Operations for Support of the Vaginal Vault
Authors
INTRODUCTION
Preventing vaginal vault prolapse by supporting the vaginal cuff is an essential part of hysterectomy, whether abdominal or vaginal. The incidence of posthysterectomy vaginal prolapse varies from 0.2% to 43%.1, 2 Preventing complications is a sine qua non in surgery. In transvaginal or transabdominal hysterectomy, it is necessary to use the pelvic supporting structures (uterosacral and cardinal ligaments) to support the vaginal cuff. Any successful repair will restore normal anatomy and a functioning vagina. In this chapter, various principles of vaginal fixation during hysterectomy are discussed, including attaching the vagina to the pelvic supporting structures, correcting, or preventing an obvious or potential enterocele, and performing a colpopexy, both vaginal and abdominal.
ANATOMY
The normal vaginal axis lies almost horizontally and superior to the levator plate.3 The vagina lies parallel to the levator ani, not directly over the genital hiatus. At the time of increased intra-abdominal pressure, the levator plate and endopelvic fascia (especially the cardinal-uterosacral complex) hold the cervix and upper vagina in their proper positions.
Stretching and laceration of the supportive structures can result in uterine or vaginal prolapse. Etiologic factors include trauma, menopausal atrophy and attenuation, and, possibly, pudendal neuropathy, with loss of levator and endopelvic fascia integrity. The uterus and vagina then overlie the genital hiatus, which leads to the prolapse of the organs.
Discussions of methods to help prevent posthysterectomy prolapse follow. These steps are performed both routinely and adjunctly. They call for strict attention to attaching the uterosacral and cardinal ligaments to the vaginal membrane. Also discussed are techniques to close the cul-de-sac of Douglas that are used to prevent the formation of an enterocele and prevent apical descent.
PREVENTING VAGINAL PROLAPSE AT THE TIME OF HYSTERECTOMY
During transvaginal hysterectomy, the uterosacral-cardinal ligament complex must be reattached to the vagina. The following steps can be performed at the beginning or the end of the procedure. I perform these steps at the beginning of a transvaginal hysterectomy so that the sutures are not cut by mistake later in the procedure, and so that these steps are not forgotten if the procedure becomes difficult or complicated. If the support is defective at the beginning of the case, I use a more proximal attachment of the uterosacral ligament to the cuff at the end of the procedure.
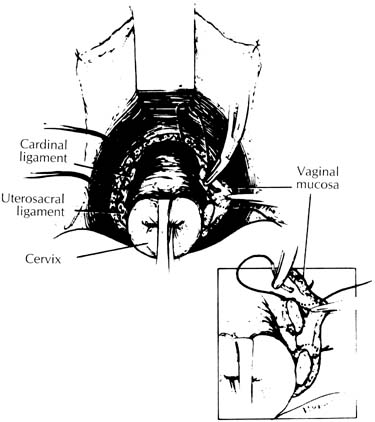
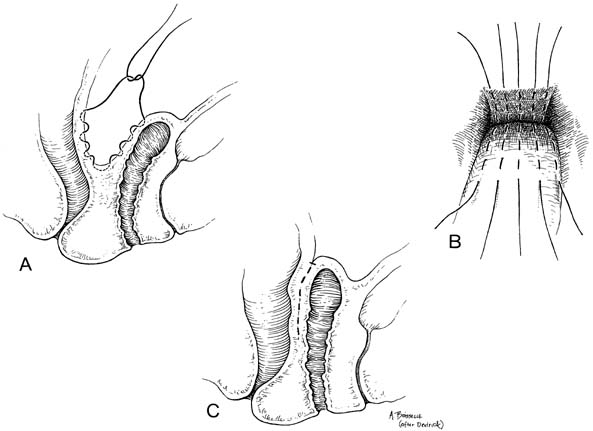
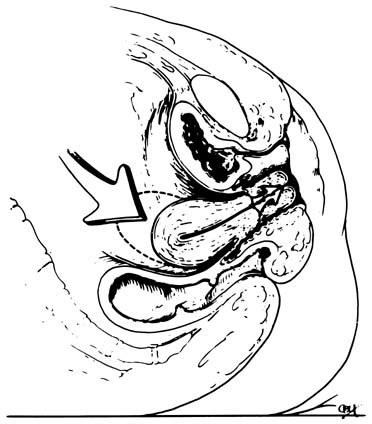
After the anterior and posterior cul-de-sacs are entered, the uterosacral and cardinal ligaments are cut and ligated. If these supporting structures are not frail or attenuated, the pedicles are sutured to the vaginal membrane (Fig. 1). By securing the pedicles to the lateral angles of the vagina, the vault is supported and the lateral angles of the vaginal cuff are readily sutured. Care must be taken because these are common sources of postoperative bleeding. These steps are completed during any transvaginal hysterectomy. If the indication for hysterectomy includes uterovaginal prolapse, these ligaments must be shortened to eliminate any laxity that is present. Shortening can be accomplished at the beginning of the procedure as long as the anterior cul-de-sac has been entered and the bladder retracted. This step elevates the bladder and ureters out of harm's way. If the uterosacral-cardinal ligaments need shortening but hysterectomy must be performed without entering the anterior cul-de-sac, the shortening steps should be performed after the uterus is removed and the bladder and ureters are elevated. A recent study showed that in all patients except those with severe uterovaginal prolapse or procidentia, the ureter actually is protected by the cutting of the cardinal ligaments at the start of the procedure.4 This step allows the ureters to fall laterally and retract toward the lateral pelvic sidewall.
