Pelvic Exenteration
Authors
INTRODUCTION
Dr Alexander Brunschwig first reported pelvic exenteration in 1948 as “the most radical surgical attack so far described for pelvic cancer”.1 His procedure involved a one-staged abdominal-perineal surgery with complete en-bloc resection of the pelvic viscera, creation of an end-colostomy and bilateral ureteral implantation above the colostomy. Brunschwig developed the procedure as a means of symptomatic palliation for patients with advanced gynecologic cancer unresponsive to radiotherapy who suffered from associated complications such as fistula, infection or pain. He performed these surgeries at the risk of a high peri-operative mortality rate of 23%.1 Over time, as the procedure developed, it was recognized that the physical and psychological morbidity of exenterative surgery should not routinely justify palliation as a surgical indication, but instead should be reserved primarily as a final curative surgery for patients with advanced or refractory disease.
Traditionally, exenteration is thought of as the radical treatment of choice in certain patients with centrally located, advanced gynecologic malignancies. Although the majority of these operations are performed for recurrent or persistent squamous cell carcinoma of the cervix after radiation therapy, others have utilized exenteration for patients with recurrent endometrial, vaginal, vulvar, urethral, bladder or anorectal cancer.2, 3, 4 A small percentage of exenterations have been performed as primary therapy for other locally advanced pelvic malignancies, such as malignant melanoma, sarcoma, and carcinoma of the vulva and endometrium.5, 6, 7, 8 In some European countries such as Germany, nearly half of gynecologic oncologists would consider exenteration as a primary treatment for locally advanced cervical cancer rather than chemotherapy and radiation.9 Despite such varied applications, recurrent carcinoma of the cervix refractory to radiotherapy remains the predominant malignancy treated by exenterative surgery.
Since Brunschwig’s initial description in 1948, perioperative mortality has decreased from 23% to approximately 3–5% in more recent reports.10 Numerous modifications of exenterative technique have resulted in steady improvements in morbidity, mortality and survival (Table 1). We can also attribute these improvements to advances in intraoperative and perioperative care including better patient selection, instrumentation, routine use of prophylactic antibiotics, venous thromboembolism prophylaxis and anesthesia monitoring.11 Although we have over 60 years of experience in performing exenteration, most of the evidence we have regarding the procedure is based on retrospective case reports and case series. Ang and colleagues attempted a Cochrane review on the subject and although they identified 1311 relevant references to exenteration in the literature, they concluded that they “found no evidence to inform decisions about exenterative surgery for women.” 12
In 1969, Dr Hugh Barber first detailed indications and contraindications to pelvic exenteration after reporting poor prognosis for patients who experienced pelvic side-wall recurrences.13 Whereas traditionally, pelvic sidewall involvement was considered an absolute contraindication to exenteration,14 improvements in outcomes have prompted numerous groups to attempt more radical resections to eradicate disease and achieve negative surgical margins. Several authors now advocate for extended pelvic resections including pelvic sidewall muscle, pelvic nerve and major neural and/or major vascular structures.15, 16, 17 New developments have allowed us to examine the use of intraoperative radiation to eliminate microscopic residual disease at the time of resection.18 Our surgical armamentarium is also equipped with newer advancements in urinary and fecal diversion as well as pelvic reconstruction which can help improve quality of life for patients while reducing surgical morbidity after exenteration.19, 20, 21
Table 1. Operative mortality rates and 5-year survival for series of pelvic exenterations
Authors | Patients | Mortality | Survival |
% | % | ||
Ingersoll and Ulfelder22 | 87 | 15 | 23.3 |
Ketcham et al.23 | 162 | 7 | 38.0 |
Symmonds et al.24 | 198 | 8.1 | 33.0 |
Rutledge et al.25 | 296 | 13.5 | 42.1 |
Averette et al.26 | 92 | 23.9 | 37.0 |
Lawhead et al.27 | 65 | 9.2 | 23.0 |
Morley et al.28 | 100 | 2 | 61.0 |
Shingleton et al.29 | 143 | 6.3 | 50.0 |
| Fleisch et al.30 | 203 | 1 | 21.0 |
| Chiantera et al.31 | 230 | 3 | 38.0 |
| Goldberg et al.32 | 103 | 1 | 47.0 |
Centrally recurrent carcinoma of the cervix continues to occur despite a decrease in the percentage of patients presenting in the advanced stage and improvements in the delivery and availability of radiation therapy. The extensive radiation fibrosis that occurs after internal and external radiation for carcinoma of the cervix precludes a more conservative surgical approach to recurrent disease in the majority of cases. The close proximity of the bladder and rectum leads to fistulas or other serious complication rates (range 20–50%) when procedures such as extrafascial or radical hysterectomy are performed in this setting.33, 34, 35 Because current chemotherapy for squamous cell carcinoma is not curative, exenterative surgery remains the only and final option for a cure in women with recurrent squamous cell carcinoma in whom radiation therapy has failed.
The most commonly employed exenterative procedure is total pelvic exenteration, which consists of resection of the bladder, uterus, various portions of the vagina, and the rectosigmoid colon. Anterior exenteration involves removal of the bladder, uterus, and a portion of the anterior vagina while sparing the rectosigmoid colon. It is generally performed for smaller lesions located on the anterior cervix. Although survival rates for carefully selected patients treated with anterior exenteration can be excellent, as demonstrated by Shingleton and associates the prognosis is dismal if the surgical margins of the specimen are involved.29 When the recurrence reaches the infralevator level, the decision is made to proceed with a total pelvic exenteration with perineal phase because there is perceived a risk of rectal injury with deep rectovaginal dissection in the radiated pelvis if the rectum is not removed.2 Posterior exenteration, which spares the bladder, is seldom performed because of the high rate of genitourinary fistula formation and prolonged postoperative bladder dysfunction. Because of the difficulties in determining negative surgical margins at the time of surgery, the high complication rates, and the knowledge that few patients with involved exenterative margins will survive, total exenterations are the most frequently performed procedures.
Pelvic exenteration remains the most radical surgical procedure performed by gynecologic oncologists. As such, the operation is associated with significant morbidity. Although little has changed in the preoperative evaluation and selection of patients, advances in perioperative care and surgical techniques have continued to improve survival while concurrently decreasing life-threatening morbidity. If a patient is willing to accept the risks inherent to the procedure, the surgeon may then proceed with this potentially curative operation.
