Performing preimplantation diagnosis has two technical components: removal of cells from the oocyte or embryo and the genetic diagnosis itself. Biopsy can be carried out on cells from the oocyte (polar body biopsy) and from the preimplantation embryo (blastomere biopsy). Both approaches require artificial reproductive procedures (in vitro fertilization [IVF]) to generate oocytes and embryos in vitro. Polar body biopsy involves removal of the first and second polar bodies. Blastomere biopsy involves aspiration of 1 or 2 cells (preferably 2 cells) from the cleavage stage embryo 3 days after insemination. Preimplantation diagnosis for genetic disease must be sensitive and rapid because genetic information is derived from 1 or 2 cells and human embryos must be transferred within 5 days of aspiration (blastocyst stage) to achieve implantation and pregnancy.
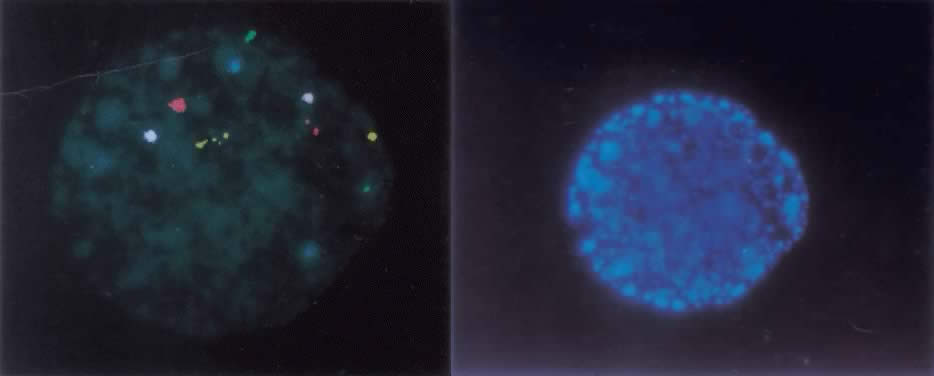
The ideal method of studying chromosomes has been by karyotyping. Cells are arrested in metaphase by preventing spindle fiber formation, fixed in an acidified solution, and then treated to enzymatic digests (e.g. trypsin) so that chromosomes could be banded and that numeric and structural chromosome aberrations detected. To obtain metaphase chromosomes from polar bodies and cleavage-stage human embryos has been problematic, because these cells could not be cultured for extended periods of time (i.e. 2 to 3 days) and few cells were suitable for karyotyping. When metaphase chromosomes were obtained, the chromosomes were short and difficult to band. With the introduction of interphase fluorescent in situ hybridization, or FISH, examination of the chromosomes of every cell within an embryo became possible. FISH uses DNA probes that bind to specific regions of the target chromosomes. FISH probes directly labeled with different colored fluorochromes were developed which bind to the centromeric, or α satellite, regions of the X, Y, and 18 chromosomes, because each of their centromeres contained unique repeat sequences. After the nuclei chromatin had been denatured to separate the double-stranded DNA into single strands, the probes were then hybridized to their complementary strand. Because the fluorochromes were bound to the probes, a fluorescent dot was seen on the chromosome. Nuclei derived from sperm, oocytes, polar bodies, or blastomeres can be FISHed within two hours.1,2 For some chromosomes, however, centromeric sequences were not specific (e.g. the α satellite probe for chromosomes 13 and 21 cross hybridized and distinguishing the two chromosomes was not possible). When the number of signals indicated a numeric chromosome aberration, it was not possible to determine which chromosome was involved. In response to this technical problem, unique-sequence, single-copy FISH probes were introduced. Because they were specific for a single gene (i.e. locus specific), these probes were also chromosome specific. A significant disadvantage is that a limited number of chromosomes, usually no more than five, can be FISHed at one time, due to their close proximity within the interphase nucleus (Fig. 1).
Chromosome aberrations occurring during gametogenesis, fertilization, and preimplantation embryonic development are in large part responsible for implantation failure, spontaneous abortion, stillbirth, and live birth with congenital malformations. Only 30% of human embryos during natural cycle conception are estimated to be able to implant themselves and become viable.3 More than 20% of these embryos in natural cycle pregnancies are believed lost before the third week of gestation.4 The rate of chromosome aberrations in spontaneously aborted fetuses following IVF was not dissimilar to that in natural cycle conceptions and exceeded 60%.5 Karyotyping of human preimplantation embryos following IVF revealed that 37% were chromosomally abnormal.6 Numeric chromosome aberrations were present in 56.5% of arrested preimplantation embryos, using FISH probes for only three chromosomes (X, Y, and 18).7 Because only 5% of 7- and 8-week-old embryos were found to be chromosomally abnormal,8 most embryos with a chromosome aberration are presumed to be lost before being recognized as a clinical pregnancy.
This chapter reviews the origin and characteristics of chromosome aberrations in the preimplantation period with particular emphasis on their implications for the treatment of infertility by IVF and the preimplantation diagnosis of chromosome disorders.