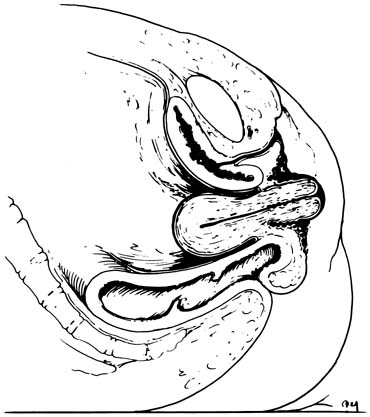
The McCall culdoplasty or a modification of this procedure is another means of supporting the vaginal cuff during transvaginal hysterectomy.5,6,7 This procedure incorporates the uterosacral and cardinal ligaments to the peritoneal surface. The sutures are attached so that when tied, the uterosacral-cardinal ligaments are drawn toward the midline, thereby helping to close off the cul-de-sac. In addition, when the suture is tied, it draws the posterior vaginal apex up to the supporting structures, elevating it to a normal position. This maneuver can be performed with one or more sutures (Fig. 2). The only drawback to this type of culdoplasty is a possible increased incidence of kinking or ligating the ureter, because it is so close to the uterosacral ligament.
Any modification of these procedures to attach the supporting structures (uterosacral cardinals) to the vagina will work. The important point is to perform these steps during the transvaginal hysterectomy. During an abdominal hysterectomy, the cardinal and uterosacral ligaments also should be attached to the vaginal cuff. As soon as the uterus and cervix are removed, the uterosacral pedicles are sewn to the lateral angles of the vagina. They may be incorporated as part of the lateral angle stitch or separately. There is no need to incorporate the round ligaments to the cuff, because they do not aid in cuff suspension and, in fact, may draw the ovaries to a position overlying the vaginal apex, predisposing the patient to dyspareunia.
Emphasis should be given to preventing posthysterectomy vault prolapse. Prolapse of the vagina results from the loss of normal pelvic support or occurs as a result of omitting the steps that use these pelvic support tissues during hysterectomy. This complication occurs after either transvaginal or transabdominal hysterectomy; hysterectomy alone will not cure uterovaginal prolapse. Hysterectomy permits the surgeon to visualize and use the supportive structures, attaching them to the vaginal membrane.
Several methods of vaginal fixation at the time of hysterectomy are currently recognized. Surgeons should attempt to prevent posthysterectomy prolapse by using the cardinal-uterosacral complex as described.
PREVENTING ENTEROCELE
Another step that helps prevent complications after transvaginal or transabdominal hysterectomy is caring for the cul-de-sac of Douglas. Whether a normal cul-de-sac, a deep cul-de-sac, or an obvious enterocele is found, an attempt should be made to avert future enterocele formation or identify and correct an obvious enterocele.
Closure of the abdominal peritoneum should be performed during vaginal hysterectomy as part of the attempt to prevent enterocele formation. Closure of the peritoneum itself is unnecessary for proper healing. However, if a deep cul-de-sac or obvious enterocele is not repaired, future enterocele formation and vaginal vault prolapse may occur.
