FAMs include all family planning methods based on the identification of the fertile time.4 This knowledge can be used to plan or avoid pregnancy. FAMs depends on two key variables, the accurate identification of the fertile days of a woman's menstrual cycle (the fertile time) and the modification of sexual behavior, either to target intercourse to plan or to avoid a pregnancy.5
The effectiveness of FAMs to avoid pregnancy depends on the ability of couples to abstain from intercourse during the fertile time (natural family planning) or to use a barrier method consistently during the fertile time (fertility knowledge with barriers).
History of Fertility Awareness Methods
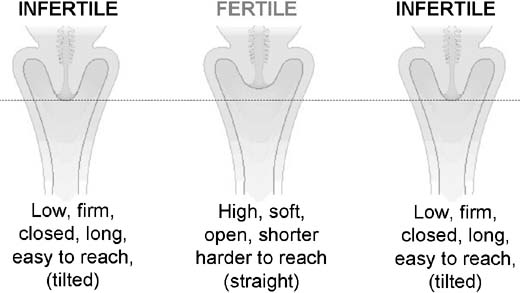
Men and women have been fascinated by reproductive physiology and ways to plan or avoid pregnancy throughout history. The scientific identification of the fertile time originated in the 1930s when Dr. Ogino in Japan and Dr. Knaus in Austria independently observed that ovulation occurred at a fixed interval of approximately 14 days before the next menstruation. This formed the basis of the rhythm or calendar method.6 In the 1950s, new methods of fertility control were developed based on the physiological signs of ovulation. Drs. John and Evelyn Billings in Melbourne, Australia pioneered a method based on the changes in cervical mucus secretions.7 Dr. John Marshall in London developed the temperature method.8 In the 1970s, Edward Keefe first described cyclic changes in the cervix.9 Over time it was realized that combining two or more of the fertility indicators resulted in a more effective method. Combining indicators has been variously described as the sympto-thermal method,10 the muco-thermic method,11 or the double check method.12
In 1972, the WHO established a task force on methods for the prediction and detection of ovulation. One of the major objectives was to develop an accurate, easy, and cheap test that could be used in the home to predict the start and end of the fertile time. WHO research13 on numerous markers of fertility found that the most accurate determinants of the start of the fertile time was the increase of oestrone-3-glucoronide (E-3-G) in urine, and the luteinizing hormone (LH) surge provides the most accurate marker of ovulation and predicting the end of the fertile time. In 1996, the first personal hormone monitoring system an immuno-chemical self-test was launched.14 While researching highly sophisticated and technologically advanced natural methods, the challenge still remained to provide reliable, simple, low-cost methods. The Standard Days Method (fixed formula)15 and the TwoDay Method16are recent developments in this area. Table 1 summarizes the key concepts in the understanding of the fertile time from the fourth century BC when jumping up and down was a popular contraceptive idea to the technological sophistication of the 21st century pinpointing the fertile time.
Table 1. The History of Fertility Awareness Methods of
Family Planning
| Dates | Key names | Development of physiological methods to avoid pregnancy |
| 4th C B | Hippocrates | Advised women to “jump so that the buttocks are touched by the feet” |
| 3rd C BC | Aristotle | Conception was most likely immediately before or after menstruation |
