vein is lateral to the intended field of dissection, the surgeon uses the tip of the ABC to develop the paravesical space bluntly down to the pelvic floor. Small blood vessels are coagulated at this time, and care should be taken to identify the accessory obturator vein, if present, because bleeding from this site can be difficult to control laparoscopically. The paravesical space is bounded by the bladder medially, the cardinal ligament and uterine artery posteriorly, the pubis anteriorly, and the obturator internus laterally.
The peritoneal incision is extended in a cephalad direction along the psoas muscle and parallel to the ovarian vessels to a point well past the pelvic brim. The ABC is used to first “spray” the peritoneal surface before incising it to control any troublesome small peritoneal vessels. The ureter is easily identified as it crosses to the medial peritoneum, and the ovarian vessels can then be transected at a point that allows for either conservation or resection of the ovary/Fallopian tube. With the ureter in view, incising the medial peritoneum just posterior to the ovarian vessels from the pelvic brim to the lateral aspect of the uterus allows an endoscopic stapler placed through the suprapubic port to staple and transect this pedicle.
With the uterus displaced superiorly and to the opposite side of the patient, the ABC is used to coagulate perforators between the ureter and the hypogastric vessels, and the pararectal space is entered. Occasionally, these perforating vessels measure more than 3 mm and should be clipped with the LIGACLIP instead of coagulated. Care should be taken to press the instrument toward the bleeding vessel because activating the LIGACLIP often causes it to retract slightly and the clip is then not optimally placed to achieve hemostasis. Blunt dissection with the ABC is performed carefully down to the levator ani muscle. In developing this space, traction is best directed at 90 degrees to the iliac vessels. This allows the operating surgeon the best opportunity to recognize perforating vessels and either clip or cauterize them before they become problematic. The pararectal space is bounded by the uterosacral ligament medially, the sacrum posteriorly, the hypogastric vessels and piriformis muscle laterally, and the cardinal ligament and uterine vessels anteriorly. When these steps are completed, an adequate assessment of the parametrium can be performed, either with a blunt laparoscopic probe or on manual rectovaginal examination, while the paravesical and pararectal spaces are opened and laparoscopic observation is possible.
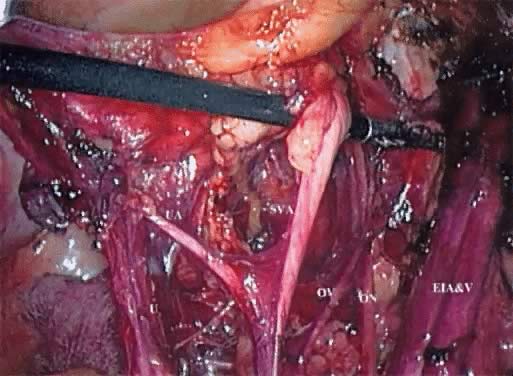
These spaces are similarly developed on the opposite side of the pelvis. If there is no evidence of extracervical disease, the radical hysterectomy and pelvic lymphadenectomy can then be performed. The superior vesical artery is isolated away from its attachments, retracted laterally, and followed proximally from the lateral aspect of the bladder. The middle and inferior vesical arteries are identified and the uterine vessels are isolated, with the ABC developing a space between the superior vesical artery and the uterine artery (Fig. 1). The EndoGIA (U.S. Surgical) is then passed through the suprapubic port and placed across the lateral parametrium. One jaw of the stapler can be visualized extending into the paravesical space with the other jaw in the pararectal space. The stapler is pressed laterally against the hypogastric vessels and superior vesicle artery. After it is ensured that the obturator nerve is free laterally and the ureter is free medially, the stapler is activated, transecting the upper cardinal ligament, including the uterine vessels (Fig. 2).
PELVIC LYMPHADENECTOMY.
For the pelvic lymphadenectomy, the surgeon continues to stand on the patient's left side. Beginning with the nodal tissue overlying the anterior and medial aspect of the common iliac and external iliac artery/vein, lymph-node-bearing tissue is resected using the tip of the ABC as a dissector and coagulator. The contralateral grasper can gently retract the common iliac vessels medially while the ipsilateral grasper elevates these nodes. The dissection is continued distally until the circumflex iliac vein is encountered, serving as the distal boundary of the dissection. Any perforating vessel in this region can be controlled with either the ABC or clip application.