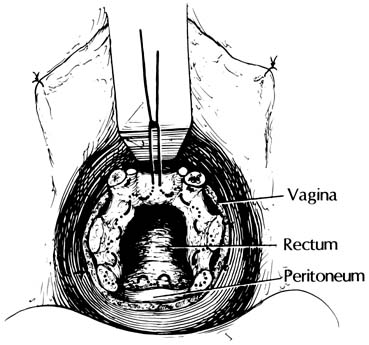
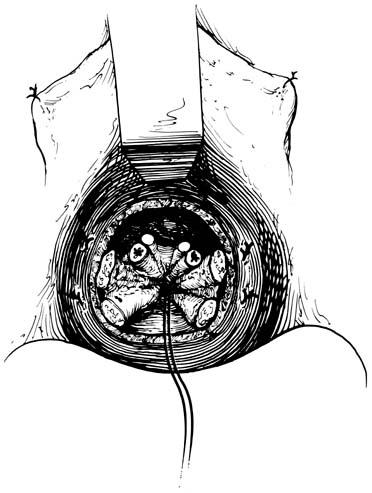
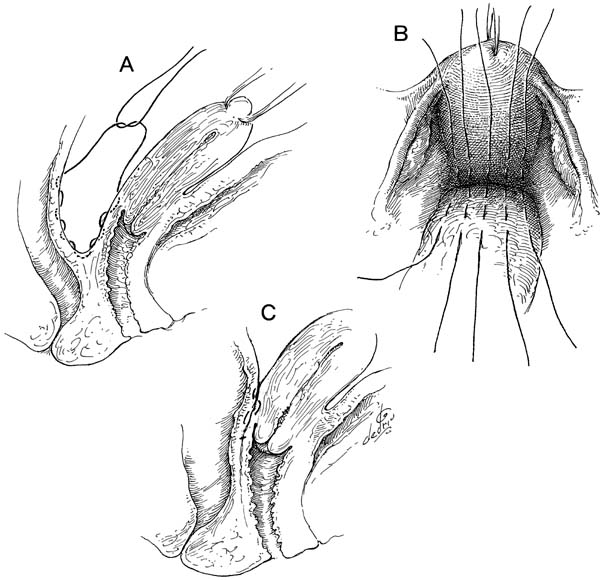
At the time of transvaginal hysterectomy, the cul-de-sac can be closed as follows. Beginning at the 12 o'clock position, a full-length, long-acting absorbable or permanent suture is placed through the anterior peritoneum (Fig. 3). In a clockwise fashion, a running purse-string suture is placed in the peritoneum. The suture may be placed counterclockwise if the surgeon is left-handed. At the level of the uterosacral and cardinal ligaments, a bite is taken through each of these ligaments proximal to the ligature connecting the pedicle to the vagina. The suture is passed through the anterior rectal serosa approximately 3–4 cm above the level of the peritoneal reflection. The suture is brought around to meet the free end of the tie. It is drawn and tied to ensure adequate and high abdominal peritoneal closure (Fig. 4). The suture is held and sewn to the vagina at the level of the cardinal ligaments as the vaginal cuff is closed. Compared with simple peritoneal closure and a McCall-type closure, this procedure only closes the cul-de-sac; it does not effectively prevent an enterocele.7
|
Several methods have been described to care for the posterior cul-de-sac of Douglas in both transvaginal and transabdominal hysterectomy.5, 6, 7, 8, 9, 10, 11 These methods vary slightly in technique, but the goals remains the same: to prevent or repair an enterocele. However, only a McCall-type suture has been shown to truly prevent enterocele formation.7
The Halban cul-de-sac closure11 is a vertical closure of the peritoneum that was first described for abdominal procedures (Figs. 5 and 6). By incorporating these peritoneal sutures vertically, ureteral damage is averted while the surgeon closes off a potential, deep, or obvious enterocele sac. This procedure is effective for transvaginal surgery as well (Fig. 7). It closes the cul-de-sac without requiring placement of sutures near the ureters. It also accomplishes high peritoneal ligation, which is an important step in closing a deep cul-de-sac. If the intact uterosacral ligaments can be picked up in the Halban-type suture, this will add strength to the closure.