PATIENT SELECTION
A critical element in the ultimate success of this operation and cure of the patient is proper selection of candidates. Such a selection process mandates a thorough evaluation for the presence of metastatic disease; any evidence of confirmed disease outside the pelvis is an absolute contraindication to a exenterative procedure with curative intent. A chest X-ray and computed tomographic (CT) scan of the pelvis and abdomen are the minimal tests necessary for the evaluation. The CT scan provides simultaneous evaluation of the liver, retroperitoneal lymph nodes, and urinary tract and allows better evaluation of sidewall involvement by the tumor in the pelvis.29 Loss of tissue planes in the lateral pelvis indicates invasion of the tumor into the pelvic musculature. However, about one-third of patients with radiographically unresectable cancer may ultimately undergo complete pathological resection, whereas one-third of patients with radiographically resectable cancers will have residual disease on their specimen.36
The ability of whole-body 2-[18F]-fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET) scan to detect recurrence after treatment has been examined and results have been favorable. Chung et al. retrospectively evaluated 76 women diagnosed with recurrence by FDG-PET CT and found that sensitivity, specificity and accuracy of the FDG-PET scan was 96.1%, 84.4% and 91.7% respectively.37 Similarly, in a prospective series of 20 patients, Hussain et al. found PET to have a sensitivity of 100% and specificity of 73% in detecting sites of extra-pelvic metastases.38 Although the FDG-PET scan may help identify disease recurrence, it lacks the soft-tissue resolution to help with detailed preoperative planning.
Many authors advocate for the use of MRI given its superior soft-tissue enhancement especially in the previously radiated pelvis.39 Donati et al. examined 50 patients with persistent or recurrent gynecologic malignancy who had MRI prior to pelvic exenteration and found inter-observer variabililty to be minimal with excellent sensitivity (75–87.5%) and specificity (92.6–100%) for invasion of the bladder, rectum and pelvic sidewall.40 However, a recent study by Forner et al. reported poor MRI sensitivity, specificity, positive and negative predictive values for final microscopic results relative to preoperative prediction (85%, 52%, 60%, 80% respectively).41 Their conclusion was that MRI alone is insufficient to predict complete tumor resection.
Although radiographic images may suggest recurrent or persistent disease, a histologic diagnosis of disease is the only definitive way to discern postsurgical changes from recurrent disease. This prerequisite for a tissue diagnosis cannot be overemphasized. In one series, three of 65 patients deemed to have recurrent disease by physical examination, symptomatology, and radiographic interpretations had no carcinoma in the exenterative specimen.27
Evaluation of renal function and the urinary tract is essential. Some investigators have suggested that the presence of a hydroureter is a relative contraindication to surgery(13,23) Others, however, have noted that in the absence of other poor prognostic signs (e.g. pelvic sidewall fixation, bulky lesion, leg edema, pain), obstruction of a ureter is not a contraindication to proceeding with surgery.29 The function of an obstructed kidney must be evaluated before surgery because incorporating a ureter from a nonfunctioning kidney into a conduit can lead to significant infectious complications. This evaluation can easily be accomplished with a renal nucleotide scan. The clinical triad of a hydroureter, unilateral leg edema, and sciatic pain indicates a high probability of sidewall or retroperitoneal disease and may be significant enough to preclude surgical exploration in most cases.
Shingleton and associates29 were able to construct risk groups based on three clinical factors: (A) duration from initial radiation therapy to recurrence; (B) size of the central mass at the time of exenteration; and (C) preoperative suspicion of sidewall fixation. Their data suggested that patients with lesions greater than 3 cm, who underwent radiation therapy less than 1 year earlier, and who are suspected of having sidewall involvement are not good candidates for exenterative procedures and therefore should not be explored surgically. Some researchers, however, believe that every patient, especially if she is young, should undergo surgical exploration to assess resectability.24
Advanced age has previously been considered a relative contraindication to exenterative surgery, probably because older patients are more likely to have pre-existing medical conditions, such as heart disease, obstructive pulmonary disease, decreased renal function, and altered immunologic response. In a recent study by Huang and colleagues, 161 patients of all ages who underwent exenteration were found to have similar incidence of early and late complications, regardless of age.42 The absolute and relative contraindications to exenteration are presented in Table 2.
Table 2. Preoperative contraindications to exenteration in patients with recurrent cervical cancer
| Absolute |
| Distant metastases |
| Involvement of common or external iliac vessels |
| Metastases to para-aortic lymph nodes |
| Involvement of the sacrum proximal to S1 |
| Tumor extension through the sciatic foramen |
| Pelvic sidewall involvement |
| Relative |
| Ureteral obstruction |
| Poor candidate for surgery because of medical comorbidities |
| Poor candidate for surgery because of inability to care for stomas or senility |
(Adapted from Gannon CJ et al., 200743)
Despite thorough preoperative evaluation, exenterations are still aborted in 28–56.5% of cases.5, 26, 28 Peritoneal and nodal disease were the two most frequently encountered reasons cited by Miller and associates for abandoning the procedure, followed by parametrial fixation and hepatic or bowel involvement.5 The psychological trauma that follows an aborted procedure mandates thorough preoperative evaluation and counselling.
PREOPERATIVE PREPARATION
To help identify those patients likely to have difficulty managing stomas or adjusting to the social changes initiated by pelvic exenteration, preoperative preparation must include a psychosocial evaluation. The importance of this evaluation has been emphasized by Brown and associates.44 Recently, general principles of intervention in preparing patients for surgery and facilitating favorable outcomes have been developed.45 These principles include preoperative interaction of the surgeon with the patient with attention to potential problems and specific evaluation of possible acute psychiatric syndromes that may occur postoperatively, such as delirium, anxiety, depression, and brief reactive psychosis. In addition, a frank discussion of the psychosexual consequences of the surgery must be provided, preferably in the presence of the patient’s partner. Psychosis or the inability to care for oneself is a contraindication to surgery.
If the patient is to be offered neovaginal reconstruction, she must be made aware that the functional results may be disappointing. Most patients are satisfied with outcomes of reconstruction; however, quality of life and body image analysis have been cited as areas of significant concern for patients postoperatively, especially in young patients with two permanent stomata and a non-functioning vagina.46 Hawighorst-Knapstein and colleagues examined 129 patients who underwent radical hysterectomy or exenteration and reported that sexual problems attributed to the greatest reduction in terms of quality of life, especially in women with non-reconstructive surgery as well as in women who received adjuvant radiotherapy and/or chemotherapy.47
As many as 50% of hospitalized patients have clinical and laboratory evidence of malnutrition. The incidence of malnutrition in patients with recurrent cancer may be even higher. Such malnourished patients are subject to increased postoperative morbidity and mortality. Nutritional evaluation of candidates for an exenterative procedure should be performed; those patients with recent weight loss, low serum albumin, low serum transferrin, delayed hypersensitivity as determined by skin testing, and decreased skinfold thickness should be considered for preoperative hyperalimentation.48
Arterial blood gas determinations and pulmonary function studies should be mandatory for any patient with suspected pulmonary compromise. Such data can serve as a baseline for management of postoperative pulmonary complications. Patients should also undergo mechanical and antibiotic bowel preparation. Orr and colleagues reported a reduction in the risk of wound and pelvic infection by as much as 50% in those women who had a bowel preparation before exenterative surgery.48
An enterostomal therapist should visit the patient and her family before surgery. Early instruction in stoma management can help allay a patient’s anxieties regarding a stoma. It is also important to have the therapist mark the appropriate stoma site to facilitate its care after surgery. The optimal area for placement of the stoma should be marked in both the sitting and the standing positions.
