Most men with infertility are eugonadotropic, normally virile, and otherwise
healthy, but they have low sperm density (< 15 million/mL) or
other seminal abnormalities. No specific etiology is known, but a variety
of fundamental defects in spermatogenesis is suspected. As one might
expect when the etiology is unknown, a multitude of empiric therapies
have been tried, unfortunately with limited success. Whereas in the
past many of these men would be destined to be childless and would eventually
be obliged to resort to donor insemination or adoption, IVF
and the new micro-assisted fertilization techniques offer the opportunity
to father children even in the most severe cases. Empiric Therapy Empiric therapies have included: androgens, gonadotropins, antiestrogens, GnRH, and
antiprostaglandins and pentoxifylline. Success has been limited, and
placebo-controlled studies have been few. ANDROGENS. Androgens have been administered in a variety of ways to enhance spermatogenesis. However, when
comparative studies have been performed using
placebo controls, androgens have not been shown to be effective. One
method was to deliver, over a period of at least 3 months, low doses
of androgen (methyltestosterone 10 to 50 mg/day), with the idea of replacing
a supposed testosterone deficiency. Androgens administered in this
fashion did not improve fertility.52 High-dose androgen therapy (testosterone enanthate, 200 mg to 500 mg intramuscularly
every 2 weeks) is given to suppress spermatogenesis for
a time, with the hope that after discontinuation sperm production will
rebound to levels higher than presuppression levels. The high levels
of testosterone suppress LH and thus spermatogenesis. Although spermatogenesis
usually rebounds somewhat after pituitary suppression with testosterone, fertility
is not increased.53 Two recent placebo-controlled studies of men with oligospermia, asthenospermia, or
teratospermia also found no benefit of androgens compared
with placebo with respect to either improvements in seminal parameters
or pregnancy rates.54,55 GONADOTROPINS AND GONADOTROPIN-RELEASING HORMONE. The administration of exogenous gonadotropins (hCG, hMG) to men with idiopathic
oligospermia has not been demonstrated to be beneficial.26 In a placebo-controlled study by Knuth and associates, using a combination
of hCG and hMG, neither semen parameters nor pregnancy rates were
enhanced compared with placebo.56 Furthermore, in a recent study, it was noted that treatment of men with
FSH did not significantly improve pregnancy rates.57 Likewise, GnRH treatment of idiopathic oligospermia has not been shown
to be effective.58 ANTIESTROGENS. Clomiphene citrate and tamoxifen are antiestrogens that exert their action
by competing with estrogen for the estrogen receptors. They enhance
gonadal function by reducing the negative feedback of estrogen at hypothalamic
and pituitary levels, resulting in increased GnRH activity, gonadotropin
secretion, production of testosterone, and hopefully, improved
spermatogenesis. Estradiol is known to have a direct inhibitory
effect on the Leydig cells, and the antiestrogens may enhance testicular
function by this mechanism as well. Another antiestrogen, testolactone, similarly
promotes testicular function both centrally and directly
by decreasing the influence of estradiol. However, it does not function
by competition for the estrogen receptor but by directly decreasing
the conversion of androgen to E2 through aromatase inhibition. Uncontrolled studies have reported improvement in sperm density and pregnancy
rates after clomiphene citrate treatment, whereas others have failed
to show benefit. However, when investigations have been well controlled, efficacy
has not been demonstrated.59,60 Sokol and colleagues61 prospectively compared clomiphene citrate (50 mg/day) and placebo, each
given for a 12-month period, in a group of 21 oligospermic men. They
found no differences between the clomiphene and placebo groups with respect
to either sperm counts or pregnancy rates. Interestingly, over
the time of the study, both groups experienced a gradual increase in sperm
density. However, a randomized, double-blind study of nearly 200 couples
by the World Health Organization showed no effect of clomiphene
treatment.62 Investigation of tamoxifen and testolactone as treatment for idiopathic
oligospermia has shown mixed results. There have been studies using tamoxifen (e.g., 20 mg/day for 4 to 12 months) that have shown improvement in sperm counts