|
The Moschcowitz procedure was first described as a method to close off a deep cul-de-sac in conjunction with prolapse of the rectum. It has been modified and is now heralded as a technique to close the cul-de-sac during the course of different abdominal procedures (i.e., hysterectomy, abdominal sacrocolpopexy, abdominal procedures for genuine stress incontinence). A circumferential suture (Fig. 8) is used to close the cul-de-sac. The anterior portion of the ligature is attached to the posterior side of the lower uterine segment if the uterus is left in situ or to the posterior vaginal wall peritoneum after hysterectomy. The method of cul-de-sac closure described previously for transvaginal hysterectomy is a modification of the abdominal Moschcowitz suture. Whether performed abdominally or vaginally, care must be taken to avoid the ureter because it is so close to the uterosacral ligaments. However, avoiding the ureters does not preclude grasping the uterosacral ligaments as an integral part of this repair. The surgeon can avoid this area with the use of direct palpation and identification12 of these structures during placement of the cul-de-sac–plicating ligatures. Of all the aforementioned procedures, only the McCall-type stitch is effective in preventing and curing an enterocele.
Enterocele formation is more common than often recognized. Ranny8 reported an incidence of 18.1% in patients undergoing major gynecologic operations. Failure to close a deep cul-de-sac at the time of hysterectomy or other procedure can result in hernia formation. Whether repairing or preventing an obvious or potential enterocele, the objectives are the same: to restore function and anatomy, prevent recurrence, and use an appropriate procedure.
Transvaginal hysterectomy and transperitoneal abdominal procedures allow the surgeon to evaluate the cul-de-sac and prevent the formation of an enterocele.
ADJUNCT SUPPORT TO THE VAGINAL CUFF
Most transvaginal hysterectomies have some degree of uterovaginal descensus. In some cases, the primary indication for hysterectomy is symptomatic pelvic relaxation. In patients who have stage I to stage IV uterovaginal prolapse, adjunct vaginal apex support may be necessary. Stage I uterovaginal prolapse is defined as the presentation of the cervix past the mid portion of the vagina, stage II to the hymen as a result of Valsalva's maneuver. Stages III and IV uterovaginal prolapse are defined as the presentation of the cervix at least 1 cm past the hymen with Valsalva's maneuver (Figs. 9 and 10).13, 14 Patients with these degrees of relaxation before surgery may be candidates for more than uterosacral-cardinal ligament complex attachment to the vaginal membrane. Moreover, in some patients, preoperative presentation will differ; however, after vault support and plastic vaginal repair procedures have been performed, the vaginal vault still may be pulled to or past the hymen. This condition, although diagnosed intraoperatively, must be repaired. Both preoperative and intraoperative evaluation of pelvic support must be performed to repair all the defects that are present.
|
|
Traditionally, sacrospinous fixation of the vagina and abdominal sacrocolpopexy have been considered appropriate only for the repair of vaginal vault prolapse or certain types of enteroceles.15, 16 However, these procedures also may be used as an adjunct procedure to prevent posthysterectomy vault prolapse. Not every patient who undergoes hysterectomy is a candidate for these procedures. If loss of the pelvic supportive structures (uterosacral-cardinal ligament complex) is noted at hysterectomy, an attempt to use their remnants should be made. However, the use of sacrospinous fixation as an adjunct procedure will prevent further vault prolapse. If abdominal hysterectomy is indicated in a patient with uterovaginal prolapse, abdominal sacrocolpopexy can be performed as an adjunct procedure.
