Simple Operations of the Vulva
Authors
INTRODUCTION
Numerous procedures available to the gynecologist for diagnosis and management of vulvar processes are adequately and appropriately addressed in a clinic or ambulatory care setting. The choice of an office versus an ambulatory operating room facility is generally based on the degree of surgical dissection required, the availability of appropriate instrumentation, and the level of anesthesia necessary for adequate patient comfort. The surgical procedures presented in this chapter are grouped by disease processes, as this grouping best explains their appropriate use in the clinical setting.
INFECTIOUS PROCESSES
Infections of the vulva are commonly due to bacteria that inhabit the skin, causing diseases such as carbuncles, furuncles, pyodermatitis, erysipelas, and impetigo. These infections are generally unimicrobial. They may be treated with topical or systemic antibiotics, depending on the seriousness of the infection. Incision and drainage may be required for localized abscesses from these infections. Carbuncles and furuncles are circumscribed areas of inflammation of the skin and deeper tissues, with furuncles specifically beginning in a hair follicle or follicular gland. Staphylococcus is the in situ organism. Application of moist heat is recommended until the abscess points, allowing incision and drainage. Predisposing factors include diabetes or systemic conditions resulting in an underlying decreased immune response. Shaving across the delicate skin of the vulvar area, crural fold, or mons could also incite or spread such a process by breaking the skin, thus allowing access of staphylococci into the deeper tissue.
Hidradenitis Suppurativa
Hidradenitis suppurativa is a disease process that originates in the apocrine sweat glands, and is initiated by closure of the duct or pore, preventing normal expulsion of the gland contents. It is commonly a complex polymicrobial infection, having been colonized with bacteria from the skin, vaginal flora, and anorectal area. Abscessed glands may rupture at or below the skin surface, infecting the surrounding tissue and forming fistulae to other apocrine glands. Bhatia and associates1 recommended that the diagnosis be confirmed by biopsy. Simple incision and drainage is not effective. Antibiotic regimens providing activity against anaerobes and facultative anaerobes may produce some response. Antibiotic treatment, however, seldom provides a cure for this infection. Early disease may be cyclic, corresponding to the secretory activity of the apocrine glands during the progestational phase of the menstrual cycle. This activity may be modified with oral contraceptive pills. Remission has been achieved in 50% of patients treated with isotretinoin (Accutane).2 This medication should be used with caution, however, in women of reproductive age because it is a powerful teratogen. Strong consideration should therefore be given to early, aggressive, wide excision of the infected skin. A probe is inserted into the infected sinus and the tract unroofed to delineate the involved areas for excision. The excision should include a margin of noninfected tissue and the underlying subcutaneous tissue without fascia. The incision may be closed primarily or allowed to heal by secondary intention. If large areas are involved, a skin graft may be required. It is imperative that all infected tissue be removed to decrease the risk of recurrence.
Crohn's Disease
Crohn's disease should be in the differential for any vulvar inflammatory process with an associated draining tract. Biopsy of the affected tissue on the perineum will reveal the presence of noncaseating granulomas characteristic of Crohn's disease. Further bowel studies as well as a fistulogram may be employed to confirm the diagnosis. Excision of a draining sinus tract produced by Crohn's disease may result in further deterioration of the tissue. Therefore, the preferred treatment is prednisone and metronidazole for 4 to 6 weeks. Surgical excision or incision of the tract may be effective after appropriate medical management.
Necrotizing Fasciitis
The potential for necrotizing fasciitis of the vulva should be entertained in any patient who has not responded to initial therapy for inflammatory vulvar processes, and especially in patients with a decreased immune response, as is seen in diabetes. The infection extends down to the level of fascia, with biopsy of the fascia being diagnostic. The underlying fascial necrosis generally exceeds the boundaries of the visible skin infection. Broad-spectrum antibiotics and aggressive surgical excision are required for therapy.3 Debridement should be continued until viable, well-vascularized tissue margins are identified. Control of diabetes is necessary, if present. Hyperbaric oxygen therapy has been shown to improve tissue healing.