| 2nd C AD | Soranus | Conception more likely if the woman has an orgasm (dilates uterus); to avoid conception, women were advised to abstain during the fertile time (Aristotle's theory); hold their breath, not move during intercourse, move away before ejaculation; then get up immediately, squat, promote sneezing, wipe the vagina, and have a cold drink |
| 9th C AD | Rhazes | Advised women to rise roughly immediately after ejaculation, sneeze, and blow their nose several times and call out in a loud noise while jumping violently backwards |
| 1600 | Fallopius | Discovered and christened the Fallopian tubes |
| 1662 | Van Horne | The “female testicles” were renamed the ovaries |
| 1869 | Squires | Noted a decrease in a woman's basal body temperature at the onset of menstruation but did not appreciate the significance of the preceding rise |
| 1928 | Van de Velde | Related the higher temperature in the latter part of the cycle to the activity of the corpus luteum |
| 1928 | Ogino (Japan) Knaus (Austria) | Independently established that ovulation occurs 12 to 16 days before the onset of the next menstrual period |
| 1937 | Rubinstein & Lindsley | Related increase in basal body temperature to evidence of ovulation (vaginal smears), several researchers then correlated basal body temperature increase with other indicators of ovulation |
| 1950s | JGH Holt | A Dutch gynaecologist, first presented basal body temperature method to couples in an intelligible manner to regulate births. |
| 1959 | John Marshall | John Marshall introduced Holt's approach into the UK |
| 1968 | John Marshall | First prospective field trial of the basal body temperature method, published in the Lancet |
| 1968 | John & Evelyn Billings | Developed knowledge about the role of cervical secretions into natural family planning methodology—The Billings Ovulation Method |
| 1968 | Dr John Marshall | Questionnaire survey of psychological experiences of couples in the BBT field trial published in Fertility and Sterility |
| 1977 | Edward F Keefe | Developed methodology related to self-palpation of the cervix |
| 1981 | WHO | First prospective trials of the Ovulation Method (cervical secretions only) |
| 1981 | Rice et al. US ‘Fairfield Trial’ | The effectiveness of combining the indicators of fertility was increasingly recognised through prospective studies |
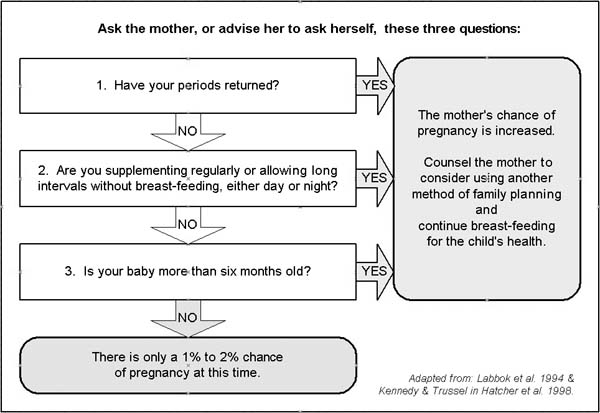
| 1988 | Bellagio, Italy | Lactational amenorrhoea method—consensus statement in the Lancet |
| 1995 | Wilcox, US | Hormonal assays and ultrasound determine the fertile time lasts from 5 days before to the estimated day of ovulation |
| 1999 | Unipath UK ‘Persona’ | A hand-held computerized device measures changes in urinary estrone-3-glucoronide (E-3-G) and LH by means of a simple urine dipstick |
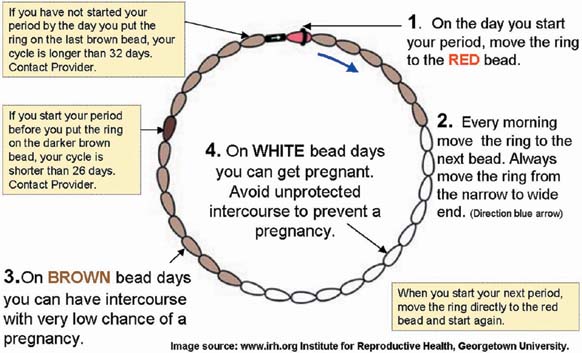
| 1999 | Arevalo, US | Introduction of the Standard Days Method (fixed formula: 8–19) rule |
| 2001 | Jennings, V | The TwoDay Method based on the presence or absence of cervical secretions |
(Adapted from; Green S, The curious history of contraception, Ebury Press, London 1971. Mucharski J, History of the Biologic Control of Human Fertility, Oakridge, New Jersey USA 1982; Belfield T, BBC Radio 4 – From Crocodile Dung to Electrocution, BBC Radio 4, Jan 2001 and data on file including published papers.)