and increased pregnancy rates, but they were not placebo-controlled.63 In contrast, a placebo-controlled study by AinMelk and colleagues demonstrated
no difference in pregnancy rates.64 Likewise, testolactone (e.g., 1 g/day for 6 to 12 months) has shown some promise in uncontrolled studies,65 but in a placebo-controlled crossover study, no efficacy for testolactone
was found.66 ANTIPROSTAGLANDINS. It has been suggested that antiprostaglandins improve spermatogenesis. In
a controlled study by Barkay and co-workers, indomethacin (50 to 75 mg/day
for 60 days) was found to improve significantly both semen parameters
and pregnancy rates compared with no improvement in the placebo
group.67 The best results (pregnancy rate of 36%) were obtained at the 75-mg dose. These
results need to be confirmed by additional controlled studies. PENTOXIFYLLINE. A methylxanthine, pentoxifylline, is a phosphodiesterase inhibitor and, as
such, results in an increase in intracellular cyclic adenosine monophosphate (cAMP) levels, which are involved with sperm motility hyperactivation
and the acrosome reaction. Merino and associates68 noted that men receiving 1200 mg of pentoxifylline over 6 months demonstrated
a significant increase in sperm motility, which is in contrast
to the observations by Tesarik and colleagues.69 Thus, the empiric treatment of idiopathic oligospermia has met with limited
success, and when therapeutic regimens have been tested against placebo
controls, they generally have failed to demonstrate efficacy. Intrauterine Insemination Artificial insemination with husband semen has been used to treat infertile
couples for almost 200 years. It is an accepted form of treatment
for men with severe hypospadias, retrograde ejaculation, neurologic impotence, and
sexual dysfunction refractory to counseling. It also has
been used in the presence of oligospermia, asthenozoospermia, low or
high ejaculate volumes, and antisperm antibodies; however, the success
rate in these settings is low and the utility is open to review. The
technique also has been used in the presence of abnormal cervical mucus, stenotic
cervical canal, or antisperm antibodies in the female. The
desire to bypass poor cervical mucus, or to assist sperm transit in male-factor
infertility has led to the technique of IUI. Abandoned because
of serious allergic reactions, IUI with unprepared semen has been
replaced with IUI with “washed sperm.” There are a variety
of techniques designed to separate sperm from the other seminal fluids, remove
antibodies or debris, and isolate a fraction of sperm with optimal
motility and morphology. These include simple washing, where semen
is diluted into a volume of culture medium and centrifuged, the supernatant
decanted, and then the process repeated. The final product has
the seminal fluid portion removed but all sperm and cellular components
remain. The swim-up and Percoll techniques are designed to isolate
a population of sperm with better motility and morphology and thus higher
pregnancy rates.70 In the swim-up procedure, after washing and centrifugation, the specimen
is incubated, allowing the most motile sperm to swim up from the pellet
into the medium. The specimen for insemination is obtained from the
supernatant, rather than the pellet. It contains fewer sperm, but the
motility is enhanced. With the Percoll procedure, motile sperm are
separated differentially by means of their ability to traverse progressively
more dense layers of a viscous medium.71 The number of sperm for insemination should not be less than 1 million, and
pregnancy rates are not increased to greater than 15 million, although
the multiple pregnancy rate is increased to more than 20 million.72 However, others have not been able to demonstrate increased pregnancy
rates with IUI over timed intercourse in oligoasthenospermic infertility.73 Recently, IUI in conjunction with superovulation has become a popular treatment
for male-factor infertility, as well as unexplained infertility. The
combination of IUI and superovulation with gonadotropins has the
theoretical advantage of placing a greater number of motile and morphologically
normal sperm in close proximity to multiple mature oocytes. In
a group of patients with male-factor infertility or abnormal postcoital
tests, IUI plus superovulation resulted in a fourfold increase
