Reversal of tubal sterilization can be performed by reanastomosis of the two obstructed segments. Tubal reanastomosis is classified according to the anatomic location of tubal damage and surgical site: cornual-isthmic, isthmic-isthmic, isthmic-ampullary, ampullary-ampullary, and ampullary-infundibular.
Gynecologists who are interested in performing reversals of tubal sterilization must emphasize microsurgical principles. This approach involves adopting a philosophy of minimizing tissue trauma during surgery and keeping current regarding knowledge of new instruments, materials, and techniques. The gynecologist also must be able to provide adequate exposure of the pelvis, magnification of tissue, and irrigation of tissue; perform appropriate hemostasis; use microsurgical instruments and fine nonreactive sutures; and avoid permanent stents or other foreign bodies.
Exposure of Surgical Fields
A Pfannenstiel skin incision is recommended for this type of surgery unless a previous midline incision has been performed. The size of the incision is determined during the survey laparoscopy and depends on the mobility of the uterus and adnexa as well as the weight of the patient. In most patients, it is possible to elevate the adnexa or even exteriorize the uterus and tubes, as suggested by Silva and associates,19 through a small (5- to 6-cm) mini-laparotomy incision. In most instances a retractor is not needed, because the uterus and moist packs around it separate the skin surfaces.
Magnification
We prefer to use a microscope for reversal of tubal sterilization, with magnification varying between 4× and 10×. Loupes can be used, but any head motion causes defocusing and makes the procedure much more cumbersome. Most microsurgeons agree that the use of the microscope in these procedures yields higher pregnancy rates than the use of surgical loupes.20,21,22
Irrigation
Constant irrigation keeps the tissue moist, thus avoiding dryness and potential trauma with future adhesion formation; it also aids in the identification of small bleeders for cauterization. We use heparinized lactated Ringer's solution in 30-ml syringes with a 25-gauge needle catheter. This method allows for a pinpoint directed flow of solution, which aids in identifying bleeding areas.
Hemostasis
The use of a bipolar coagulator is essential to minimize tissue trauma and avoid the use of numerous sutures. The use of microforceps with bipolar coagulation capabilities is recommended. Unipolar microelectrodes also are helpful for hemostasis, and they can be used for any necessary excision of tissue, such as adhesions.
Microsurgical Instruments
In addition to bipolar forceps, other key instruments include tissue microforceps with and without teeth, a microneedle electrode, iris scissors, and fine microsurgical scissors. The use of glass, quartz, or plastic rods is helpful for tissue retraction when adhesions are present. Quartz rods are recommended as backstops for adhesiolysis when a CO2 laser is used, because they are not as fragile as glass.
Suture Materials and Needles
The use of absorbable 8-0 and 9-0 polyglactin (Vicryl) or polydioxanone (PDS) sutures are recommended because they provoke less tissue reaction and possible fibrosis than do nylon or catgut. The needle most often used is a taper-cut, 3/8 -inch circle with an overall length of 3 to 5 mm.
Technique of Reanastomosis
A pediatric Foley catheter is placed in the uterine cavity before a Pfannenstiel incision is made. This catheter is connected to intravenous tubing and a 20-ml syringe containing diluted indigo carmine dye. This equipment greatly facilitates the surgery because chromopertubation can be performed by the surgeon as needed during the procedure. This procedure allows the surgeon to assess tubal segment patency before reanastomosis, leakage of the reanastomosis site, and final tubal patency.
With the patient in the dorsal supine position, a Pfannenstiel incision large enough to allow adequate exposure of the uterus and tubes is made. A retractor is placed, and the bowel is packed with several moist laparotomy sponges. Care must be taken not to include distal tubal segments during the initial bowel packing. The uterus and adnexa are elevated by placing moistened laparotomy sponges in the cul-de-sac and fixed by placing another sponge anteriorly in the vesicouterine pouch. Sponges may be placed within a washed surgical glove to avoid drying during long surgical procedures. The goal is to elevate the adnexal structures so that the fallopian tubes have adequate exposure with minimal mobility and are as close to the plane of the abdominal surface as possible.
ISTHMIC-ISTHMIC REANASTOMOSIS.
The first step in tubal reanastomosis is preparation of the two segments of fallopian tubes. After the area of occlusion, whether a ring, clip, or cauterized area, is excised with straight, fine, iris-type scissors, both ends of the adjoining tube are cut transversely to allow patency. This procedure usually involves removal of approximately 0.5 cm from the obstructed ends of the tube, or as much tubal tissue as necessary until adequate patency is observed. Hemostasis is achieved with a bipolar coagulator or microelectrode or, if necessary, a 6-0 Vicryl suture for the mesosalpinx. Patency of the proximal end of the tube is evaluated using the previously placed intrauterine pediatric catheter. Similarly, the adjoining distal segment of the tube is prepared, and patency is checked. The use of a lacrimal probe that is fed gently through the fimbrial end or, alternatively, an 18-gauge angiocatheter, can help to delineate the area of occlusion for more accurate excision of tissue. It also can be used for distal irrigation to confirm patency. If patency of both segments is not adequate, or if the tissue does not appear viable (e.g., it is white or fibrotic), it may be necessary to excise another 0.5- to 1-cm segment of tube until this tissue appears pink and bleeds easily, and the surgeon is comfortable with the quality of the tissue and the patency. Irrigation can help to identify small bleeders, which are then controlled using cautery. A 2-0 nylon splint is then fed into the proximal and distal segments of the fallopian tube.