Physiology: Defining the Fertile Time
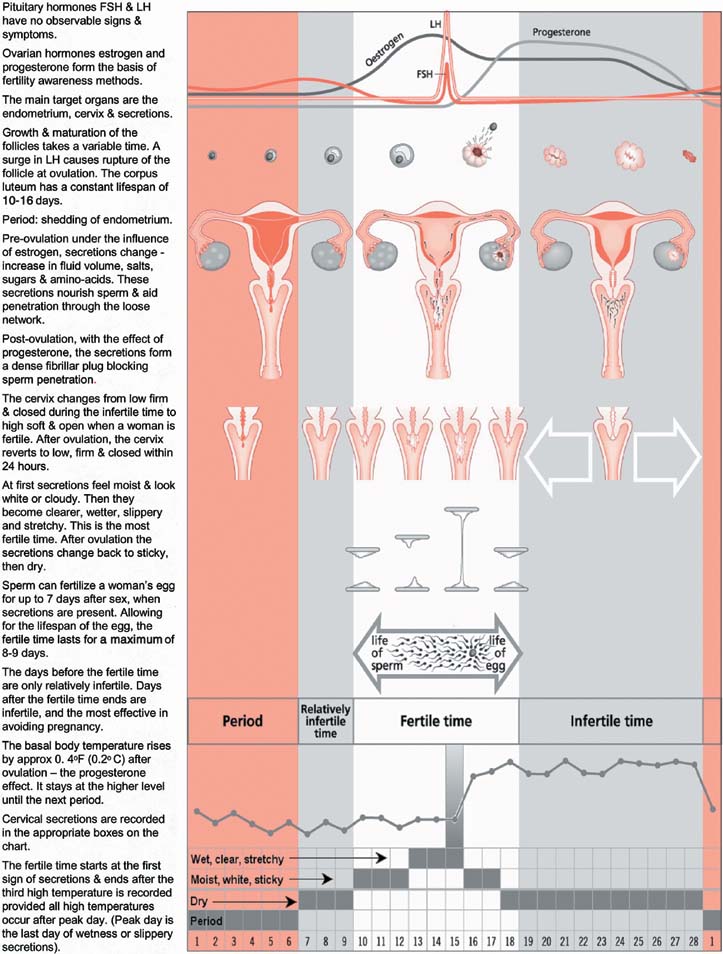
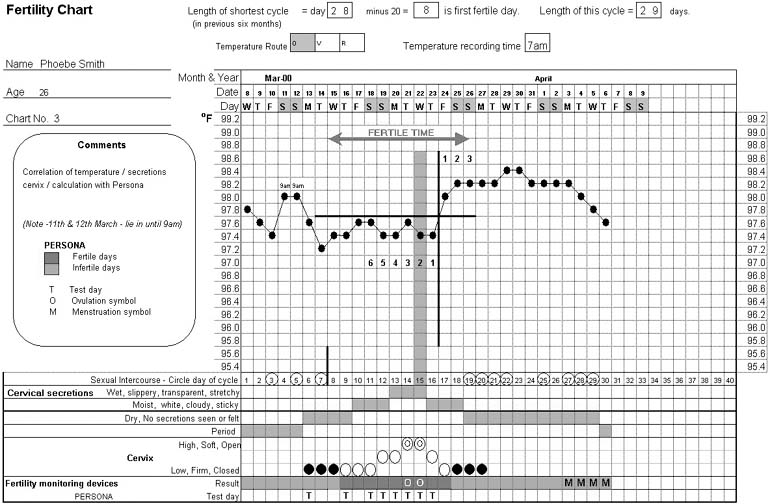
FAMs are based on an understanding of reproductive physiology. Figure 1 summarizes the physiological changes that occur during the menstrual cycle and the observed indicators of fertility.
The hypothalamus secretes pulses of gonadotrophin-releasing hormone (GnRH) to regulate the pituitary output of follicle stimulating hormone (FSH) and LH. FSH and LH act on the ovaries to stimulate the production of the ovarian hormones, estrogen, and progesterone. In the first half of the cycle (the follicular phase), FSH controls follicular growth, the growing follicles secrete estrogen, and a surge of LH triggers ovulation. The ruptured follicle develops into the corpus luteum and secretes progesterone. Estrogen and progesterone in turn affect the target organs—the endometrium (lining of the uterus), the cervix and cervical secretions and the breasts. Progesterone also has a thermogenic effect causing an increase in basal body temperature. If the egg is not fertilized, estrogen and progesterone levels decrease and the endometrium is shed at the next menstruation. In addition to its role in controlling the menstrual cycle, the hypothalamus also controls body temperature, sleep, thirst, appetite, and fluid balance. Disturbances to these bodily processes can affect the hypothalamic function and hence cause menstrual disturbances.
Baerwald evaluated changes in the ovarian follicle dynamics during the menstrual cycle.17 She found that women ovulate only once per cycle. However, women experience multiple waves of follicular development each cycle, but only one of these waves results in an actual ovulation. In 100% of the women they studied, a wave of follicular development occurred in the first half of the menstrual cycle and culminated in ovulation around the middle of the cycle. This was followed by additional follicular waves that never resulted in an ovulation.
The fertile time (days of potential fertility) is defined by the WHO as the time from the first act of intercourse, which may lead to pregnancy, to the demise of the ovum.18 The fertile time lasts for an average of 6 days. To identify the fertile time during each menstrual cycle, it is essential to know the lifespan of the sperm in the female genital tract before ovulation, the timing of ovulation, and the length of time during which the ovum can be fertilized after ovulation.