A plane is carefully created between the external iliac vessels and the psoas muscle by retracting these vessels medially. The ABC is then used to coagulate any perforators in this space. The obturator fossa is entered laterally, and attachments of the lymph node bundle to the psoas muscle are incised. The obturator nerve can be identified easily with this approach, and the tip of the ABC is placed just above the nerve and is used to bluntly strip the nodal tissue off the nerve. Using the inferior border of the external iliac vein as a landmark, the nodal tissue can now be retracted medially, and the ABC is used to coagulate the nodal tissue just beneath the vein. This dissection begins at the bifurcation of the internal and external iliac vessels and is performed distally to the point that the obturator nerve exits the pelvis. At the bifurcation of the iliac vessels, the bundle of nodes often are “tethered” to this area. This is caused by attachment and continuation of the nodal bundle lateral and proximal to the bifurcation of the common iliac vessels. Often at this point, the posterior divisions of the hypogastric vein, including the lateral sacral and inferior gluteal veins, are visible. The ABC is of particular value at this point. There is little space for surgical maneuvering because large nerves and fixed veins are present. By using the ABC as a blunt dissector and then with short bursts of coagulating current, the surgeon can complete the lymphadenectomy with minimal risk of neural or vascular injury. The remaining pelvic lymph nodes at this point lie along the medial aspect of the common iliac and hypogastric arteries. Again, these nodes are grasped and the ABC is used to coagulate and dissect this tissue off the vessels.
DEVELOPMENT OF THE RECTOVAGINAL SEPTUM AND RESECTION OF THE UTEROSACRAL/CARDINAL LIGAMENTS.
The proximal pelvic ureter is bluntly separated from the posterior leaf of the broad ligament. Care should be taken to identify the periureteral tissue, which may be as much as 1 cm anterior to the ureter. Dissection of this tissue along with the ureter minimizes bothersome bleeding and may reduce devascularization of the ureter. The ureter is pushed posteriorly and laterally in a distal direction to the uterine vessels. The posterior peritoneum can be incised down toward the uterosacral ligament. Working from a lateral-to-medial direction, the plane between the sigmoid colon serosa/mesentery and peritoneum is developed using short bursts of the ABC current. This point is not often addressed, but we have found that by beginning this dissection laterally, there is little difficulty in identifying this plane and separating the rectum from the vagina. The peritoneum over the posterior uterosacral ligament can then be incised safely. The rectovaginal septum is entered and the rectum is dissected off of the posterior aspect of the vagina. Again, small amounts of argon gas are insufflated in this region by tapping the foot pedal in very short bursts; this infuses the argon without deploying the unipolar current and greatly facilitates opening this space in a relatively bloodless fashion. A gauze Raytec sponge also assists in bluntly developing this space.
The surgeon transects the uterosacral ligaments at the level appropriate to the individual case. The stapler is passed through the ipsilateral post, and the uterosacral ligament is divided with one or two purchases of the stapler on each side. Alternatively, if a fifth port is in place, the laparoscope is placed through the upper port and the stapler passed through the periumbilical port. The ureter must be visualized and retracted laterally before the stapler is closed and activated. The cardinal ligaments are similarly transected with the stapler; again, the extent of the resection can be individualized. It should be stressed that we attempt to maximize the amount of the cardinal and uterosacral ligaments resected before the ureteral dissection. In our opinion, this approach shortens the operative time by facilitating the surgeon's ability to place the uterus on sufficient traction and thereby delineating the dissectional planes important to this portion of the procedure.
DEVELOPMENT OF THE VESICOVAGINAL SPACE AND URETERAL DISSECTION.
The ABC is used to develop the vesicovaginal space by pressing the tip on the underside of the peritoneal edge near its reflection from the bladder onto the cervix. The pedal is tapped as described above. The ABC then transects the vesicovaginal peritoneum, and an Endoscopic Blunt Tip Dissector (Ethicon Endo-surgery) is used to separate the bladder from the cervix and upper vagina. Small blood vessels are coagulated with the ABC.