in the pregnancy rate compared with IUI alone.74 In a study by Serhal and co-workers, the pregnancy rate/cycle was significantly
greater for the combination of IUI and gonadotropin superovulation (26.4%) than
for IUI alone (2.7%) or superovulation alone (6.1%).75 In a review of several studies, Dodson and Haney found the fecundity rate
with IUI and superovulation in male-factor infertility was 8.7%; for
unexplained infertility, it was 17%.76 It appears that IUI alone or superovulation alone is not effective, but
the combination may offer some limited benefit to patients with male-factor
infertility.77 Donor Insemination For couples who have failed to conceive despite therapy or those with extreme
idiopathic oligospermia, donor insemination offers the couple an
alternative to adoption. In the absence of contributing female-factor
infertility, donor insemination is extremely successful (70% with 5 to 6 cycles). If
donor insemination is unacceptable and adoption is not
desired, the male who wants to pursue having his own genetic offspring
can avail himself of the new reproductive technologies: IVF and micro-manipulation. Sperm Retrieval Techniques for In Vitro Fertilization and Micro-Assisted
Fertilization There are a variety of techniques involved in the retrieval of spermatozoa
for utilization in IVF and micro-assisted fertilization, such as ICSI. This
includes: masturbation, electroejaculation/vibratory stimulation, percutaneous
epididymal sperm aspiration (PESA), microsurgical epididymal
sperm aspiration (MESA), and testicular sperm extraction (TESE). Masturbation
requires 2 to 3 days of abstinence before production
of the sample, which subsequently undergoes sperm preparation before
use. Electroejaculation/vibratory stimulation requires the use of a device
and urinary alkalization in patients with ejaculatory dysfunction
to produce an adequate sample. PESA and MESA are used in men with azoospermia
secondary to obstructive and nonobstructive disorders. PESA involves
local anesthesia and multiple blind passages with a 21- to 23-gauge
needle through the epididymis, with the advantage of avoiding a
skin incision. However, the disadvantage is the “blind” nature
of the procedure, which may cause significant damage to the epididymis, making
future attempts at conception difficult. Conversely, MESA
provides retrieval of many sperm, with less epididymal damage, which
then may be cryopreserved and used for future procedures.78 TESE involves an open surgical biopsy of the testicle when epididymal
sperm retrieval is unable to occur and provides similar pregnancy rates
when using micro-assisted fertilization.79 In Vitro Fertilization In vitro fertilization and its micromanipulative innovations show promise
of being an advance for male infertility on the level that traditional
IVF has been for female tubal infertility. The concept of IVF originated
with the desire to treat infertility caused by failed gamete union
secondary to tubal obstruction. The first successful in vitro manipulation
of gametes by conventional IVF occurred with the birth of Louise
Brown in England in 1978. Although the methodology of processing and
storing sperm had been available for many years, the ability to recruit, collect, and
culture oocytes was required before the possibility
of enhancing fertilization by the in vitro incubation of gametes became
possible. Since the delivery of the first baby some 21 years ago, the
technique has spread worldwide, and consistent results are now obtained. Moreover, the
indications soon expanded to include unexplained infertility
and male factor. Although it was logical that inseminating
oocytes in vitro would facilitate fertilization, the number of motile
sperm originally used for insemination (2 to 6 million/oocyte) limited
application of the technique in oligospermic infertility. With time and
experience, the number of motile sperm used for insemination has declined (50,000 to 100,000/oocyte) with maintenance of fertilization rates
and tolerable levels of polyspermic fertilization.80 This development opened the door for treatment of the oligospermic male
using IVF. Additionally, controlled ovarian hyperstimulation with hMG
allows the recruitment of multiple ovarian follicles and retrieval of
multiple oocytes, which then can be inseminated using processed sperm
from the male partner. CONVENTIONAL IN VITRO FERTILIZATION AND THE OLIGOSPERMIC MALE. Male-factor infertility is the indication for approximately 25% of IVF
