Benign Neoplasms of the Vulva
Authors
INTRODUCTION
Vulvar assessment is an integral part of gynecologic examination. Vulvar abnormalities have many variations in presentation. Because multiple diagnoses may have similar gross characteristics, histologic evaluation is critical in establishing an accurate diagnosis. Histologic classification based on the tissue of origin is practical in the description of vulvar lesions. The two major categories for vulvar lesions are tumors of epithelial origin and tumors of mesenchymal origin.
TUMORS OF EPITHELIAL ORIGIN
Condyloma Acuminatum
Human papillomavirus (HPV) infections of the vulva are common clinical occurrences. HPV infections are classified as either clinical or subclinical, contingent on the infectivity of the virus and the response of the affected epithelium. The typical expression is a soft, pink-white, papillary epithelial lesion. These lesions may occur singly or in clusters that may become confluent (Fig. 1). The usual vulvar locations are the prepuce, vestibule, and perineal body. Perianal and anal loci also are seen frequently.
Although there are more than 60 subtypes of HPV, relatively few affect the vulva.1 The HPV subtypes that are most frequently encountered on the vulva are HPV 6 and HPV 11. HPV 2, the virus associated with common epithelial warts, also is seen in the squamous epithelium of the vulva.2 HPV subtypes that are associated with a higher incidence of malignant transformation on the cervix, specifically HPV 16, 18, 31, and 35, may be present in vulvar lesions.1 The incidence of the diagnosis of vulvar, vaginal, and cervical HPV lesions has increased significantly in the last three decades.3 This increase is partly attributable to advancements in diagnostic techniques, such as polymerase chain reaction and DNA hybridization techniques. Although it is difficult to estimate the incidence or prevalence of the infection, estimated percentages of patients with clinical and subclinical HPV infection in some college populations exceed 40%.1 There is no reliable method of identifying subclinical or dormant infection. Even if only clinically expressed HPV is considered, it is now one of the most common sexually transmitted diseases. Some HPV infections may progress to vulvar intraepithelial neoplasia (VIN) and an even smaller segment may progress further to frankly invasive squamous cell carcinoma of the vulva, but the majority of lesions are limited to the HPV cutaneus expression known as the venereal wart or condyloma. Immunosuppressed states and pregnancy are associated with enlargement and progression of condylomatous lesions (Fig. 2).3
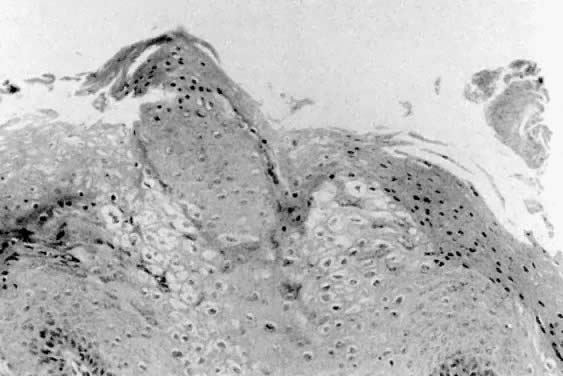
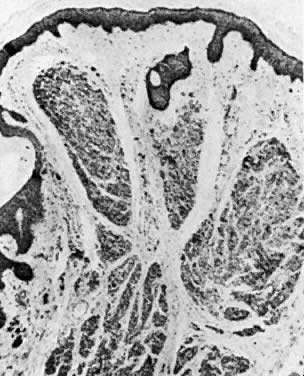
Histologically, condylomata appear as epithelial papillomas with acanthosis and parakeratosis (Fig. 3). Some epithelial cells exhibit atypical nuclei and perinuclear halos that are believed to be a manifestation of HPV infection.2 These cells are known as koilocytes. The underlying stroma usually exhibits a mild inflammatory response. Biopsies of condylomatous lesions that are resistant to treatment or that have an abnormal appearance should be performed for histologic confirmation of the diagnosis. Differentiation between condylomata and vulvar papillomatosis or other vulvar lesions can then be made.
Treatment consists of destruction of the cutaneous manifestations of the HPV infection. Eradication of the virus from the epithelium is not clinically possible. Control of epithelial viral expression can be accomplished with topical agents such as trichloroacetic acid, bichloracetic acid, podophyllin or its derivatives, or topical 5-fluorouracil (5-FU). Cryotherapy, laser vaporization, and electroexcision or desiccation are other methods of treatment. Intralesional or systemic administration of interferon is another therapeutic option that usually is reserved for recalcitrant lesions. Recurrent viral cutaneous expressions usually are managed with alternative treatments or combinations of treatments.