THE OPERATION
The exenteration consists of three important and distinct components: determination of resectability, resection, and reconstruction. Although thorough preoperative evaluation will limit the number of patients considered for exenteration, resectability ultimately can be determined only by surgical evaluation. This criterion previously necessitated an initial exploratory laparotomy; however, several authors have demonstrated that operative laparoscopy can help identify patients with resectable compared with unresectable disease even in patients with history of prior radiation.46 Approximately 50% of patients undergoing laparotomy will have intraperitoneal or retroperitoneal metastases and are not appropriate candidates for exenteration.49 Laparoscopy is a minimally invasive tool, which may help spare patients a radical and potentially morbid procedure.50
If laparoscopy is performed and no contraindications to exenteration are noted, one then traditionally proceeds to laparotomy, although some surgeons have successfully managed to complete the surgery laparoscopically (see New surgical techniques below). After the abdomen is opened, determination of resectability includes inspection and palpation for intraperitoneal disease, evaluation of nodal status, and determination of the presence or absence of sidewall fixation. Evidence of disease on any peritoneal surfaces or metastatic disease to the para-aortic nodes is considered by most as an absolute contraindication to surgery and the procedure is typically aborted.3
The appropriateness of performing an exenteration with positive pelvic lymph nodes is debatable. Stanhope and Symmonds reported a 5-year survival rate of 23% in patients with positive nodes who underwent this procedure, thus arguing in favor of proceeding with surgery.51 Unfortunately, however, no other investigators have even approached this survival rate. Rutledge and co-workers reported a survival rate of only 7% in patients with positive pelvic nodes;25 Shingleton and associates also reported a poor survival.29 Morley and co-workers reported a 0% 5-year survival rate in patients with positive regional lymph nodes, citing this finding as a contraindication to exenteration in such patients.28 In another series, the 5-year survival rate was 9.2% for those patients with positive lymph nodes.52 Interestingly, Shingleton and associates were unable to demonstrate a difference in survival between those patients who underwent pelvic node dissection and those who did not and Benn et al. found that nodal status was not associated with time to recurrence or progression.10, 29 These findings suggest that lymph node dissection is not a mandatory component of the operation when no clinically suspicious nodes are encountered. From the available data, it would seem that positive pelvic nodes are a contraindication to pelvic exenteration.
Sidewall fixation should be evaluated and, if found, is traditionally a contraindication to surgery. This can be determined by opening the paravesical and pararectal spaces, and performing a biopsy, if necessary, to confirm the presence of disease. Shingleton and associates reported a 0% 2-year survival in patients treated with exenteration in the presence of sidewall fixation.29 This poor survival rate was confirmed by Creasman and Rutledge.53 That being said, the presence of sidewall fixation as a contraindication to surgery is being challenged with newer surgical techniques (see below).10
Once resectability has been determined, a decision regarding the feasibility of anterior exenteration versus total pelvic exenteration should be considered. Reports by Orr and coworkers48 and Symmonds and associates have shown that anterior exenteration can be performed in carefully selected patients with excellent survival and low morbidity.24 Hatch and colleagues reported a 5-year survival of 53% and an operative mortality of only 1.6% in 69 patients who underwent anterior exenterations.54 They were also able to develop criteria for identifying appropriate candidates for anterior exenteration. Women with cancer recurrence more than 1 year after radiotherapy, a lesion less than 3 cm in diameter, and no evidence of bladder invasion, were believed to be ideal candidates for anterior exenteration. These criteria would suggest that patients who are being considered for anterior exenteration should undergo a cystoscopy to rule out bladder mucosal involvement.
The major potential intraoperative complication with this procedure is hemorrhage. Blood loss generally varies from 2300 to 4000 mL (median 3000 cc) in most reports but can be much greater.55 Ketcham and coworkers reported increased mortality in patients with intraoperative blood loss greater than 3000 mL.23 Intraoperative monitoring with a pulmonary catheter should be considered in all patients undergoing pelvic exenteration. This has been shown to aid considerably in the management of intraoperative fluid replacement, which can exceed 1500 mL/h.56
After resection of the tumor, attention must be given to reconstruction. This includes urinary reconstruction, covering of the denuded pelvic floor, reconstruction of the vagina, and consideration of reanastomosis of the colon and rectum versus protective colostomy, where appropriate.
Construction of a urinary conduit
The first attempts at urinary diversion consisted of wet colostomies and rectal bladders. These were soon abandoned because of frequent and life-threatening urinary tract infection as well as serious metabolic side-effects including hyperchloremic acidosis as a result of fecal contamination of urine.46 More contemporary options include orthotopic neobladder reconstruction, or supravesicular urinary diversion with continent pouches or incontinent conduits using a segment of autologous bowel. However, these approaches carry their own challenges including anastomotic breakdown, infection, ureteric stricture, pouch leakage, stone formation, incontinence and renal dysfunction.57
In orthotopic neobladder reconstruction, a segment of bowel is used as a urinary reservoir and is anastamosed to the urethra to avoid the need for a urostomy on the anterior abdominal wall. This is an appealing concept as it may afford long-term continence to 80% patients undergoing exenteration.19 That being said, many authors do not recommend the orthotopic neobladder because of the extent the anterior vaginal wall, pubo-urethral ligaments and endopelvic fascia that will need to be spared with this approach as well as the high risk of urinary fistula after prior radiotherapy and high local recurrence rate.58 In a series of 29 women undergoing orthotopic reconstruction after anterior exenteration, 32% developed fistula and required surgical conversion for definitive treatment.59 Because of this, most surgeons construct continent pouches of incontinent conduits at the time of exenteration.