cycles. Oligospermia, abnormal morphology, and motility adversely influence
fertilization rates.81 However, once fertilization has occurred, the implantation rate per transfer
is equal to that of other IVF patients.82,83 Fertilization rates for male-factor IVF have been reported by Tournave83 and Cohen84 to be 30% and 53%, respectively. However, the overall pregnancy rate for
IVF in the United States as reported by the Society for Assisted Reproductive
Technology is 18% for male infertility.85 The national IVF registry has demonstrated consistently an increased chance
of failed fertilization in male-factor infertility (50%) compared
with tubal infertility (15%). These low fertilization rates result in
fewer embryos for transfer and a lower overall success rate (deliveries/retrieval).86 Failure of fertilization at IVF is devastating to the infertile couple. The
financial and emotional investment is of such magnitude that even
when it is anticipated because of known severe andrological infertility, the
disappointment is great. What can the patient be offered after
failed fertilization, and what of the patient with such extreme semen
abnormalities that even conventional IVF is not a consideration? Several
new techniques have been developed to assist the fertilization process, some
of which promise to make conceiving a pregnancy a reality for
even the most severe oligospermic, asthenospermic, and teratospermic
males. When there is failure of fertilization at IVF or when a male
factor is anticipated or known, options include: gamete intrafallopian
transfer (GIFT); repeat conventional IVF; modification of sperm concentration; and
micro-assisted fertilization. Although recommended by some, the
use of a second sperm sample (husband/partner or donor) to reinseminate (rescue) oocytes
that have failed to undergo fertilization has
not proven efficacious. INTRAFALLOPIAN TRANSFER PROCEDURES. In nontubal infertility, intrafallopian transfer procedures have gained
popularity because of modestly increased clinical pregnancy rates compared
with IVF (25% vs. 10%). It is not clear whether these results are
due to the benefits of the in vivo tubal environment or whether they
only reflect differences in patient selection. The rationale for GIFT
is that the oviduct, being the natural location for fertilization, offers
the optimal environment. In nonmale-factor patients, the usual number
of sperm placed with the oocytes in the oviduct is 100,000. In male-factor
cases, some investigators suggest the use of increased sperm
numbers (325,000 sperm/oviduct),82 whereas others report using reduced numbers (2,500/oviduct).87 It is likely in these cases that the criteria used to define a male factor
are different. Indeed, in retrospect, a male factor may not even
exist because functional sperm are clearly present. A drawback with GIFT
is that in the absence of pregnancy, fertilization cannot be confirmed. Thus, some
investigators perform fertilization in vitro and then
transfer the zygote to the fallopian tube. In one study of 78 planned
zygote intrafallopian transfer (ZIFT) cycles, failure of fertilization
was observed in 34 (43.6%). These results would not have been available
if GIFT was the planned procedure, and perhaps 34 patients would have
undergone unnecessary laparoscopy.88 Although some retrospective studies have shown advantages of ZIFT over
IVF, a prospective, randomized study comparing IVF and ZIFT found no advantage
of ZIFT over IVF for the treatment of male-factor infertility.88 In a comparison of IVF, GIFT and ZIFT, Tournaye and associates reported
take-home baby rates of 13.5%, 7%, and 20%, respectively.89 These results were not different statistically. Furthermore, with ZIFT, one-cell
zygotes are transferred before determination of pronuclear
stage arrest or cleavage failure, both of which are more common in male-factor
infertility83; thus, not permitting embryo preselection, as has been shown advantageous
in IVF.90 Both ZIFT and GIFT have the added disadvantage of requiring laparoscopy
and general anesthesia for transfer with consequent increased cost. The
possibility of transcervical-intrafallopian transfer91 of cleavage-stage embryos could impact the success and cost equation, but
the efficacy of these procedures has yet to be determined. Thus, conventional IVF provides advantages in cost and convenience when