Verrucous carcinoma of the vulva appears as a large condyloma or a lesion suspicious for invasive carcinoma. The lesion, first described by Buschke and Lowenstein as a giant condyloma,2 is associated with the HPV 6 viral subtype.1 Verrucous carcinoma may involve large areas of the vulva, and it has a pushing rather than an infiltrative border. Characteristically, it is localized to the vulva. Management is best accomplished by wide excision and careful postoperative evaluation.
Vulvar Intraepithelial Neoplasia
Vulvar intraepithelial neoplasia is a hyperplastic squamous lesion with atypia that is confined to the epithelium. VIN is histologically divided into three categories: VIN I (mild dysplasia), VIN II (moderate dysplasia), and VIN III (severe dysplasia and carcinoma in situ). VIN lesions are sufficiently atypical to be considered premalignant. The incidence of progression to a malignant invasive process is relatively low (10% to 15%), and the time frame for progression may span several years.4
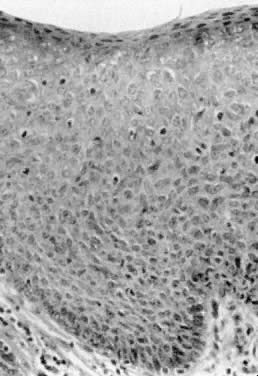
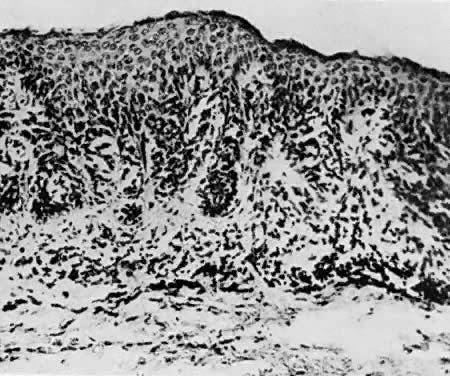
Bowen's disease, VIN III, and carcinoma in situ are clinically synonymous terms. These lesions appear as hyperkeratotic, raised, and frequently pigmented epithelial thickenings (Fig. 4). They usually occur in women who are in the sixth decade or older; however, a younger age does not exclude the diagnosis. Biopsy findings show full-thickness epithelial atypia and mitotic activity (Fig. 5). The affected areas may be asymptomatic or excoriated from scratching. Any thickened, raised, or hyperkeratotic lesion observed during gynecologic examination should be considered for biopsy, regardless of the associated symptoms. Vulvar lesions may be multifocal; therefore, multiple biopsies are suggested. Enhancement of lesions with dyes such as toluidine blue has been recommended to address the multifocal nature of these lesions. Toluidine blue should stain the areas of nuclear concentration that are associated with VIN III; however, most lesions are hyperkeratotic, and the keratin surface prevents penetration of the dye to the epithelial nuclei. A more effective approach is application of a dilute acetic acid solution to the vulva. Areas of VIN and HPV expression become acetowhite after soaking for several minutes.4 The vulva then can be examined with a magnifying lens or colposcope. In this manner, subtle epithelial changes are more easily identified.
Bowen's disease or VIN III should be treated with surgical, laser, or electrical excision.4 It is preferable to remove the lesion with a technique that provides tissue for further histologic study. The use of 5-FU or systemic interferon has had marginal compliance and success.3,5 Surgical excision with assessment of margins remains the preferred management option. Close follow-up to assess recurrence is suggested.
Bowenoid papillosis has a clinical and pathologic presentation that is similar to that of VIN III. It occurs in patients in the second, third, and fourth decades of life. It is expressed as multiple papillomatous lesions that may involve more than one area of the vulva.3,4 These lesions are associated with HPV infections. Biopsy findings show epithelial atypia with koilocytotic changes of HPV. Progression to an invasive malignancy occurs in rare cases, such as in immunosuppressed or immunocompromised patients. Management is conservative unless premalignant changes are present. Premalignant lesions are treated in a manner similar to VIN.
Basal Cell Carcinoma
Basal cell carcinomas usually are asymptomatic until they are large enough to be noticed by the patient or until ulceration and bleeding develop. The tumor is firm with rolled borders, and most often is found on the labia majora of postmenopausal women. Metastasis is rare. Management consists of wide excision of the tumor with adequate margins. Evaluation for metastases should be considered if the excised specimen shows invasion of subcutaneous fat, tumor thickness greater than 1 cm, or involvement of the urethra or vagina. Basal cell carcinomas account for 2% to 4% of benign neoplasms of the vulva.6
Histologically, these tumors have peripheral palisading of the basal cells at the epithelial margins. The remainder of the tumor has closely packed, uniform cells, with basophilic nuclei and scant cytoplasm. Mitotic figures are frequent. These tumors are locally invasive; therefore, thorough study of the entire lesion is necessary. The margins in particular should be evaluated and reported for adequacy. Margins of less than 4 mm are at higher risk for recurrence.