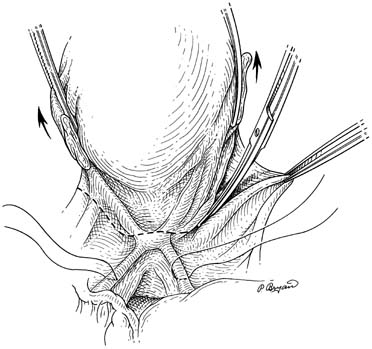
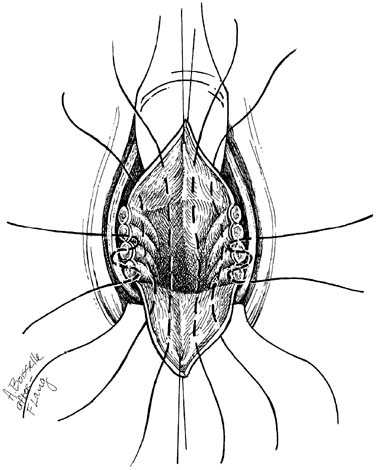
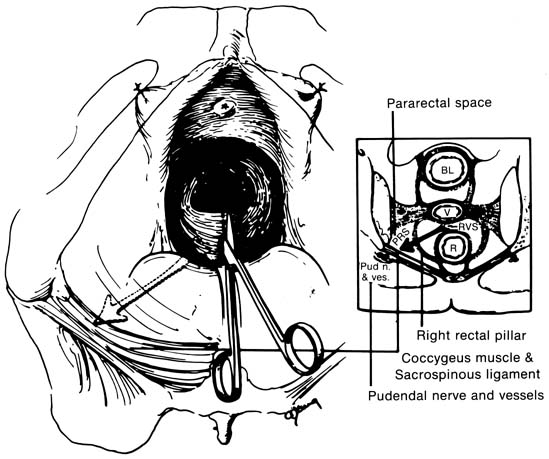
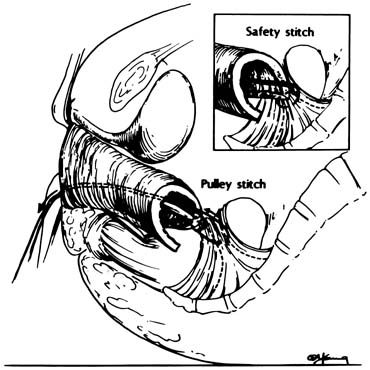
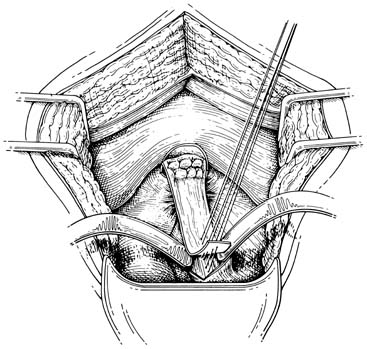
If preoperative or intraoperative evaluation in a patient undergoing transvaginal hysterectomy shows the need for adjunct vaginal support, a sacrospinous colpopexy is easy to perform after hysterectomy. The sacrospinous ligament fixation procedure is performed as follows. The posterior vaginal wall is opened to the apex, and the rectovaginal space is entered. This space is dissected with the surgeon's finger to the level of the ischial spine. The descending rectal septum (pillar) is perforated, opening the pararectal space (Fig. 11). With additional blunt dissection, the ischial spine and coccygeus muscle–sacrospinous ligament complex are palpated and identified visually. Long-acting absorbable sutures or monofilament permanent sutures are placed through the ligament. These sutures are held and left untied until any additional reconstructive procedures are completed. Ligament fixation is performed with both safety and pulley stitches (Fig. 12). In a recent study of 695 sacrospinous ligament fixation procedures, this procedure was found to be effective in vaginal apex cure to 97.0% of apex prolapse.17 If abdominal hysterectomy was indicated despite the presence of uterovaginal prolapse, abdominal sacrocolpopexy can be performed.
|
|
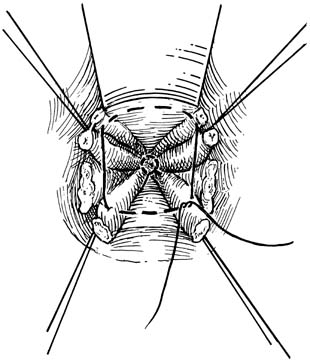
Several modifications to abdominal sacrocolpopexy have been proposed, but this discussion is limited to a single modification of two of them.18, 19 An incision is made in the peritoneum in the hollow of the sacrum from the sacral promontory downward as far posteriorly as possible. The cul-de-sac is obliterated. Three to five permanent sutures are placed in the periosteum approximately 1 cm apart. These sutures are used to hold one end of the graft (synthetic nonabsorbable material or homologous fascia) to the sacrum. The other end of the graft is sutured to the posterior wall of the exposed vaginal vault. The graft is sewn to the vaginal vault and sacral promontory periosteum. The graft is secured to the underlying serosa of the sigmoid with two or three 2-0 nonabsorbable sutures (Fig. 13).
|
Thus, the literature is replete with attempted nonsurgical and surgical management of genital prolapse. More than 1500 articles have been written on the management or prolapse. Before the 20th century, most treatments were partial or had serious drawbacks. This summary involves only a few of the anatomically corrective operations for supporting the vaginal vault. Various principles of vaginal fixation during hysterectomy are currently recognized. It is crucial for the surgeon to note the laxity of the supporting structures and attempt to repair this laxity at the initial operation. Hysterectomy offers a good opportunity to evaluate all the anatomic aspects of pelvic support and to prevent future vaginal prolapse. Attaching the pelvic supportive structures to the vagina, repairing an obvious or potential enterocele, and using appropriate adjunct procedures are some of the surgical approaches to providing support to the vaginal cuff.