compared with GIFT or ZIFT, and success rates probably are not significantly
different. If GIFT is considered, it should be limited to cases
of mild to moderate male-factor infertility, where fertilization potential
is known or expected to be good. REPEAT CONVENTIONAL IN VITRO INSEMINATION. Studies have noted that of male-factor patients who had one IVF cycle
with failed fertilization, 81% had achieved successful fertilization after
another cycle. However, with the new micro-assisted fertilization
techniques such as ICSI, with more effective fertilization and pregnancy
rates yet slightly higher costs, many clinicians have recommended
going directly to these procedures rather than IVF.92 HEAVY CONVENTIONAL INSEMINATION. Although concentrations of 50,000 to 100,000 sperm/mL are customary for
conventional IVF, much higher concentrations are appropriate for male-factor
infertility. Several groups recommend that in the presence of
severe male-factor infertility or conventional IVF fertilization failures, patients
undergo an IVF cycle with “heavy” conventional
insemination. The effective sperm concentration can be as high as 1 to 5 million/mL.93 Tucker and colleagues93 reported 53% fertilization and 36% viable pregnancy rates with heavy conventional
insemination in a series of patients with severe male-factor
infertility or previous fertilization failure. They recommend that
all but the most extreme oligospermia undergo heavy insemination before
proceeding to micromanipulation. When oligospermia is severe and insufficient
sperm are available, these concentrations frequently can be
obtained using the microdrop technique. Sperm concentrations of 1 million/mL
can be obtained by placing as few as 25,000 cells in 25-mL droplets
of medium under oil. Bayer and co-workers have had success with this
technique in the presence of severe male-factor infertility.94 Another technique that can be employed when sperm numbers are limited
is to inseminate multiple oocytes in a single dish. Fertilization can
be enhanced further in male-factor cases by inseminating with not only
a high concentration of sperm but with a highly motile population as
well. Special procedures (e.g., mini-Percoll), designed to separate a highly motile subpopulation of
sperm have evolved for this purpose.95 Micro-Assisted Fertilization Although conventional IVF has been very helpful in treating couples with
long-term andrological infertility, there are patients with severe male-factor
infertility (extreme oligospermia, absence of normal morphology, and
motility), and fertilization failure patients with no currently
detectable semen abnormalities, who are appropriately considered for
treatment by more aggressive techniques. Philosophical extremes still
exist in deciding which patients should be considered for micromanipulation: a
last resort procedure or one appropriate for all suspected
or diagnosed male-factor infertility. These techniques involve the use
of micromanipulators to mechanically assist the sperm-egg interaction
process. THE MICROMANIPULATION TECHNIQUE. Under visualization on the stage of an inverted microscope, oocytes in
culture medium droplets under oil are held and micromanipulated with
specially prepared holding and injection pipettes. The oocyte is immobilized
with gentle suction applied by the holding pipette, and the injection
pipette is used to incise the zona pellucida (ZP), deposit several
sperm in the perivitelline space, or inject a single sperm directly
into the ooplasm. These techniques can be classified as: zonal, subzonal, and
intracytoplasmic procedures. Although known by many names such
as zona drilling, subzonal insertion, and direct egg injection, the
following terms are used in this chapter: partial zona dissection (PZD), subzonal
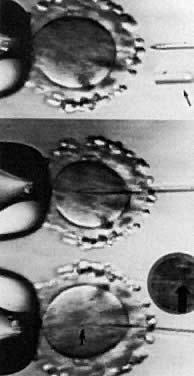
injection (SUZI), and intracytoplasmic sperm injection (ICSI) (Fig. 2).  Fig. 2. Micro-assisted fertilization. Metaphase II oocyte illustrating microsurgical-assisted
fertilization techniques: PZD, incision in ZP to facilitate sperm entry: SUZI, injection of a few sperm into perivitelline space; ICSI, injection of a single sperm into the ooplasm. Fig. 2. Micro-assisted fertilization. Metaphase II oocyte illustrating microsurgical-assisted
fertilization techniques: PZD, incision in ZP to facilitate sperm entry: SUZI, injection of a few sperm into perivitelline space; ICSI, injection of a single sperm into the ooplasm.