Acrochordon
Fibroepithelial polyps are common in the vulvar epithelium. They are referred to as skin tags. There is no malignant potential for this lesion. They are soft, flesh-colored, polypoid structures. Skin appendages and hair are not characteristic of acrochordon. Therapy is local excision of symptomatic lesions.
Histologically, the acrochordon is described as a fibrovascular stalk with mature hyperkeratotic squamous epithelium. Epidermal appendages are infrequent, and the vascular pattern may be enhanced.
Hidradenoma
Hidradenomas are tumors of the apocrine sweat glands. Some may have an origin in the eccrine sweat glands. They usually are less than 1 cm in diameter, and they occur on the medial aspect of the labia majora (Fig. 6). The lesions are firm and freely movable. Ulceration and pain may develop if the lesion connects with the epithelial surface. Treatment is surgical excision.
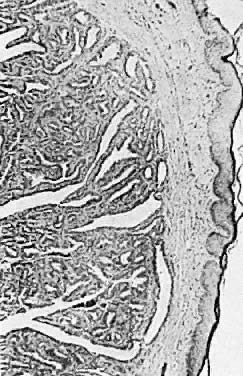
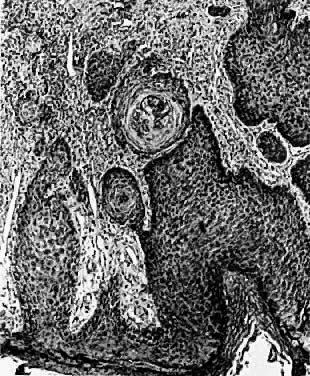
Histologically, the hidradenoma has cystic spaces that are lined with columnar cells. The lesion is further characterized by many complex folds, papillary structures, and pronounced glandular proliferation (Fig. 7). This lesion may be confused with adenocarcinoma. The distinguishing features of the hidradenoma include the lack of pleomorphism, stacking up of cells, and nuclear conformity.
Syringoma
Syringomas are small, benign hamartomas of the eccrine sweat glands. Usually, multiple lesions are present, and they may occur at more than one site on the body. The lesions are asymptomatic, and no treatment is needed unless pain or pruritus develops.7
Microscopically, these are tumors of dilated sweat gland ducts, and cysts lined with benign cuboidal cells (Fig. 8). A minimal inflammatory response is present unless the cysts rupture.
Pigmented Vulvar Tumors
Pigmented vulvar lesions occur in 10% to 12% of all women. Two percent have pigmented changes with premalignant characteristics. Benign pigmented lesions are classified as lentigines, vulvar melanosis, and nevi.
Lentigines are small (1 to 4 mm), well-circumscribed macules. They occur in 3% to 6% of women. Lentigines also are part of several syndromes that include atrial myxoma and other cardiac structural and conduction defects (LAMB syndrome, LEOPARD syndrome).8 No therapy is necessary.
Histologically, lentigines are similar to junctional nevi. There is hyperplasia in the epidermis, and increased melanin in the basal layer of skin. Nuclear atypia is not seen in the hyperplastic tissue.
Vulvar melanosis is a lesion that is larger than lentigo and has an irregular border. Histologically, increased numbers of melanocytes and dermal melanophages are present. Melanin deposition in the basal and suprabasal epidermal layers is present. Vulvar melanosis and lentigines are part of a spectrum of pigmentation changes of the vulva. It is important to distinguish them from melanomas by performing biopsy of a representative area.
Vulvar nevi occur in 2% of women. Nevi are classified as intradermal, junctional, and compound. The intradermal nevus arises within the dermis (Fig. 9), and the junctional nevus arises from the basal epidermal layer (Fig. 10). The compound nevus has characteristics of both intradermal and junctional nevi (Fig. 11). Histologic evaluation of the melanocytes for atypical architecture and cytologic changes distinguishes pigmented nevi from melanoma. Irritated or bleeding nevi should be excised. A high index of suspicion and liberal use of excision should be part of the management scheme.