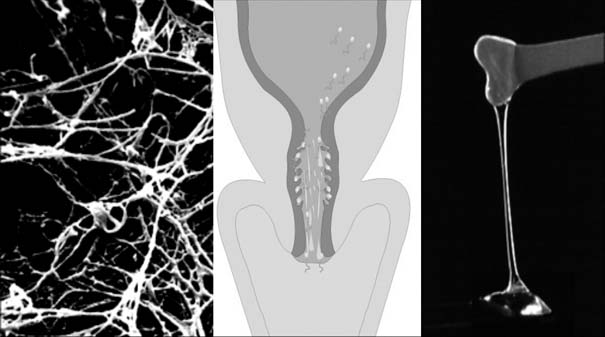
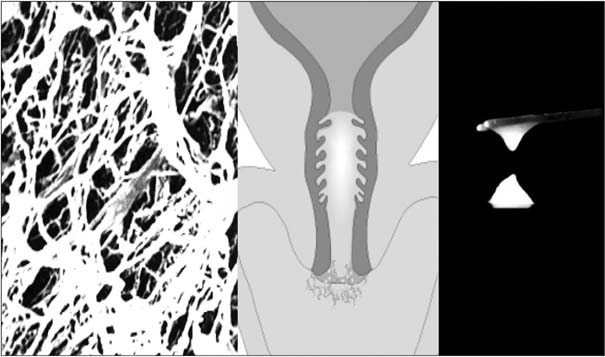
The lifespan of the sperm is up to 7 days. In the female genital tract, the survival of the sperm depends on the presence of alkaline cervical secretions (mucus), produced from the secreting cells lining the cervix. In the absence of cervical secretions, the acidic vaginal environment will rapidly destroy sperm.19,20 In the presence of fertile secretions, sperm will live an average of 3 days, with a 99% probability that the survival time is less than 7 days.21 The average life span of the ovum is approximately 17 hours.22 Fertilization must take place during those few hours after ovulation if pregnancy is to occur.
Detection of Ovulation and Correlation With the Indicators of Fertility
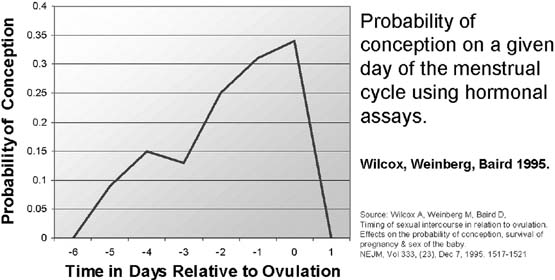
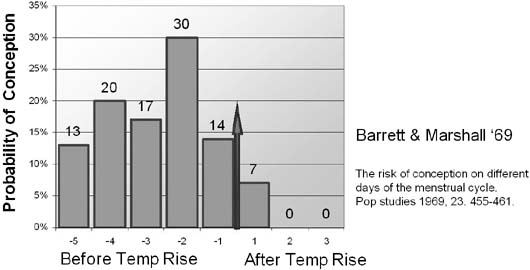
Ultrasound gives the most accurate information on the time of ovulation. Ultrasound studies have shown that the temperature increase and cervical secretion changes are accurate in indicating the time of ovulation.23 Ovulation can also be detected by hormone assays in plasma or urine.24 In the North Carolina Early Pregnancy Study, Wilcox researched the chances of conception on each day of the menstrual cycle.25 The estimated day of ovulation was determined by ratios of urinary metabolites of estrogen and progesterone. They identified the limits of the fertile window from 6 days before to 1 day after ovulation (Fig. 2).
|
|
Dunson26 compared the North Carolina data with the Barrett and Marshall data27 that used the basal body temperature (BBT) increase as a marker of ovulation. They used a new statistical model to correct for errors in estimating the day of ovulation. They suggested that BBT-based estimates of the day of ovulation are not perfect but have a high probability of being ± 1 day of the true ovulation day. They estimated the same 6-day fertile window in both studies after controlling for error.
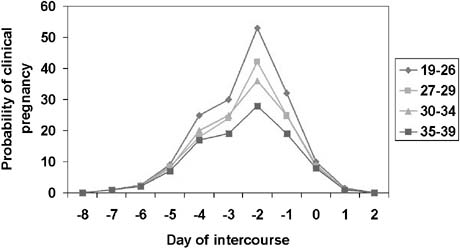
The probability of conception on a given day of the cycle was also analyzed using data from a large prospective European study of 782 women aged 18 to 40 who kept daily records of waking temperature, cervical secretions, menstruation, and intercourse. Nearly all pregnancies occurred within a 6-day fertile window. This analysis included a review of the effects of age on conception rate. There was no evidence for a shorter fertile window in older men or women. The team concluded that women's fertility begins to decrease in the late 20s, with substantial decreases by the late 30s. Fertility for men is less affected by age but shows significant decline by the late 30s28 (Fig. 3).