|
PARTIAL ZONA DISSECTION. Before fertilization can occur, sperm must penetrate the ZP, traverse
the perivitelline space, and fuse with the oolemma in the process of entering
the ooplasm. The ZP, an acellular glycoprotein coat surrounding
the oocyte, plays several roles in fertilization and early development, including
the provision of a species-specific barrier to fertilization, a
barrier to polyspermia, and a protective shell for the preimplantation
embryo. Because ZP passage represents a prerequisite step for
the fertilizing sperm, the creation of gaps or slits in the zona should
facilitate this process (see Fig. 2). Oocytes dissected in this manner are inseminated subsequently with standard
concentrations of capacitated sperm. Chemical, mechanical, and
laser techniques have been employed. The ZP was first opened using acidified
Tyrode's solution delivered through a microneedle (zona drilling). This
process was successful in mice but not when applied in
human IVF because of induced oocyte damage. In 1988, the first human pregnancy
was produced from microsurgical fertilization using a micropipette
to mechanically open the ZP (PZD).96 To minimize damage to the oocyte during this process, limited shrinkage
is induced by conducting the procedure in sucrose. The technique usually
involves placing the micropipette through the ZP into the perivitelline
space and then continuing out through the opposite side of the
ZP without entering the ooplasm. Releasing the oocyte from the holding
pipette, the ZP overlying the micropipette is rubbed against the side
of the holding pipette until a slit is created in the ZP. Other investigators
have advocated using laser for PZD because of its simplicity
and precision.97 However, the overall success of PZD has been limited. It is estimated that
only 100 to 150 live births have resulted from the method.98 In a comparative study involving 130 male-factor cycles, no differences
were found between IVF and PZD with respect to fertilization (12% vs. 13%); the
cleavage rate was higher for the IVF group (89% vs. 73%); and
the pregnancy rate for IVF was 33% compared with 12% for PZD.99 The conclusion was drawn that PZD was no better than conventional IVF. Furthermore, PZD
is complicated by excessive rates of polyspermia, variously
reported at 30% to 47%. Although rates of polyspermia may be modulated
by patient selection, gap size, and sperm concentration, results
have been inconsistent. In most centers, the implantation capacity
also is reduced, most likely because of oocyte damage during the procedure (2%–30%), or
improper culture conditions during the micromanipulation (temperature
and pH). These problems and inconsistent results
have led many investigators to abandon PZD.100 SUBZONAL INJECTION. The second generation of micromanipulation techniques includes SUZI or
the direct subzonal insertion of sperm through and under the zona pellucida
into the perivitelline space (see Fig. 2). Depending on their morphologic appearance, several sperm (3 to 6) are
aspirated into a sharp, bevelled microneedle and injected through the
ZP. Because the ZP and its ZP3, the zona glycoprotein implicated in
acrosome reaction induction, are bypassed in this process, strategies
to prematurely induce the acrosome reaction have been conceived. Two methods
designed for this purpose are: washed sperm incubated for 24 hours
in Tyrode's medium + 50% follicular fluid, and electroporation + incubation
in 3.5 mmol/L pentoxifylline.101 Although these procedures increase the acrosome-free sperm to as high
as 54%, their efficacy remains unproven. Indeed, motile sperm in the perivitelline
space still may be exposed to ZP3 present on the inner aspects
of the zona. In theory, increasing the number of reacted sperm should
allow the use of fewer sperm (3 vs. 6), thereby decreasing the risk
of polyspermic fertilization. Unfortunately, the clinical success with SUZI has been less than spectacular, with
fertilization rates hovering around 20% and pregnancy rates
around 10%.102,103 The drawbacks of SUZI are the same as those for PZD: polyspermic fertilization
and impaired implantation. Because the oolemma cannot block multiple
sperm fusion, SUZI is inherently complicated by polyspermic fertilization. The
fertilization rate with SUZI can be increased by increasing
the number of sperm placed in the perivitelline space, but the
proportion of polyspermic embryos may become unacceptably high. However, polyspermia
may be lower than with PZD103 and can be influenced by the number of sperm inserted. Implantation rates