Bricker described the first urinary conduit in 1950.60 The Bricker ileal conduit remains the most commonly performed urinary diversion procedure and is used in approximately half of all exenterations currently performed.19 The ileum and sigmoid bowel segments have often received significant amounts of radiation before the procedure, resulting in a high rate of intestinal and conduit complications. Therefore, some surgeons use a segment of non-irradiated transverse colon.46 Orr and colleagues showed a significant reduction in urinary leaks and gastrointestinal complications with transverse colon conduits.61 Morley and co-workers prefer the sigmoid conduit because it avoids an anastomosis (28) . Several authors have recommended the routine use of ureteral stents to decrease technical error during conduit construction and to protect against urinary strictures.61, 62
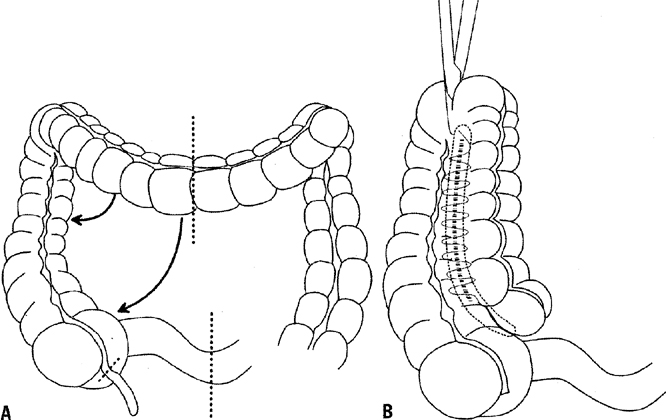
At several institutions, ileal and colonic conduits have been replaced with continent urinary diversions. These continent conduits more closely simulate the normal lower urinary tract system with a low-pressure system and a urine capacity approximating that of a normal bladder. They do not require an external collection device and, ideally, are not subject to reflux. Such techniques are the result of refinements of the pioneering works of Gilchrist et al. and Kock and associates.63, 64 Expanding on these works, Rowland and colleagues demonstrated that the ileocecal valve could be used for recurrent, intermittent catheterization.65 Numerous variations of continent urinary diversions have subsequently been developed, including the Kock, Mainz, Mainz II, Indiana, Miami, Penn, and supracecal colonic continent urostomy (SCCCU) pouches.64, 66, 67, 68, 69, 70, 71 One of these techniques, the Miami pouch, is illustrated in Fig. 1. None of these procedures appears to be superior to the others and overall, they carry a late complication rate of approximately 46%.58 No controlled prospective trial has demonstrated whether continent ileocecal pouches such as the Mainz or the Miami pouches have higher complication rates compared with un-irradiated continent pouches from the ascending, transverse or descending colons.46 The approach to surgery should ultimately be guided by the underlying disease, patient’s personal preference and skill of the responsible surgeon.72
Early and late complications of continent urinary reservoirs appear to be similar for all types described. Common complications include ureteral stricture/obstruction (early and late), anastomotic leak (early), sepsis (early), and urinary stone formation (late). Operative mortality rates from early complications have been reported to be as high as 9%.73 Importantly, these operations require judicious patient selection, despite the suggestion that they can be performed in half of patients undergoing exenteration.67 Appropriate candidates should be highly motivated and possess the manual dexterity to care for the continence mechanisms. In addition, continent diversions are inappropriate for patients with compromised renal function. Whichever continence mechanism is employed, the benefits derived from these procedures must be weighed against the disadvantages of more extensive surgery, a longer length of operation, and a greater rate of surgical and postoperative complications.
Covering the denuded pelvic floor
After the exenterative procedure, the denuded raw pelvic floor must be covered to avoid infectious and gastrointestinal complications. The true pelvis has lateral borders composed mostly of bone and cannot collapse to fill surgically created defects. Although grafts constructed of foreign materials such as mesh have been used for covering the denuded pelvic floor, this carries a 72% rate of infection and fistula in patients with prior radiotherapy.46 The optimal closure of the pelvis is probably accomplished with a technique that brings in a new blood supply. Transposition of an omental pedicle, as demonstrated by Powers and colleagues, meets this criterion and helps exclude the small bowel from further radiation and prevent entrapment in the pelvis.74, 75 Other methods of closing the pelvis include reanastomosis of the colon and rectum, as reported by Berek and associates, and use of a myocutaneous flap as part of vaginal reconstruction, as reported by Hatch.76, 77 Others have used a peritoneal patch or graft with good results.28 Said et al. examined the use of Human Acellular Dermal Matrix (HADM), commonly used for reconstruction in other torso locations, and found that it was associated with lower rates of complications (including infection, adhesions, and cutaneous exposure) than synthetic mesh.78
Vaginal reconstruction
Consideration of vaginal reconstruction should be made before the operation. This must be discussed with the patient to determine the desirability of maintaining sexual function. Lack of sexual desire, advanced age, or lack of a sexual partner may lead the patient to decide not to undergo vaginal reconstruction. The following are among the numerous methods of postexenteration vaginal reconstruction: split-thickness skin grafts, myocutaneous flaps, sigmoid vaginostomy, vulvovaginoplasty, ileal vagina, and amnion grafts.
Gracilis myocutaneous flaps historically were very popular but have been shown to have a high rate of necrosis, poor healing and vaginal prolapse. The inferior gluteal flap has been described with excellent results and no late complications.79 Transversely or vertically oriented rectus abdominis myocutaneous (TRAM or VRAM) flaps have also become much more common. They have the advantage of using the primary incision, require only one donor site, have a large vascular pedicle and have a large arc of rotation. They also improve leukocyte delivery, increase oxygen tension and reduce risk of infection in the perineal wound.80 The most commonly reported complication with this approach is flap dehiscence, which has been reported as high as 65%.81 Berger and colleagues recently described 46 patients who had VRAM flaps and only 19.6% experienced flap complications compared with reported rates of gracilis flap necrosis of up to 37%.82 In a series of patients presented by Goldberg and colleagues, 90% of patients were sexually active after VRAM reconstruction and 81% of patients reported they would have the procedure again.83 These approaches still face challenges including stenosis (even with dilatation), lack of lubrication and inadequate length.20
Reanastomosis of the colon and rectum
In patients who have undergone total pelvic exenteration, consideration should be given to reanastomosis of the colon and rectum. The development of the end-to-end circular stapling device has allowed the anastomosis of the colon to as little as 3–4 cm of rectal stump. Berek and associates reported good results with this technique, but recommended a diverting colostomy in previously irradiated patients.77 Husain and co-workers noted a greater than 50% rate of anastomotic leaks in patients undergoing concomitant low rectal anastomosis.84 However, Forner et al. found no correlation between preceeding radiotherapy or chemotherapy and the frequency of breakdown of rectal anastomosis in a series of 91 patients.85 Hatch and associates reported success with reanastamosis, but recommended bowel rest with 14 days of total parenteral nutrition instead of a diverting colostomy.86 An omental wrap of the anastomosis site was also recommended. They noted that most leaks were posterior and believed that it was important to cover this area with the omentum. The reservoir capacity of the rectum is reduced, and frequent defecation can be a problem after surgery. Hatch and associates recommended diphenoxylate and atropine sulfate (Lomotil) or loperamide (Imodium) every 2 hours until stool frequency is satisfactory.86 This problem usually diminishes with time, making consideration of reanastomosis reasonable. Frequent defecation as well as rectal tenesmus, which is another side-effect of a low end-to-end anastomosis of the colon to rectum, can be reduced through the construction of a rectal J-pouch low-pressure reservoir, possibly obviating the need for antidiarrheal medication.87
POSTOPERATIVE CARE
Patients who have undergone exenterative surgery should be placed in an intensive care unit and monitored closely.88 The advantages of a pulmonary artery catheter over a central venous catheter are well documented.56 Many of these patients will be unable to tolerate significant oral intake for a number of days after surgery. Orr and colleagues demonstrated a reduction in postoperative weight loss from 10.6% of total body weight to 1.8% in patients who received parenteral and enteral hyperalimentation after exenterative surgery.89
As expected with surgery of this magnitude, postoperative complications after exenterations are common. Febrile morbidity is the most frequently encountered complication, occurring in 75–85% of patients. Potential causes include pulmonary sources, pelvic cellulitis and abscess, wound infection, and occasionally, pelvic septic thrombophlebitis. Symptomatic pulmonary emboli occur in 1–5% of patients and, therefore, efforts should be made in the perioperative period to reduce the possibility of a pulmonary embolus.88 This may be accomplished by prophylactic low-dose heparin therapy or by a pneumatic antiembolic compression hose. Pyelonephritis after exenteration occurs between 5% and 20% of the time.48 Almost all conduits are colonized with bacteria within 1 week after surgery, making an accurate diagnosis difficult. The routine use of both prophylactic antibiotics and subcutaneous heparin has been shown to reduce the morbidity from pelvic exenteration.90
The most serious complication, because of its associated mortality and morbidity, is gastrointestinal obstruction or fistula. Reoperation for small bowel fistula is reported to have a perioperative mortality rate of 30–40%.91 For those patients surviving a fistula, long-term side-effects include short bowel syndrome, persistent pelvic drainage, and chronic diarrhea.92 Rectovaginal fistula may occur after anterior exenteration and also carries a significant mortality rate.28, 48 Every effort should be made in the preoperative evaluation and during the operation to avoid these potential complications.