Further research on the probability of conception on each day of the cycle is required to more clearly define the outer limits of the fertile time. This will require larger studies that use more precise markers of ovulation and more detailed data on intercourse frequency.
Cycle Length Variability
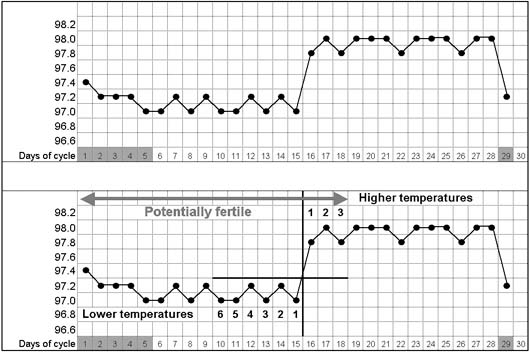
The length of a menstrual cycle is measured from the first day of menstruation, (the first day of fresh red bleeding) up to, but not including, the first day of the next menstruation. The position of the fertile time will vary according to the length of the cycle. The time from ovulation to the next menstruation is likely to be constant (approximately 10 to 16 days), whereas the time before ovulation is more variable (Fig. 4).
|
|
It is important that women understand that there is a wide variation in normal cycle length that is compatible with good health so that they do not become overly concerned by the 28-day ideal.29 In 1977 Vollman,30 evaluated the variability in cycle length. The 28-day cycle was the commonest length cycle recorded but only in 12.4% of cycles. Cycle length is most variable in the first few years after the menarche and in the years preceding the menopause. A woman's age minus her age at menarche (her gynecological age) is also an important factor when considering cycle length and regularity. Cycle length changes with age, forming a U-shape curve from the menarche to menopause. The mean cycle length decreases from 35 days at age 12 to a minimum of 27 days at age 43, increasing to 52 days at age 55 years, with an enormous range of cycle length.
A large Danish study (n = 3743) investigated the epidemiology of menstrual patterns among women of fertile age (15 to 44) and confirmed the normally used definitions of polymenorrhea (cycle length less than 21 days) and oligomenorrhea (cycle length between 36 and 90 days). The high frequency in a normal population of large menstrual cycle length variation challenges the view that an intraindividual variation of more than 5 days should be regarded as a sign of disease in women.31
Methods Used to Identify the Fertile Time
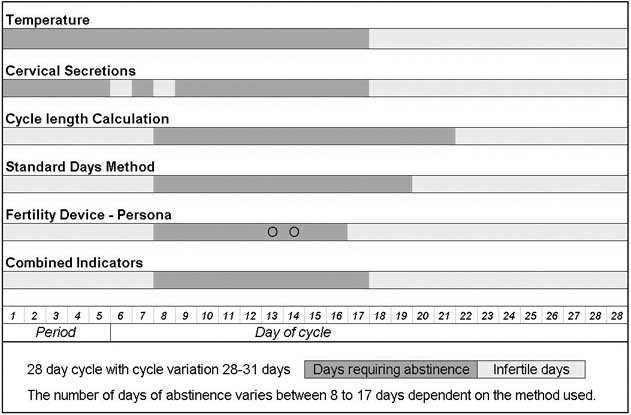
The fertile time can be identified by using three different approaches—observing physiological indicators; using a calculation based on cycle length, or by using fertility monitoring devices. The first approach—observing the physiological indicators of fertility (the observed indicators)—may include recording the basal body temperature (BBT); monitoring cervical secretions either by observing the changing characteristics or by the more simplified TwoDay Method and possibly by recording the changes in the cervix. The second way to identify the fertile time is by using calculations based on cycle length—either personalised information based on a woman's previous cycle lengths or a more simplified Standard Days Method. Finally the fertile time can be identified by using fertility monitoring devices such as personal hormone monitoring systems, and saliva testing devices. The methodology, effectiveness and evidence-base of these approaches will be discussed. The knowledge gained about the fertile time through these methods can then be used to either plan or avoid a pregnancy.
The Observed Indicators
Women are taught to observe, record, and interpret the changes in one or more of the following indicators of fertility to identify the fertile time: the BBT, the cervical secretions, and the cervix. Each of these indicators of fertility will change in response to the increasing and decreasing levels of estrogen and progesterone during the menstrual cycle. These indicators may be used alone to identify the fertile time but are more commonly combined to improve the effectiveness to avoid a pregnancy.