with SUZI embryos also may be better than for PZD.84 Likewise, the risk of blastomere or cytoplasm extrusion and contamination
of the perivitelline space with medium is reduced with SUZI (smaller
gap). However, this technique recently has been superseded by ICSI. INTRACYTOPLASMIC SPERM INJECTION. The next logical step was to use micromanipulation to inject a single
sperm through the ZP and oolemma directly into the ooplasm (see Fig. 2). Although the most invasive technique, the inherent advantage to ICSI
is avoidance of polyspermic fertilization because only one sperm is injected. Initial
concerns with ICSI centered on whether the cytoskeleton
would be disrupted, causing defective cell division (minimized by injecting
distal to the meiotic spindle); whether fertilization would occur
with genetically abnormal sperm; and whether oocyte activation (completion
of the fertilization process, initiation of cleavage, and development), if
triggered, would be normal. In animals, the ICSI procedure
has not always resulted in activation, and various treatment regimens
have been developed to overcome this limitation. For instance, oocytes
can be activated by exposure to ethanol, calcium ionophore, or electrical
fields (electroporation). The common mediator with these methods
is most likely elevation of intracellular calcium ion concentration, either
by extracellular calcium influx or by intracytoplasmic mobilization
of calcium stores.104 It has become apparent that injection of a single sperm into the cytoplasm
is sufficient stimulus in humans to trigger activation. In addition, the
increased intracellular calcium associated with the injection
process does not, in and of itself, provoke egg activation,105 but rather, the release of a sperm factor appears to be required. Interestingly, an
intact acrosome is not a deterrent to ICSI success. Although preclinical trials of ICSI established that fertilization could
be obtained,106 clinical pregnancies were not reported until 1992.107 High fertilization and pregnancy rates with ICSI currently are routine
in several centers around the world.98 The most extensive experience has been realized in a program in Brussels.108 In their ICSI technique, sperm either were incubated overnight, treated
with pentoxifylline and deoxyadenosine, electroporation, or were exposed
transiently to elevated calcium levels to increase the chance for
fertilization. These recipes for success have been largely abandoned. Percoll-gradient
processed sperm are dispersed in polyvinylpyrrolidone, a
viscous solution that allows separation of motile sperm from immotile
cells, specifically in conditions of severe oligoasthenozoospermia.109 Subsequent immobilization of the spermatozoa by various techniques, such
as crimping the tail of the spermatozoa at the tip, allows for delivery
into the micropipette.110 Beveled, injection micropipettes (7 μm outer and 5 μm inner diameter) then
are front-loaded tail first, with the resultant immobilized
spermatozoa for injection into the ooplasm (Fig. 3).108 In men with complete asthenozoospermia, there are no motile sperm and
less than 50% of the sperm are viable. As a result, the hypo-osmotic swelling
test was developed and used to enhance fertilization and pregnancy
in these patients, as well as in previously cryopreserved sperm that
usually have poor motility. When sperm are incubated in a hypo-osmolar
medium, those that are viable and functional undergo swelling of
the cytoplasmic space and the sperm tail fibers curl. These sperm in turn
may be used in ICSI and provide a better outcome.111 The indications for ICSI are the absence of fertilization, a failure to
fertilize in a previous cycle of IVF, antisperm antibodies, teratozoospermia, sever
oligoasthenozoospermia, obstructive azoospermia, such
as with congenital bilateral absence of the vas deferens, nonobstructive
azoospermia, and anejaculation.112 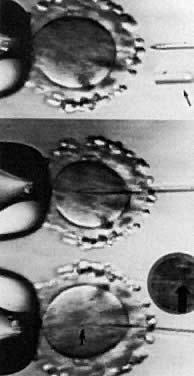 Fig. 3. Intracytoplasmic sperm injection. Top: metaphase II oocyte just before insertion of micropipette containing single
sperm (magnified sperm head in pipette, arrow). Middle: micropipette inserted into ooplasm. Bottom: single sperm in center of ooplasm after injection (arrowhead; magnified sperm head inset, arrow). Fig. 3. Intracytoplasmic sperm injection. Top: metaphase II oocyte just before insertion of micropipette containing single
sperm (magnified sperm head in pipette, arrow). Middle: micropipette inserted into ooplasm. Bottom: single sperm in center of ooplasm after injection (arrowhead; magnified sperm head inset, arrow).