NEW SURGICAL TECHNIQUES
Laterally extended endopelvic resection (LEER) has received attention as a new operation to treat infrailiac pelvic wall recurrences. This particular procedure utilizes the idea that most recurrent sidewall carcinoma does not invade the adjacent striated muscle and therefore inclusion of the pelvic side wall muscles in the surgical specimen will result in tumor-free margins.50 In his description of the procedure, Hockel extends the lateral resection plane of pelvic exenteration to include parietal fat pad, obturator internus, pubococcygeus, iliococcygeus, and cocygeus. The procedure is not indicated for parietal disease above the level of the obturator nerve and the sciatic foramen.93 In a series of 91 patients treated with LEER, locoregional control was achieved in 92% of the cases with a 5-year overall survival of 61%.17 Patients treated with LEER resections have similar reported disease-free survival, overall survival and complication rates compared with patients who have traditional exenterative resections.94
Some investigators have extended resection even further to include portion of pelvic bone, major neural and vascular structures including the common and/or external iliac vessels in an attempt to achieve negative pathologic margins.16 Andiyakan et al. described 22 patients who underwent extended pelvic resections and 77% achieved negative margins with 48% overall survival in patients with complete pathologic resection.15 Caceres et al. reported similar outcomes in 14 patients of whom 11 (78%) achieved a complete resection with negative surgical margins.11 As experience evolves with exenteration and postoperative survival and morbidity improve, we are likely to see a concurrent increase in the number of more radical procedures attempted to eradicate disease.
The addition of intraoperative radiation at the time of exenteration, either in the form of external beam radiation by linear accelerator or high dose rate interstitial brachytherapy, has been examined to potentially reduce local recurrence, especially in those patients with microscopic or close margins at the time of pelvic exenteration.95, 96, 97 The preliminary findings are still variable, and further study is warranted at this time. Backes et al. recently published a series of 21 patients who received intraoperative radiation therapy and failed to demonstrate superior outcomes.18 The data from Memorial Sloan Kettering describe 17 patients who received intraoperative radiation in whom local control was obtained for 83% of patients with no gross residual disease.3 More data are required to make definitive recommendations regarding this interesting adjunctive treatment.
Finally, there have been several studies published by surgeons who have been able to complete pelvic exenteration laparoscopically. In 2003, Pomel et al. reported the first laparoscopic exenteration and 6 years later Lim et al. reported the first robotic assisted laparoscopic exenteration.98, 99 Recently, Iavazzo et al. published the largest series of eight patients undergoing robotic anterior exenteration. They boasted an average OR time of 375–600 minutes, an average estimated blood loss of 200–550 cc and short duration of hospitalization between 3 and 53 days.100 These authors acknowledge that the open approach remains the gold standard in terms of exenterative technique, however, the development of minimal invasive approaches represents a significant advancement in surgery for cervical cancer.
SUMMARY
Pelvic exenteration continues to be a challenge to surgeons who undertake the care of women with pelvic cancer. It provides the only hope for cure in women with pelvic malignancies that recur after radiation therapy. The potential for significant morbidity and even death secondary to this procedure should always be kept in mind and should guide in the selection of candidates for this operation.
REFERENCES
Brunschwig A. Complete excision of pelvic viscera for advanced carcinoma; a one-stage abdominoperineal operation with end colostomy and bilateral ureteral implantation into the colon above the colostomy. Cancer 1948 Jul;1(2):177-183. |
|
Andikyan V, Khoury-Collado F, Gerst SR, Talukdar S, Bochner BH, Sandhu JS, et al. Anterior pelvic exenteration with total vaginectomy for recurrent or persistent genitourinary malignancies: review of surgical technique, complications, and outcome. Gynecol Oncol 2012 Sep;126(3):346-350. |
|
Chi DS, Barakat RR. Surgical management of advanced or recurrent endometrial cancer. Surg Clin North Am 2001 Aug;81(4):885-896. |
|
Chokshi RJ, Fowler J, Cohn D, Bahnson R, Lumbley J, Martin EW Jr. A single-institution approach to total pelvic exenteration. Am Surg 2011 Dec;77(12):1629-1639. |
|
Miller B, Morris M, Levenback C, Burke TW, Gershenson DM. Pelvic exenteration for primary and recurrent vulvar cancer. Gynecol Oncol 1995 Aug;58(2):202-205. |
|
Geisler JP, Look KY, Moore DA, Sutton GP. Pelvic exenteration for malignant melanomas of the vagina or urethra with over 3 mm of invasion. Gynecol Oncol 1995 Dec;59(3):338-341 |
|
Morris M, Alvarez RD, Kinney WK, Wilson TO. Treatment of recurrent adenocarcinoma of the endometrium with pelvic exenteration. Gynecol Oncol 1996 Feb;60(2):288-291 |
|
Barakat RR, Goldman NA, Patel DA, Venkatraman ES, Curtin JP. Pelvic exenteration for recurrent endometrial cancer. Gynecol Oncol 1999 Oct;75(1):99-102 |
|
Forner DM, Lampe B. Exenteration as a primary treatment for locally advanced cervical cancer: long-term results and prognostic factors. American Journal of Obstetrics & Gynecology 2011 Aug;205(2):148.e1-148.e6. |
|