Viral Infections
Molluscum contagiosum is a member of the pox virus family and presents on the vulva as multiple, small, umbilicated lesions. The treatment of choice is evacuation of the umbilicated lesions, commonly with a dermal curette, followed by chemical cauterization of the base.
Condylomata acuminata is one of the manifestations of human papillomavirus (HPV) infections in the lower genital tract. Clinical infection is usually apparent in approximately 3 months, although the incubation period may range from several weeks to 8 months. More than 60 subtypes of HPV have been identified. HPV-6, -11, -16, -18, and -31 account for most genital tract infections. Histopathologic and virologic evaluation of vulvar lesions has demonstrated HPV-6 and -11 to be associated with the majority of exophytic condylomata. These two types are also common in flat cervical condylomata and low-grade cervical dysplasia. Reid and associates4 found HPV-16 and -18 to be commonly associated with high-grade dysplasia and invasive carcinomas. HPV-16 and -18 are infrequently identified in benign lesions. As condylomata acuminata identified on the vulva may be associated with cervical, vaginal, or perianal HPV infection, a careful clinical evaluation including cytology and colposcopy as indicated is appropriate in all patients who present with vulvar warts. This not only aids in defining the extent of condylomatous change, but also permits appropriate therapy to include any involved areas.
Condylomata acuminata generally present as small and usually multifocal lesions. The first line of therapy involves a local application of 25% podophyllin solution or 90% trichloroacetic acid. Podophyllin may be applied to the lesions without anesthesia in the office setting. A burning sensation occurs as the podophyllin is left on the lesion and gradually increases over time. The recommendation is to allow this solution to remain on the lesions for 4 to 6 hours after application, at which time it may be removed by bathing. Its use is restricted to nonpregnant patients and to the vulva. It should not be applied within the vagina because of increased absorption and potential neurotoxicity. Bichloroacetic or trichloroacetic acid has the advantage of being applicable for vaginal use as well as during pregnancy. It may produce a burning sensation initially, but this actually resolves over time and requires no rinsing solution. A disadvantage to both of these methods is that they commonly require multiple applications for adequate therapy.
Vulvar and perianal condylomata may become particularly massive secondary to lack of therapy, immunosuppression, and occasionally pregnancy. Surgical therapy is appropriate for extensive volume of disease, multicentric disease associated with intraepithelial neoplasia, and in immunocompromised hosts. Biopsy should be used liberally in condylomata that are refractory to topical treatment or have an atypical appearance. Laser ablation therapy has been shown to be very effective in removing bulk, multicentric, or resistant condylomata. Further biopsies may be obtained at the same time. Recurrence rates range from 25% to 50%. Close follow-up may allow early treatment of small recurrent lesions.
General anesthesia is generally preferred for laser ablation therapy. Lesions should be vaporized no deeper than the level of the surrounding skin surface, using only a depth of the first surgical plane as defined by Reid and co-workers.5 I generally employ a power of 20 W with a spot diameter of 1.5 to 2 mm, giving a power density of 500 to 800 W/cm2 for vaporization. Sites of vaporization are wiped with moistened gauze sponges to remove debris, cool the tissue, and permit accurate assessment of the depth of vaporization and the amount of remaining lesion. A brush technique is employed for the epithelium surrounding the lesions. The power is reduced to 10 W with a spot size of 2 mm to maintain a power density of 250 W/cm2. This superficially denudes the adjacent epidermis, as HPV has been demonstrated in the tissue proximal to the actual condyloma.6 Treatment of the subclinical infection is believed to prevent the reactivation of latent virus in the adjacent tissue, which may otherwise manifest as clinical infection after laser therapy.
Healing should be complete in 2 to 4 weeks. Local care includes sitz baths, followed by drying with the air setting of a blow dryer and application of silver sulfadiazine (Silvadene) cream. Narcotic analgesics are frequently required and are appropriate during the early healing process. Patients with known immunosuppression, particularly those with recalcitrant condyloma, may be treated after therapy or at the time of early recurrences with natural interferon alfa.7 This medication is not commonly used as initial therapy because of the requirement of regional injections 2 to 3 times per week with associative flu-like symptoms. Topical application of fluorouracil cream (Efudex) 5% has also been used to treat genital warts, but it is particularly caustic in the vulvar area and is generally limited to vaginal use.