VAGINAL VAULT PROLAPSE
Vaginal vault prolapse poses a challenge to the gynecologic surgeon, as evidenced by the many historic attempts to repair this condition surgically. Although more than 40 procedures have been proposed, few have succeeded in reconstructing the vagina in its normal anatomic position. This goal is of utmost importance so that the anatomy is not distorted, the patient is not predisposed to enterocele formation, and the vagina has normal function. With any reconstructive procedure, some operative failures will occur. Some of the factors that cause operative failure are unpredictable, but age, poor tissue condition, scar tissue, increased abdominal pressure, and neuropathies may prevent optimal reconstruction from taking place and lead to a less-than-perfect outcome. Every attempt should be made to restore the anatomy to its normal position. Attaching the vagina with an abdominal sacrocolpopexy or through vaginal sacrospinous fixation usually results in good anatomic restoration.
Each patient must be treated individually. If good support and function of the vagina are the desired results of operative repair of posthysterectomy prolapse, surgical techniques may vary considerably from patient to patient. However, the result remains restoration of the vagina to its normal anatomic position. Preventing recurrence is one of the goals in reconstructive surgery for vaginal vault prolapse. Recurrences frequently have the following causes: (1) an enterocele sac was ignored; (2) the vaginal vault was suspended in a position that was too far anterior, possibly to the anterior rectal wall, thereby predisposing the patient to a rapid recurrence of enterocele; (3) both of these factors may be present; and (4) the procedure was performed incorrectly.
An important consideration in selecting a procedure is whether the patient will remain sexually active. It is of paramount importance to verify that a woman is sure that she will not be sexually active if an obliterative technique is to be performed. Recent studies of the Neugebauer-Le Fort procedure20 for vaginal prolapse reported good results. However, every effort should be made to preserve vaginal function, length, and axis.
Of the more than 40 procedures for vaginal vault prolapse described over the past century, three major categories have evolved: (1) complete obliteration (colpocleisis); (2) abdominal sacrocolpopexy or vaginal sacrospinous fixation, or a modification thereof; and (3) anterior abdominal wall-ventral fixation, which rarely is used because the normal anatomy is not restored. The procedures for vaginal vault prolapse that offer the best anatomic outcome are those that already have been described: transvaginal sacrospinous fixation, transabdominal sacrocolpopexy with the use of either an artificial or a fascial graft, and a high uterosacral ligament attachment to the vagina (or a high modified McCall culdoplasty).
This section does not attempt to describe every type of repair that has been reported for this complication of hysterectomy. However, a partial review of the different types of abdominal and vaginal repairs can be found in the reference section.13,14,15,16,17,18,19,20,21,22,23,24,25 The most important consideration is that the normal anatomy is restored and the specific site or sites of damage are reconstructed properly.
It has been shown, both clinically and anatomically, that damage to the suspensory fibers that attach to the vaginal vault results in vaginal vault prolapse.26 These include the fibers that make up the endopelvic fascia of the cardinal-uterosacral ligament complex. When these fibers are destroyed, are surgically lax, or are not used for prevention of posthysterectomy prolapse at the time of hysterectomy, vaginal vault prolapse can result. Therefore, every effort should be made to reattach these fibers to the vaginal vault at the time of hysterectomy to prevent posthysterectomy prolapse.27 Theoretically, this approach should prevent prolapse in almost every case. However, diminution in the suspensory fibers, menopausal atrophy, or loss of the neural supply to this area may result in vaginal vault prolapse, and one of the techniques for anatomic repair of vault prolapse will be needed.
The numerous attempts in the literature to repair vault prolapse suggest that this condition is a significant problem for the gynecologic surgeon. Careful reconstruction of anatomy at the time of hysterectomy will prevent many posthysterectomy prolapses. However, if prolapse occurs, restoration of the normal anatomic relationships should be attempted, either transvaginally or transabdominally. In addition, any other defect that is present should be corrected at the same time. Limiting treatment to repair of the vaginal vault prolapse without correction of a cystocele, enterocele, rectocele, or paravaginal defect can result in recurrence of other anatomic hernias and failure of the initial repair. Anatomic vaginal or abdominal repair can be accomplished in this group of patients without reduction in vaginal depth, diameter, or function.