Benn T, Brooks RA, Zhang Q, Powell MA, Thaker PH, Mutch DG, et al. Pelvic exenteration in gynecologic oncology: a single institution study over 20 years. Gynecol Oncol 2011 Jul;122(1):14-18. |
|
Caceres A, Mourton SM, Bochner BH, Gerst SR, Liu L, Alektiar KM, et al. Extended pelvic resections for recurrent uterine and cervical cancer: out-of-the-box surgery. International Journal of Gynecological Cancer 2008 Sep-Oct;18(5):1139-1144 |
|
Ang C, Bryant A, Barton DP, Pomel C, Naik R. Exenterative surgery for recurrent gynaecological malignancies. Cochrane Database of Systematic Reviews 2014;2:010449. |
|
Barber HR. Relative prognostic significance of preoperative and operative findings in pelvic exenteration. Surg Clin North Am 1969 Apr;49(2):431-447. |
|
Mattingly RF. Indications, contraindications, and method of total pelvic exenteration. Oncology 1967;21(4):241-259. |
|
Andikyan V, Khoury-Collado F, Sonoda Y, Gerst SR, Alektiar KM, Sandhu JS, et al. Extended pelvic resections for recurrent or persistent uterine and cervical malignancies: an update on out of the box surgery. Gynecol Oncol 2012 May;125(2):404-408. |
|
Chi DS, Caceres A, Boland PJ. Extended pelvic resection of iliacus muscle and femoral nerve for isolated recurrent uterine cancer. Gynecol Oncol 2007 Feb;104(2 Suppl 1):48-49. |
|
Hockel M, Horn LC, Einenkel J. (Laterally) extended endopelvic resection: surgical treatment of locally advanced and recurrent cancer of the uterine cervix and vagina based on ontogenetic anatomy. Gynecol Oncol 2012 Nov;127(2):297-302. |
|
Backes FJ, Billingsley CC, Martin DD, Tierney BJ, Eisenhauer EL, Cohn DE, et al. Does intra-operative radiation at the time of pelvic exenteration improve survival for patients with recurrent, previously irradiated cervical, vaginal, or vulvar cancer?. Gynecol Oncol 2014 Oct;135(1):95-99. |
|
Chiva LM, Lapuente F, Nunez C, Ramirez PT. Ileal orthotopic neobladder after pelvic exenteration for cervical cancer. Gynecol Oncol 2009 Apr;113(1):47-51. |
|
Ferrari JP, Hemphill AF, Xu J, DeJesus RA. Modified rotational bowel vaginoplasty after total pelvic exenteration. Ann Plast Surg 2013 Mar;70(3):335-336. |
|
Fowler JM. Incorporating pelvic/vaginal reconstruction into radical pelvic surgery. Gynecol Oncol 2009 Oct;115(1):154-163. |
|
Ingersoll FM, Ulfelder H. Pelvic exenteration for carcinoma of the cervix. N Engl J Med 1966 Mar 24;274(12):648-651. |
|
Ketcham AS, Deckers PJ, Sugarbaker EV, Hoye RC, Thomas LB, Smith RR. Pelvic exenteration for carcinoma of the uterine cervix. A 15-year experience. Cancer 1970 Sep;26(3):513-521. |
|
Symmonds RE, Pratt JH, Webb MJ. Exenterative operations: experience with 198 patients. American Journal of Obstetrics & Gynecology 1975 Apr 1;121(7):907-918. |
|
Rutledge FN, Smith JP, Wharton JT, O'Quinn AG. Pelvic exenteration: analysis of 296 patients. American Journal of Obstetrics & Gynecology 1977 Dec 15;129(8):881-892. |
|
Averette HE, Lichtinger M, Sevin BU, Girtanner RE. Pelvic exenteration: a 15-year experience in a general metropolitan hospital. American Journal of Obstetrics & Gynecology 1984 Sep 15;150(2):179-184 |
|
Lawhead RA Jr, Clark DG, Smith DH, Pierce VK, Lewis JL Jr. Pelvic exenteration for recurrent or persistent gynecologic malignancies: a 10-year review of the Memorial Sloan-Kettering Cancer Center experience (1972-1981). Gynecol Oncol 1989 Jun;33(3):279-282 |
|
Morley GW, Hopkins MP, Lindenauer SM, Roberts JA. Pelvic exenteration, University of Michigan: 100 patients at 5 years. Obstetrics & Gynecology 1989 Dec;74(6):934-943. |
|
Shingleton HM, Soong SJ, Gelder MS, Hatch KD, Baker VV, Austin JM Jr. Clinical and histopathologic factors predicting recurrence and survival after pelvic exenteration for cancer of the cervix. Obstetrics & Gynecology 1989 Jun;73(6):1027-1034. |
|
Fleisch MC, Pantke P, Beckmann MW, Schnuerch HG, Ackermann R, Grimm MO, et al. Predictors for long-term survival after interdisciplinary salvage surgery for advanced or recurrent gynecologic cancers. J Surg Oncol 2007 May 1;95(6):476-484 |
|
Chiantera V, Rossi M, De Iaco P, Koehler C, Marnitz S, Fagotti A, et al. Morbidity after pelvic exenteration for gynecological malignancies: a retrospective multicentric study of 230 patients. International Journal of Gynecological Cancer 2014 Jan;24(1):156-164. |
|
Goldberg GL, Sukumvanich P, Einstein MH, Smith HO, Anderson PS, Fields AL. Total pelvic exenteration: the Albert Einstein College of Medicine/Montefiore Medical Center Experience (1987 to 2003). Gynecol Oncol 2006 May;101(2):261-268. |
|
Rubin SC, Hoskins WJ, Lewis JL Jr. Radical hysterectomy for recurrent cervical cancer following radiation therapy. Gynecol Oncol 1987 Jul;27(3):316-324. |
|
Terada K, Morley GW. Radical hysterectomy as surgical salvage therapy for gynecologic malignancy. Obstetrics & Gynecology 1987 Dec;70(6):913-915. |
|
Adcock LL. Radical hysterectomy preceded by pelvic irradiation. Gynecol Oncol 1979 Oct;8(2):152-163. |
|
Jurado M, Alcazar JL, Martinez-Monge R. Resectability rates of previously irradiated recurrent cervical cancer (PIRCC) treated with pelvic exenteration: is still the clinical involvement of the pelvis wall a real contraindication? a twenty-year experience. Gynecol Oncol 2010 Jan;116(1):38-43. |
|
Chung HH, Kim SK, Kim TH, Lee S, Kang KW, Kim JY, et al. Clinical impact of FDG-PET imaging in post-therapy surveillance of uterine cervical cancer: from diagnosis to prognosis. Gynecol Oncol 2006 Oct;103(1):165-170. |
|
Husain A, Akhurst T, Larson S, Alektiar K, Barakat RR, Chi DS. A prospective study of the accuracy of 18Fluorodeoxyglucose positron emission tomography (18FDG PET) in identifying sites of metastasis prior to pelvic exenteration. Gynecol Oncol 2007 Jul;106(1):177-180. |