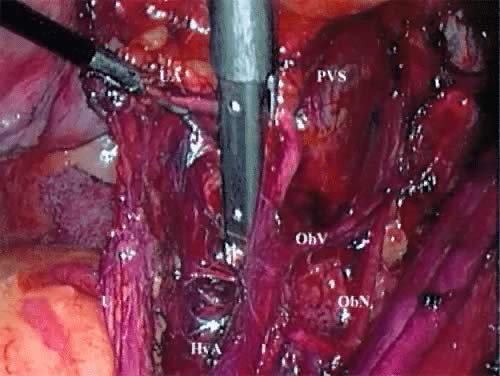
The ureteral dissection is now performed. As the scrubbed technician elevates the uterus to the side opposite the dissection, the assistant surgeon retracts the ureter laterally and somewhat posteriorly. The surgeon then grasps the transected uterine artery and places medial traction on it. The ABC is used to coagulate and dissect the periarterial tissue over the ureter. The vesicouterine sheath is next incised while the ureter continues to be placed on posterolateral traction. A helpful maneuver in developing this space is placing the tip of the ABC directly on top of the ureter and retracting firmly in a distal and anterior direction. The ureter can then be rolled and retracted laterally. In attempting to complete this dissection with unipolar surgical instruments such as shears, the surgeon needs to exercise exceptional care because unintentional, if not unavoidable, contact can be made with the ureter. The position and magnification provided by the laparoscope/camera are great assets here in safely completing the ureteral dissection. Occasionally, a vessel in the area measuring greater than 3 mm is encountered and requires clips to be used for hemostasis.
RESECTION OF THE UPPER VAGINA.
Before the medial aspect of the parametria and paracolpos is resected, the bladder is dissected away from the distal vagina using the ABC. The surgeon places her or his nondominant hand into the anterior vaginal fornix and tents the vagina anteriorly. This maneuver not only facilitates the dissection by increasing the countertraction; it also assists in determining the extent of dissection needed to achieve adequate vaginal margins. The EndoGIA (U.S. Surgical) is again used to transect the paravaginal tissue. The stapler is passed through the suprapubic port to establish the lateral margin and then from the lateral port to establish the distal margin of resection. Consecutive purchases with the stapler are taken until the vagina is encountered. When the bladder has been satisfactorily advanced off of the top of the vagina, an anterior colpotomy is performed either with the ABC or with laparoscopic scissors connected to unipolar current. This is one of the few instances during this procedure in which the ABC may cause extra char to the tissue. Once the anterior colpotomy is performed, grasping the cervix laparoscopically and placing upward traction on it allows for rapid completion of this step. The sound and tenaculum are removed at this time. Although the simplest step conceptually, this is often the most difficult step because the maintenance of the pneumoperitoneum becomes problematic once the colpotomy is started. Prior solutions included packing the vagina with a moistened laparotomy sponge or a partially filled surgical glove or using a balloon/manipulator, all placed into the vagina. With the advent of the 30 L/min insufflator, we are able to maintain adequate pneumoperitoneum by closing all open trocar vents and having the scrubbed technician manually approximate the labia majora. The specimen is now completely freed and easily removed by grasping it with a tenaculum brought through the vagina.
CLOSURE OF THE VAGINAL CUFF.
Laparoscopic vaginal cuff closure is accomplished with an EndoStitch suturing device placed through the suprapubic port. A 48-inch 0 or 2-0 Polysorb suture is cut to approximately 12 inches, and a small loop is tied to the end of the suture. The flat-surfaced graspers are passed through the lateral ports; they are more effective in grasping the suture and providing tension on the suture. The first stitch incorporates both sides of the vaginal angle opposite to the surgeon, with the needle passed through the looped end. With the assistant pulling the end of the suture laterally and slightly posteriorly, the vagina is closed in a running fashion and tied laparoscopically.
AORTIC LYMPHADENECTOMY.