TUMORS OF MESENCHYMAL ORIGIN
Leiomyoma
Leiomyomas are derived from smooth muscle components of the vulva. These include round ligament remnants, cutaneous smooth muscle tissues, erectile tissue, and blood vessels. The tumors usually are smooth and movable,9 and they most frequently occur in the labia majora. Treatment is local excision. The histologic characteristics are identical to those of other gynecologic leiomyomas.
Lipoma
Lipomas of the vulva have similar characteristics to lipomas that occur on other parts of the body. They arise in vulvar fatty tissue and rarely exceed 4 cm in diameter. Histologically, they are composed of mature fat cells with a thin capsule. Treatment is local excision.
Fibroma
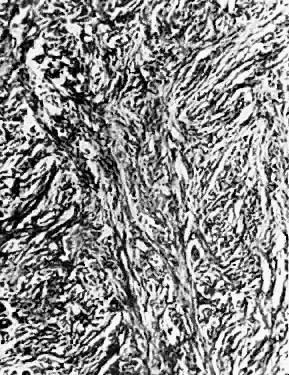
Fibromas occur on the vulva as small exophytic projections. They may become large and produce symptoms (Fig. 12). The lesions are composed of dense collagen fibers and fibroblasts, and they usually are seen on the labia majora. The histologic appearance is similar to that of leiomyomas (Fig. 13). Treatment consists of local excision.
Neurofibroma
Neurofibromas are dermal tumors that make up 5% of all benign vulvar lesions. They are small, flesh-colored, pedunculated lesions on the labia that develop after puberty. Eighteen percent of patients with von Recklinghausen's disease have vulvar neurofibromatosis as a component.10 One half of patients with vulvar neurofibroma will have von Recklinghausen's disease. Of patients with von Recklinghausen's disease, black women have vulvar neurofibromas more frequently (28%) than white women (15%) (Fig. 14).10 These lesions have eosinophilic fibrils,11 usually exclusive of neural tissue. Occasionally, they form a larger mass that is symptomatic and requires excision; otherwise, no treatment is necessary.
Granular Cell Tumor
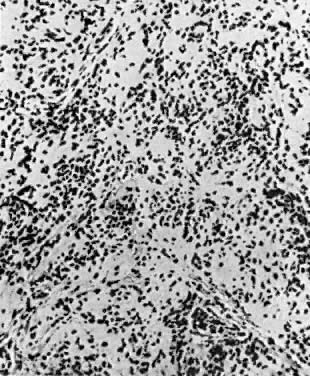
Granular cell tumors (granular cell myoblastomas) of the vulva range in size from 1 to 4 cm. These lesions characteristically form firm nodules with poor encapsulation, usually located on the labia majora. These asymptomatic, slowly growing benign neoplasms arise from neural tissue, and may occur in a deep or superficial location with respect to the epidermis. The tumor infiltrates the underlying tissue and may ulcerate if it reaches the epidermis. This pseudoepithelial hyperplasia may be clinically confused with squamous cell carcinoma of the vulva. Microscopically, the tumors are composed of large eosinophilic, polygonal cells. Cells are arranged in sheets with irregular borders; collagen fibers occur within the field of cells (Fig. 15). The tumor extends into the contiguous tissue, and may cause an epidermal response of accentuated acanthosis that resembles squamous cell carcinoma histologically.
Treatment is local excision. Wide local excision is suggested because of the infiltrative nature of the tumor. Although these tumors are benign, incomplete excision may lead to recurrence of the lesion. A malignant version of the granular cell tumor has been reported; however, its occurrence is rare.6
Vascular Tumors
Malformations of vascular and lymphatic tissue may occur on the vulva, including capillary hemangioma, cavernous hemangioma, angiokeratoma, lymphangioma, and Kaposi's sarcoma.
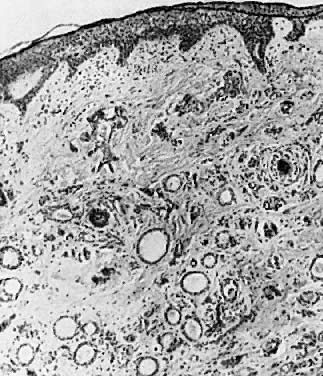
Hemangiomas, both capillary and cavernous, are well-demarcated papules. They may be congenital or acquired, and usually are asymptomatic. Cavernous hemangiomas show atypical proliferation of endothelial-lined spaces and vessels, with large, dilated vessels that extend into the subdermis and subcutaneous tissue. Hemangiomas usually are managed expectantly, unless trauma causes bleeding or other symptoms develop. Active management includes excision, laser therapy, sclerosing agents, or cryotherapy.