REFERENCES
Symmonds RE, Williams TJ, Lee RA, et al: Posthysterectomy enterocele and vaginal vault prolapse. Am J Obstet Gynecol 140:852, 1981 |
|
Kaser O, Ikg FA, Hirsch HA: Atlas of Gynecologic Surgery. pp 6.1-6.9, 2nd ed.. New York, Thieme-Stratton, 1985 |
|
Nichols DH, Milley PS, Randall CL: Significance of restoration of normal vaginal depth and axis. Obstet Gynecol 36:251, 1970 |
|
Cruikshank SH, Kovac SR: Role of the uterosacral-cardinal ligament in protecting the ureter during transvaginal hysterectomy. Int J Gynaecol Obstet 40:141, 1993 |
|
McCall ML: Posterior culdoplasty. Obstet Gynecol 10:595, 1957 |
|
Thompson JD, Rock JA, (eds): Telinde's Operative Gynecology. pp 720-723, Philadelphia, JB Lippincott, 1992 |
|
Cruikshank SH, Kovac SR: Randomized comparison of three surgical methods at vaginal hysterectomy to prevent enterocele. Am J Obstet Gynecol 180:859, 1999 |
|
Ranny B: Enterocele, vaginal prolapse, pelvic hernia: Recognition of treatment. Am J Obstet Gynecol 140:852, 1981 |
|
Torpin R: Excision of the cul-de-sac of Douglas for surgical care of hernias through the female caudal wall, including prolapse of uterus. J Int Coll Surg 24:322, 1955 |
|
Moschcowitz AV: The pathogenesis, anatomy, and cure of prolapse of the rectum. Surg Gynecol Obstet 15:7, 1912 |
|
Halban J: Gynakologische-Operations. 171-172, Berlin, Urban & Schwarzenberg, 1932 |
|
Cruikshank SH, Pixley RL: Surgical method of identifying the ureters during total vaginal hysterectomy. Obstet Gynecol 67:277, 1986 |
|
Bump RG, Mattiasson A, Bo K, et al: The standardization of terminology of female pelvic organ prolapse and pelvic floor function. Am J Obstet Gynecol 175:10, 1996 |
|
Cruikshank SH, Cox DW: Sacrospinous fixation at the time of transvaginal hysterectomy. Am J Obstet Gynecol 162:1611, 1990 |
|
Randall CL, Nichols DH: Surgical treatment of vaginal inversion. Obstet Gynecol 38:327, 1971 |
|
Morley GW, DeLancey JOL: Sacrospinous ligament fixation for eversion of the vagina. Am J Obstet Gynecol 158:872, 1988 |
|
Cruikshank SH, Muniz M: Outcomes study–695 sacrospinous fixations over a 16-year period, a study of the cure rates. Am J Obstet Gynecol (In Press) |
|
Lansman HA: Posthysterectomy vault prolapse: Sacral colpopexy with dura mater graft. Obstet Gynecol 63:577, 1984 |
|
Feldman GB, Birnbaum SJ: Sacral colpopexy for vaginal vault prolapse. Obstet Gynecol 53:399, 1979 |
|
Ahranjani M, Nora E, Rezai P, et al: Neugebauer–Le Fort operation for vaginal prolapse. J Reprod Med 37:959, 1992 |
|
Ridley JH: A composite vaginal vault suspension using fascia lata. Am J Obstet Gynecol 126:590, 1976 |
|
Stanton SL, Cardozo CA: Results of the colposuspension operation for incontinence and prolapse. Br J Obstet Gynaecol 86:693, 1979 |
|
Lee RA, Symmonds RE: Surgical repair at posthysterectomy vault prolapse. Am J Obstet Gynecol 112:953, 1972 |
|
Langmade CF, Oliver JA, White JS: Cooper ligament repair of vaginal vault prolapse twenty-eight years later. Am J Obstet Gyencol 131:134, 1978 |
|
Palma PCR, Pinotti JA: Endoscopic suspension of vaginal prolapse. Int J Gynaecol Obstet 27:451, 1988 |
|
DeLancey JOL: Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717, 1992 |
|
Cruikshank SH: Preventing posthysterectomy vaginal vault prolapse and enterocele during vaginal hysterectomy. Am J Obstet Gynecol 156:1433, 1987 |