|
Hricak H, Hamm B, Semelka RC, Cann CE, Nauert T, Secaf E, et al. Carcinoma of the uterus: use of gadopentetate dimeglumine in MR imaging. Radiology 1991 Oct;181(1):95-106. |
|
Donati OF, Lakhman Y, Sala E, Burger IA, Vargas HA, Goldman DA, et al. Role of preoperative MR imaging in the evaluation of patients with persistent or recurrent gynaecological malignancies before pelvic exenteration. Eur Radiol 2013 Oct;23(10):2906-2915. |
|
Forner DM, Meyer A, Lampe B. Preoperative assessment of complete tumour resection by magnetic resonance imaging in patients undergoing pelvic exenteration. European Journal of Obstetrics, Gynecology, & Reproductive Biology 2010 Feb;148(2):182-185. |
|
Huang M, Iglesias DA, Westin SN, Fellman B, Urbauer D, Schmeler KM, et al. Pelvic exenteration: impact of age on surgical and oncologic outcomes. Gynecol Oncol 2014 Jan;132(1):114-118. |
|
Gannon CJ, Zager JS, Chang GJ, Feig BW, Wood CG, Skibber JM, et al. Pelvic exenteration affords safe and durable treatment for locally advanced rectal carcinoma. Annals of Surgical Oncology 2007 Jun;14(6):1870-1877 |
|
Brown KG, Koh CE, Vasilaras A, Eisinger D, Solomon MJ. Clinical algorithms for the diagnosis and management of urological leaks following pelvic exenteration. European Journal of Surgical Oncology 2014 Jun;40(6):775-781 |
|
Turns D. Psychosocial issues: pelvic exenterative surgery. J Surg Oncol 2001 Mar;76(3):224-236. |
|
Hockel M, Dornhofer N. Pelvic exenteration for gynaecological tumours: achievements and unanswered questions. Lancet Oncology 2006 Oct;7(10):837-847 |
|
Hawighorst-Knapstein S, Fusshoeller C, Franz C, Trautmann K, Schmidt M, Pilch H, et al. The impact of treatment for genital cancer on quality of life and body image--results of a prospective longitudinal 10-year study. Gynecol Oncol 2004 Aug;94(2):398-403 |
|
Orr JW Jr, Shingleton HM, Hatch KD, Taylor PT, Partridge EE, Soong SJ. Gastrointestinal complications associated with pelvic exenteration. American Journal of Obstetrics & Gynecology 1983 Feb 1;145(3):325-332 |
|
Cho JE, Liu C, Gossner G, Nezhat FR. Laparoscopy and gynecologic oncology. Clinical Obstetrics & Gynecology 2009 Sep;52(3):313-326. |
|
Hockel M. Surgical treatment of locally advanced and recurrent cervical carcinoma: overview on current standard and new developments. Onkologie 2003 Oct;26(5):452-455 |
|
Stanhope CR, Symmonds RE. Palliative exenteration--what, when, and why?. American Journal of Obstetrics & Gynecology 1985 May 1;152(1):12-16. |
|
Jones WB. Surgical approaches for advanced or recurrent cancer of the cervix. Cancer 1987 Oct 15;60(8 Suppl):2094-2103. |
|
Creasman WT, Rutledge F. Preoperative evaluation of patients with recurrent carcinoma of the cervix. Gynecol Oncol 1972 Nov;1(1):111-118 |
|
Hatch KD, Shingleton HM, Soong SJ, Baker VV, Gelder MS. Anterior pelvic exenteration. Gynecol Oncol 1988 Sep;31(1):205-216 |
|
Hope JM, Pothuri B. The role of palliative surgery in gynecologic cancer cases. Oncologist 2013;18(1):73-79. |
|
Orr JW Jr, Shingleton HM, Soong SJ, Hatch KD, Bryant JW, Partridge EE, et al. Hemodynamic parameters following pelvic exenteration. American Journal of Obstetrics & Gynecology 1983 Aug 15;146(8):882-892. |
|
Backes FJ, Tierney BJ, Eisenhauer EL, Bahnson RR, Cohn DE, Fowler JM. Complications after double-barreled wet colostomy compared to separate urinary and fecal diversion during pelvic exenteration: time to change back?. Gynecol Oncol 2013 Jan;128(1):60-64. |
|
Karsenty G, Moutardier V, Lelong B, Guiramand J, Houvenaeghel G, Delpero JR, et al. Long-term follow-up of continent urinary diversion after pelvic exenteration for gynecologic malignancies. Gynecol Oncol 2005 May;97(2):524-528. |
|
Ungar L, Palfalvi L. Pelvic exenteration without external urinary or fecal diversion in gynecological cancer patients. International Journal of Gynecological Cancer 2006 Jan-Feb;16(1):364-368. |
|
Bricker EM. Bladder substitution after pelvic evisceration. Surg Clin North Am 1950 Oct;30(5):1511-1521. |
|
Orr JW Jr, Shingleton HM, Hatch KD, Taylor PT, Austin JM Jr, Partridge EE, et al. Urinary diversion in patients undergoing pelvic exenteration. American Journal of Obstetrics & Gynecology 1982 Apr 1;142(7):883-889. |
|
Schlesinger RE, Berman ML, Ballon SC, Lagasse LD, Watring WG, Futoran RJ, et al. The choice of an intestinal segment for a urinary conduit. Surg Gynecol Obstet 1979 Jan;148(1):45-48. |
|
Gilchrist Rk, Merricks Jw, Hamlin Hh, Rieger it. Construction of a substitute bladder and urethra. Surg Gynecol Obstet 1950 Jun;90(6):752-760. |
|
Kock NG, Nilson AE, Nilsson LO, Norlen LJ, Philipson BM. Urinary diversion via a continent ileal reservoir: clinical results in 12 patients. J Urol 1982 Sep;128(3):469-475. |
|
Rowland RG, Mitchell ME, Bihrle R. Alternative techniques for a continent urinary reservoir. Urol Clin North Am 1987 Nov;14(4):797-804 |
|
Thuroff JW, Alken P, Riedmiller H, Engelmann U, Jacobi GH, Hohenfellner R. The Mainz pouch (mixed augmentation ileum and cecum) for bladder augmentation and continent diversion. J Urol 1986 Jul;136(1):17-26. |
|
Penalver MA, Bejany DE, Averette HE, Donato DM, Sevin BU, Suarez G. Continent urinary diversion in gynecologic oncology. Gynecol Oncol 1989 Sep;34(3):274-288. |
|
Duckett JW, Snyder HM 3rd. Use of the Mitrofanoff principle in urinary reconstruction. Urol Clin North Am 1986 May;13(2):271-274. |
|
Rowland RG, Mitchell ME, Bihrle R, Kahnoski RJ, Piser JE. Indiana continent urinary reservoir. J Urol 1987 Jun;137(6):1136-1139. |
|