An aortic lymphadenectomy can be performed based on surgeon preference. We typically do this procedure first after placing and securing the laparoscopic trocars. This is because the bowel is least active immediately after induction of anesthesia and can be retracted easiest into the upper quadrants. The right-handed surgeon stands on the patient's right side for this part of the procedure. The video monitors are placed at the head of the table at 45 degrees to the patient's clavicles, and the laparoscope is placed through the suprapubic port. We reported a significant decrease in our operating times when the video monitors were thus positioned for the aortic lymphadenectomy.21
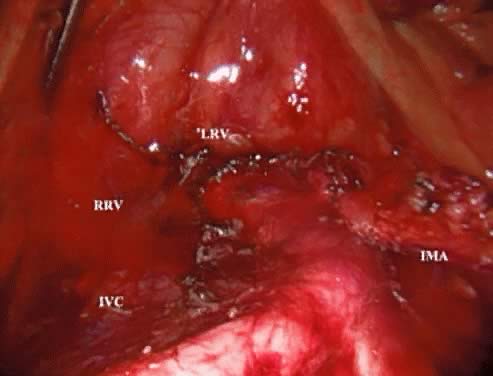
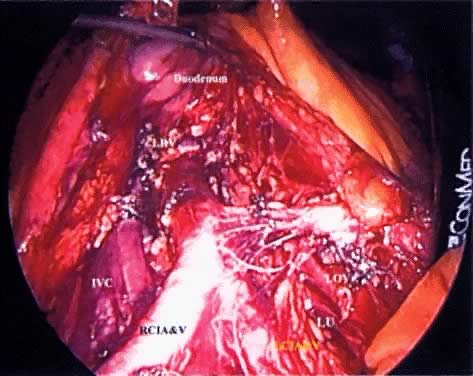
A peritoneal incision is made with the ABC by grasping the peritoneum over the proximal right common iliac artery and aortic bifurcation and extending it superiorly to the level of the IMA. The argon gas helps to dissect this retroperitoneal space and identify any small perforating vessels. Continuing the incision across the midline just above the IMA mobilizes the duodenum. The assistant places a grasper through the left lateral trocar and elevates the third portion of the duodenum by pushing it superiorly and laterally. A gauze Raytec sponge can be placed posterior to the duodenum to assist in elevating it. These maneuvers provide excellent exposure of the vena cava, lower aorta, and right common iliac vessels (Fig. 3).
After the right ureter is identified, the lymph-node-bearing tissue overlying the distal vena cava and right common iliac artery is grasped and the ABC is used to coagulate small perforators entering the nodal fat pad as well as the small lymphatics. The dissection continues in the interspace between the vena cava and aorta. The nodal tissue is retracted superiorly and laterally to the right. This provides an excellent way to identify a small vein commonly found, which drains the fat pad into the vena cava. Once identified, this vessel can almost always be coagulated or clipped. When using the ABC or any unipolar source, the surgeon should take care to apply the current to the vessel nearest to the nodal side as contrasted with the vena cava side.
The first step in removing the left aortic lymph nodes is identifying the origin of the IMA and then incising the peritoneum distally, which parallels the IMA into the pelvis. This incision allows for elevation of the IMA away from the aorta. Using the ABC bluntly, this dissection is performed until the left ureter and psoas muscle is identified as the lateral border of the dissection. The surgeon gently elevates and pushes the IMA and the attached mesentery to the left with a grasper in the right lateral port, and the assistant surgeon grasps the nodal bundle lateral to the aorta. Using the ABC, the aorta is retracted to the right, and the lymphatic attachments are coagulated and resected.
CLOSURE OF THE TROCAR SITES.
While the trocars are still in place, an EndoClose is passed on either side of the trocar with a 0-Polysorb suture loaded in the carrier. The suture should be passed though the fascia and not the skin. Once the sutures are placed, each trocar is closely removed while reapproximating the fascia. This is confirmed by digital examination. In our opinion, the last trocar to be removed should be the suprapubic because it is located in the least likely location for bowel herniation as the incision virtually abuts the pubis. The laparoscope allows for direct inspection of the closure of the other trocar sites.
PLACEMENT OF DRAINS.
If placement of a pelvic drainage system is planned, the top (nondrain) end of a 12- to 15-mm Jackson-Pratt drain is easily passed through either of the lateral ports, grasped from the opposite port, and pulled through to the appropriate length on the opposite side. The drain end can then be placed to the desired site of drainage with the laparoscopic graspers. The sutures closing the fascial defects should be placed before the drains are placed to avoid pulling the drain through the skin when the trocar is pulled out. This can lead to a problem in re-establishing the pneumoperitoneum as well as closing the trocar site. Then, as the drains are pulled through, the trocar can be removed and the suture knotted. The skin can then be either stapled or sutured with 4-0 Polysorb suture.
 menopausal score (M)
menopausal score (M)