|
In the early developmental phase of the ICSI procedure, a comparison of 750 cycles
of ICSI and SUZI was conducted, and a fertilization rate of 55% for
ICSI versus 17% for SUZI was obtained.108 ICSI quickly was adopted as the standard assisted fertilization treatment
for couples unable to benefit from conventional IVF. Palermo and associates
have noted in their experience of 355 cycles with 2,970 injected
oocytes that greater than 93% of the oocytes remained intact after
the procedure, with a 69% fertilization rate and a 38% ongoing pregnancy
rate achieved per oocyte retrieved.113 Another series by Ubaldi and co-workers114 from Brussels consisted of 2,820 cycles of ICSI; greater than 95% of the 36,425 oocytes
remained intact, and the pregnancy rate approximated 38%. This
study also detailed no significant difference between the pregnancy
rates per cycle with ejaculated, epididymal, and testicular sperm. Others
also have been successful with ICSI (fertilization rate > 50%) and
have recommended using ICSI any time the predicted fertilization
rate from heavy conventional insemination is less than 40% These
authors reason that the majority of failed fertilization is because
of specific severe defects, such as teratozoospermia, oligospermia, asthenozoospermia, or
acrosomal defects, which affect sperm/ZP binding.115 Although concerns about disruption of chromosomal or cytoskeletal elements
or the consequences of fertilization with genetically abnormal sperm
continue, confidence is accumulating that clinical outcomes will be
normal. In infertile men, approximately 7% have a major sex chromosome
abnormality, half of which are accounted for by a mosaic Klinefelter
condition. The incidence rises from 2% in men with normal sperm concentration
to 20% in those with azoospermia.116 Despite these data and an apparently high risk for chromosome abnormalities
in ICSI fetuses, Bonduelle and colleagues found the risk of chromosomal
abnormalities to be approximately 1%, similar to the general newborn
population.117 Furthermore, the early pregnancy loss rate has been approximately 19%, and
fetal karyotypes performed on 151 patients for prenatal diagnosis (amniocentesis
or chorionic villus sampling), and examination of 119 children
after birth did not reveal an increase in congenital anomalies.108 Sperm employed for ICSI can be morphologically very abnormal; pregnancies
have occurred with very low counts, 0% motility, 0% normal morphology, as
well as with cryopreserved sperm. In fact, in situations of previously
diagnosed primary testicular failure with FSH levels greater
than 30 mIU/mL, nearly 50% of men had mature sperm on testicular biopsy
suitable for ICSI.118 In addition, application of round spermatid nuclei injection (ROSNI) in
humans is undergoing careful consideration, with fertilization rates
of approximately 30%, two pregnancies, and resultant childbirth.119 Because ICSI allows fertilization by sperm, which under natural conditions
are incapable of ZP penetration and oocyte-sperm fusion, concern
also exists that germ-line mutations might be transmitted, resulting in
heritable defects. The inheritance of susceptibility to infertility
is another concern and would not be recognized until late in the next
generation (the reproductive years). Once sexing of the spermatozoa becomes
routinely available, prevention of sex-linked diseases may be preventable
by selecting the healthier gender. Thus, careful evaluation, genetic
consultation with the couples, and follow-up of the pregnancies
resulting from ICSI are necessary. |
 = low,
= low,  = high, nl = normal).
= high, nl = normal).