Angiokeratomas are dark red to brown papules with an irregular verrucoid surface. They rarely are larger than 2 cm. If the lesion becomes symptomatic, or if clinical suspicion of melanoma exists, an excisional biopsy should be performed.
Lymphangiomas are similar to hemangiomas, but they do not have red blood cells in the vessels. Absence of a muscular layer around the vascular structures further distinguishes these lesions from hemangiomas (Fig. 16). Grossly, they present as multiple, white or gray, vascular nodules with epithelial thickening.12 The lesion usually is subdermal. Treatment is surgical excision if symptoms develop.
Kaposi's sarcoma is a multifocal vascular tumor associated with acquired immunodeficiency syndrome, rarely occurring on the vulva.13 Inflammation, hemorrhage, and fibrosis are associated with a dermal proliferation of endothelial-lined vessels and spindle cells. This diagnosis should prompt further clinical study of the immune status of the patient. The patient should be tested for human immunodeficiency virus. Smaller lesions can be excised. Larger lesions are managed with local radiation therapy or systemic chemotherapy.
Endometriosis
Ectopic endometrial tissue may occur on the vulva. The usual location for endometriosis of the vulva is in healed episiotomy scars. Clinically, patients report cyclic pain and dyspareunia. Histologically, endometrial glands and stroma with extensive hemosiderin deposition are identified. Vulvar adenosis, which may occur after laser vaporization of condyloma, can mimic endometriosis.14 Excision is the best method of management. Recurrences are common.
Grandular Cysts
Tumors of the vulva may result from cystic enlargement of the vulvar glands. Cysts of both Bartholin's duct and Skene's duct may occur. The pathophysiologic features involve blockage of the gland duct, with continued secretion or infection of the gland itself. Without a route of egress, the glandular location swells and enlarges (Fig. 17). Clinically, these lesions are cystic to palpation and may be tender if infection is present. Management is incision and drainage, with or without marsupialization. Recurrent episodes may prompt excision of the gland. It is important to diagnose these tumors as cystic because solid malignant tumors of these areas may present in a similar fashion.
REFERENCES
Sawchuk WS: Vulvar manifestations of human papillomavirus infection. Dermatol Clin 10: 405, 1992 |
|
Kaufman RH, Friedrich EG, Gardner HL: Viral infections. In Benign Diseases of the Vulva and Vagina, 3rd ed, pp 111–122. Chicago, Year Book Medical Publishers, 1989 |
|
Potkul RK, Lancaster WD, Kurman RJ et al: Vulvar condylomas and squamous vestibular micropapilloma. J Reprod Med 135: 1019, 1990 |
|
Wilkinson EJ: Normal histology and nomenclature of the vulva, and malignant neoplasms, including VIN. Dermatol Clin 10: 283, 1992 |
|
Kaufman RH, Friedrich EG, Gardner HL: Intraepithelial neoplasia of the vulva and vagina. In Benign Diseases of the Vulva and Vagina, 3rd ed, pp 179–188. Chicago, Year Book Medical Publishers, 1989 |
|
Hood AF, Lumadue J: Benign vulvar tumors. Dermatol Clin 10: 371, 1992 |
|
Carter J, Elliott P: Syringoma: An unusual cause of pruritus valvae. Aust N Z J Obstet Gynaecol 30: 382, 1990 |
|
Rock B: Pigmented lesions of the vulva. Dermatol Clin 10: 361, 1992 |
|
Faber K, Jones MA, Spratt D, Tarraza HM: Vulvar leiomyomatosis in a patient with esophagogastric leiomyomatosis: Review of the syndrome. Gynecol Oncol 41: 92, 1991 |
|
Gersell DJ, Fulling KH: Localized neurofibromatosis of the female genitourinary tract. Am J Surg Pathol 13: 873, 1989 |
|
Blickstein I, Lurie S: Gynaecological problems of neurofibromatosis. Aust N Z J Obstet Gynaecol 30: 380, 1990 |
|
Johnson TL, Kennedy AW, Segal GH: Lymphangioma circumscription of the vulva: Report of two cases. J Reprod Med 36: 808, 1991 |
|
Rajah SB, Moodley J, Pudifin DJ et al: Kaposi's sarcoma associated with acquired immunodeficiency syndrome presenting as a vulval papilloma. S Afr Med J 2: 585, 1990 |
|
Sedlacek TV, Riva JM, Magen AB et al: Vagina and vulvar adenosis: an unsuspected side effect of CO2 laser vaporization. J Reprod Med 35: 995, 1990 |