Before the actual reanastomosis is performed, the mesosalpingeal defect is approximated with sutures of 6-0 material such as Vicryl or PDS and placed correctly to align both lumens. Two stay sutures are placed at the junction between the mesosalpinx and the 6-o'clock portion of the tubes that are about to be approximated. The sutures are held with a small hemostat and tied after the first muscular suture at the 6-o'clock position is placed. The purpose of these stay sutures is to decrease tension on the reanastomotic site. Additional sutures incorporating only the muscular layer follow at the 3-, 9-, and 12-o'clock positions. PDS or Vicryl material is used (Fig. 1). The use of a microscope facilitates accurate placement of the sutures. The serosal layer is approximated in a circumferential manner, using as many interrupted 8-0 or 9-0 sutures as needed (see Fig. 1). In the past, the splint was removed through the cervix several days after the procedure. The need for this procedure can be avoided by gently removing the splint with atraumatic forceps before placing the 12-o'clock suture. The same procedure is repeated on the opposite tube.
|
ISTHMIC-AMPULLARY REANASTOMOSIS.
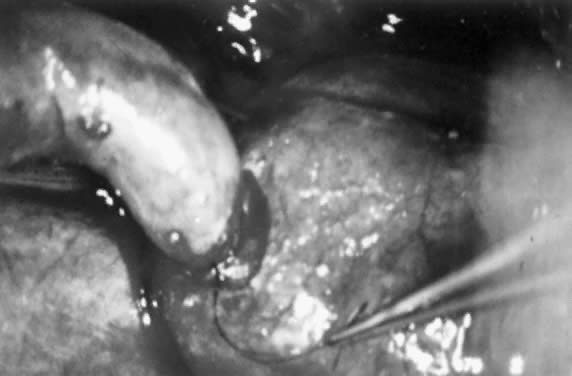
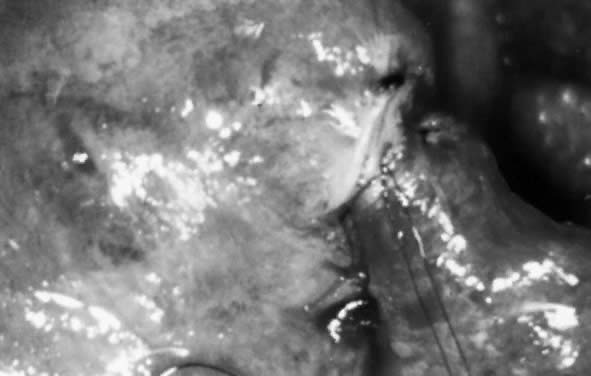
Because the ampulla is greater in diameter than the isthmus, it is important to prepare the lumens carefully to avoid significant luminal disparity. This preparation can be done in two ways. One option is to enlarge the isthmic diameter by cutting a slit anteriorly, on the antimesenteric side, to create a fish-mouth opening. Alternatively, the ampullary stump can be cut so that the diameter approximates that of the isthmic side (Figs. 2 and 3). This procedure is done by stretching the stump end with a lacrimal probe and taking small-diameter cuts until patency is reached (Figs. 4 and 5). A two-layer reanastomosis is performed in a similar fashion to that at the isthmic-isthmic site (Fig. 6).
|
|
|
|
AMPULLARY-AMPULLARY REANASTOMOSIS.
The primary difficulty with ampullary-ampullary reanastomosis is that the muscularis is thin, and the mucosal folds tend to prolapse. It may be necessary to push the mucosal folds gently inward instead of resecting them. A two-layer reanastomosis is then performed. Because the diameter is large compared with that of the much smaller isthmus, it often is necessary to place more sutures than usual to approximate the lumens.
CORNUAL-ISTHMIC REANASTOMOSIS.
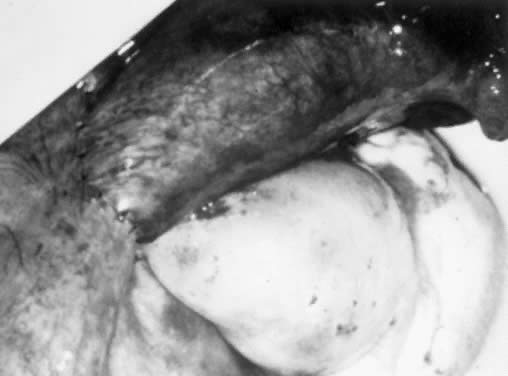
The surgical treatment of cornual occlusion by uterotubal implantation has been replaced by cornual-isthmic reanastomosis because of its superior postreversal pregnancy rates of 46% to 69%.23,24,25,26,27,28 The technique involves preparation of the isthmic portion of the tube similar to that with isthmic-isthmic reanastomosis, with some modification of the cornual side. With a small blade, such as a no. 15 Bard-Parker scalpel, the cornual region is shaved serially. One-millimeter slices are removed until patency is shown (Figs. 7 and 8). Bleeding areas are controlled, preferably by microbipolar cautery, to minimize tissue injury. After the stay sutures of 6-0 Vicryl are placed to align the lumens, a two-layer reanastomosis is performed (Fig. 9). A splint is used, but it is removed at the end of the procedure. A cornual-ampullary reanastomosis is more difficult than a cornual-isthmic procedure because of the large discrepancy in lumen diameter of the ampulla. The best recommendation is to make the ampullary diameter as small as possible, as recommended for the isthmic-ampullary reanastomosis.
|
|