Silver DF, Ashwell TR. Choices in creating continent urostomies following pelvic exenteration for gynecologic malignancies. Gynecol Oncol 2001 Sep;82(3):510-515. |
|
El-Lamie IK. Preliminary experience with Mainz type II pouch in gynecologic oncology patients. Eur J Gynaecol Oncol 2001;22(1):77-80. |
|
Forner DM, Lampe B. Ileal conduit and continent ileocecal pouch for patients undergoing pelvic exenteration: comparison of complications and quality of life. International Journal of Gynecological Cancer 2011 Feb;21(2):403-408. |
|
Penalver MA, Angioli R, Mirhashemi R, Malik R. Management of early and late complications of ileocolonic continent urinary reservoir (Miami pouch). Gynecol Oncol 1998 Jun;69(3):185-191. |
|
Galandiuk S, Jorden J, Mahid S, McCafferty MH, Tobin G. The use of tissue flaps as an adjunct to pelvic surgery. Am J Surg 2005 Aug;190(2):186-190. |
|
Powers JC, Fitzgerald JF, McAlvanah MJ. The anatomic basis for the surgical detachment of the greater omentum from the transverse colon. Surg Gynecol Obstet 1976 Jul;143(1):105-106. |
|
Hatch KD. Construction of a neovagina after exenteration using the vulvobulbocavernosus myocutaneous graft. Obstetrics & Gynecology 1984 Jan;63(1):110-114. |
|
Berek JS, Hacker NF, Lagasse LD. Rectosigmoid colectomy and reanastomosis to facilitate resection of primary and recurrent gynecologic cancer. Obstetrics & Gynecology 1984 Nov;64(5):715-720. |
|
Said HK, Bevers M, Butler CE. Reconstruction of the pelvic floor and perineum with human acellular dermal matrix and thigh flaps following pelvic exenteration. Gynecol Oncol 2007 Dec;107(3):578-582. |
|
Loree TR, Hempling RE, Eltabbakh GH, Recio FO, Piver MS. The inferior gluteal flap in the difficult vulvar and perineal reconstruction. Gynecol Oncol 1997 Sep;66(3):429-434. |
|
Chessin DB, Hartley J, Cohen AM, Mazumdar M, Cordeiro P, Disa J, et al. Rectus flap reconstruction decreases perineal wound complications after pelvic chemoradiation and surgery: a cohort study. Annals of Surgical Oncology 2005 Feb;12(2):104-110. |
|
Chokshi RJ, Kuhrt MP, Arrese D, Martin EW Jr. Reconstruction of total pelvic exenteration defects with rectus abdominus myocutaneous flaps versus primary closure. Am J Surg 2013 Jan;205(1):64-70. |
|
Berger JL, Westin SN, Fellman B, Rallapali V, Frumovitz M, Ramirez PT, et al. Modified vertical rectus abdominis myocutaneous flap vaginal reconstruction: an analysis of surgical outcomes. Gynecol Oncol 2012 Apr;125(1):252-255. |
|
Goldberg GL. Total pelvic exenteration: the reconstructive phase. Gynecol Oncol 2005 Dec;99(3 Suppl 1):S149. |
|
Husain A, Curtin J, Brown C, Chi D, Hoskins W, Poynor E, et al. Continent urinary diversion and low-rectal anastomosis in patients undergoing exenterative procedures for recurrent gynecologic malignancies. Gynecol Oncol 2000 Aug;78(2):208-211. |
|
Forner DM, Lampe B. Intestinal complications after pelvic exenterations in gynecologic oncology. International Journal of Gynecological Cancer 2009 Jul;19(5):958-962. |
|
Hatch KD, Shingleton HM, Potter ME, Baker VV. Low rectal resection and anastomosis at the time of pelvic exenteration. Gynecol Oncol 1988 Oct;31(2):262-267. |
|
Wheeless CR Jr, Hempling RE. Rectal J-pouch reservoir to decrease the frequency of tenesmus and defecation in low coloproctostomy. Gynecol Oncol 1989 Sep;34(3):379-382. |
|
Girtanner RE, De Campo T, Alleyn JN, Averette HE. Routine intensive care for pelvic exenterative operations. Surg Gynecol Obstet 1981 Nov;153(5):657-659. |
|
Orr JW Jr, Shingleton HM. Importance of nutritional assessment and support in surgical and cancer patients. J Reprod Med 1984 Sep;29(9):635-650. |
|
Goldberg JM, Piver MS, Hempling RE, Aiduk C, Blumenson L, Recio FO. Improvements in pelvic exenteration: factors responsible for reducing morbidity and mortality. Annals of Surgical Oncology 1998 Jul-Aug;5(5):399-406. |
|
Devereux DF, Sears HF, Ketcham AS. Intestinal fistula following pelvic exenterative surgery: predisposing causes and treatment. J Surg Oncol 1980;14(3):227-234. |
|
Miller B, Morris M, Gershenson DM, Levenback CL, Burke TW. Intestinal fistulae formation following pelvic exenteration: a review of the University of Texas M. D. Anderson Cancer Center experience, 1957-1990. Gynecol Oncol 1995 Feb;56(2):207-210. |
|
Hockel M. Laterally extended endopelvic resection (LEER)--principles and practice. Gynecol Oncol 2008 Nov;111(2 Suppl):S13-7. |
|
Hockel M. Laterally extended endopelvic resection. Novel surgical treatment of locally recurrent cervical carcinoma involving the pelvic side wall. Gynecol Oncol 2003 Nov;91(2):369-377. |
|
Beitler JJ, Anderson PS, Wadler S, Runowicz CD, Hayes MK, Fields AL, et al. Pelvic exenteration for cervix cancer: would additional intraoperative interstitial brachytherapy improve survival?. Int J Radiat Oncol Biol Phys 1997 Apr 1;38(1):143-148. |
|
Crowe PJ, Temple WJ, Lopez MJ, Ketcham AS. Pelvic exenteration for advanced pelvic malignancy. Semin Surg Oncol 1999 Oct-Nov;17(3):152-160. |
|
Chi DS, Gemignani ML, Curtin JP, Hoskins WJ. Long-term experience in the surgical management of cancer of the uterine cervix. Semin Surg Oncol 1999 Oct-Nov;17(3):161-167. |
|
Pomel C, Rouzier R, Pocard M, Thoury A, Sideris L, Morice P, et al. Laparoscopic total pelvic exenteration for cervical cancer relapse. Gynecol Oncol 2003 Dec;91(3):616-618. |
|
Lim PC. Robotic assisted total pelvic exenteration: a case report. Gynecol Oncol 2009 Nov;115(2):310-311 |
|
Iavazzo C, Gkegkes ID. Robotic technology for pelvic exenteration in cases of cervical cancer. International Journal of Gynaecology & Obstetrics 2014 Apr;125(1):15-17. |