Cryotherapy to the vulva has mostly been abandoned. Not only does it often require general anesthesia, but the depth of tissue destruction is difficult to assess, thereby making it less popular than more precise methods outlined above. Electrocautery with a loop has been found to be effective particularly with extensive lesions, but again general anesthesia is generally required, and the depth of penetration is not as precise as with laser therapy. However, this method can be combined with laser therapy: larger lesions can be removed superficially with the loop, leaving the resultant base of the lesion amenable to laser therapy.
DERMATOLOGIC CONDITIONS
Dermatologic conditions of the vulva are responsible for a large number of gynecologic office visits. The vulvar skin is a frequent site of contact dermatitis produced by both primary irritants and allergic phenomena. The vulvar area may be irritated by local cosmetic or therapeutic agents, as well as by biological fluids such as urine or feces in cases of incontinence or difficult hygiene. Generalized skin conditions such as psoriasis, seborrheic dermatitis, and lichen planus may also have manifestations in the vulva and may be confused with other etiologies, such as candidiasis. These skin conditions may have a slightly different appearance on the vulva than in other areas of the body because of the moisture present. Steroid preparations are commonly used for these dermatologic conditions. In contact dermatitis the offending substance, if identified, is removed. Biopsy is recommended in any of these circumstances if the course is chronic or the precise etiology unclear.
Biopsy of the vulvar skin is usually obtained with a Keyes biopsy punch. A simple alcohol preparation is sufficient with infiltration of local anesthetic, usually 1% lidocaine injected subepidermally with a 25-gauge needle. The addition of epinephrine promotes vasoconstriction and prolongs the anesthetic effect. The Keyes punch is available in diameters ranging from 2 to 5 mm, with 4- and 5-mm diameters most commonly employed for vulvar use. The site selected for biopsy should include tissue representative of the lesion or area of abnormality, but not necessarily the most central inflamed or necrotic area, which may give minimal tissue diagnosis because of the inflammation present. Therefore, the site picked is often at the periphery and may even include an edge of the lesion as it approaches the normal tissue. The cutting edge of the punch is applied to the surface (Fig. 1). With light pressure, the punch is rotated clockwise and counter clockwise, essentially drilling a hole through the full thickness of the skin. The specimen is then elevated with forceps and removed sharply from the underlying subcutaneous tissue. Hemostasis may be controlled with application of a silver nitrate stick to the site. Direct pressure may also be employed. Occasionally a suture of 3.0 chromic is required.
|
Intractable Pruritus
Some patients with benign dermatologic conditions have chronic pruritus that is not amenable to topical agents. This may be due to the inability of these drugs to penetrate the thickened, hyperkeratotic surface of the skin. In these instances a steroid injection into the subepithelial dermis may be appropriate. An injection of 20 to 30 mg (10 mg/mL) of triamcinolone acetonide (Kenalog) to a localized area is effective. The injected solution should be rubbed thoroughly into the tissue. Relief of symptoms may occur within 48 hours. Remissions may last for 4 to 6 months. Injections can be repeated for recurrent symptoms.
Local alcohol injections have also been employed, but require a general anesthetic. The entire vulvar area is marked off in a grid of 1-cm squares (Fig. 2). Absolute ethyl alcohol, 0.1 to 0.2 mL, is then injected into the subcutaneous tissue with a 25-gauge needle at each intersection of the lines, beginning at the lowest level of the grid.8 Care must be taken to avoid injection into the epithelium or into the deep subcutaneous tissue to avoid tissue necrosis and sloughing. Thin folds of the labia minora should be injected only at the bases. All areas should be fully massaged to facilitate even distribution. Localized edema is noted rapidly and is present for 2 to 3 weeks. Recurrent symptoms may require additional treatment. Most patients get at least enough relief so that their symptoms may be controlled with topical agents.
The Mering procedure may be employed if all other measures have failed to produce relief of symptoms.9 It involves blunt dissection through the subcutaneous tissue of the vulva to interrupt the branches of the ilioinguinal and genitofemoral nerves. The procedure requires a general or regional anesthetic. Incisions are made at the lateral margins of the labia majora, extending to the level of the clitoris superiorly and the anal orifice inferiorly (Fig. 3). The dissection is continued to the level of the fascia. The nerves in the adjacent tissue are disrupted bluntly, allowing the fingers in each incision to meet in the midline above and below the clitoris; blunt dissection proceeds posteriorly to meet in the perineum, and even around the rectum if symptoms are present in this area. This perianal disruption will also affect branches of the pudendal nerve. Hematoma formation and cellulitis are potential complications. A small drain is therefore placed in the most dependent portion of the incision. Both the underlying tissue and the skin edges are closed with absorbable suture. It is recommended that this area be treated with direct pressure for 24 hours, followed by ice packs.
Vulvar Vestibulitis
Vulvar vestibulitis is the most prevalent of the vulvar pain syndromes, or vulvodynia. It is a chronic condition for which no single etiology has been identified. It is characterized by inflammation localized to the vulvar vestibule, with dyspareunia as the most common complaint. The technique described for diagnosis includes probing the vestibule with a cotton-tipped applicator to map the area of burning and pain, which is often exquisite, thus mimicking the patient's symptoms. The area involved is nonkeratinized squamous epithelium containing mucous-secreting minor vestibular glands. These glands supply lubrication for coitus and may become inflamed due to edema, trauma, or infection. The examination reveals areas of bright erythema consistent with focal inflammation. Biopsy often shows a chronic inflammatory infiltrate with plasma cells. HPV has been demonstrated in some lesions by DNA hybridization techniques.10
Therapy has been directed toward treating any underlying infectious or dermatologic etiologies that may be aggravating these symptoms, as well as toward the use of topical anesthetic solutions or gels applied to the affected areas before coitus. Other therapies that have been reported as having some success in small series include acyclovir given over a 3-month period,11 intradermal injection of interferon alfa three times per week for 4 weeks,12 and low-dose 5-fluorouracil.13 Laser ablation has been successful in some cases.14 Surgical excision is considered for women whose symptoms have persisted for more than 6 months despite use of the therapies already mentioned. With vulvar vestibulectomy, 60% to 80% of women report significant pain relief. In performing the vestibulectomy with perineoplasty, the specific area of pain should be carefully delineated with a marking pen immediately before the administration of any anesthetic. The full epithelial thickness should be excised with inclusion of the adjacent hymen (Fig. 4). The posterior vaginal wall should be separated from the underlying tissue for 2 to 3 cm above the hymenal ring so that it may be pulled down and out to close the defect created. This vaginal mucosa is attached to the perineum with a mattress closure of interrupted absorbable suture.
CYSTS OF THE VULVA
Bartholin's Duct Cyst
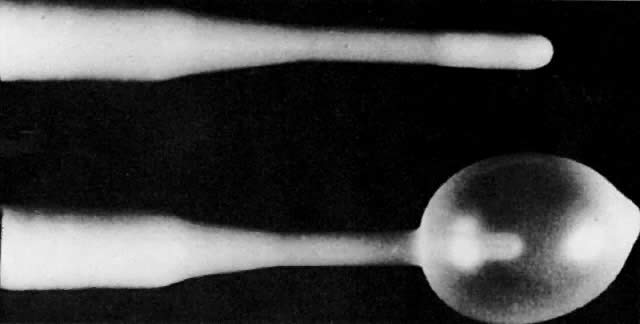
The most common large cyst of the vulva is a cystic dilation that results from an obstructed Bartholin's duct. The underlying gland continues to produce secretions. In asymptomatic women less than 40 years of age, no treatment may be required. To exclude malignancy in women above the age of 40, excision of the cyst and the underlying gland is recommended. Adenocarcinoma may be found in the gland, as well as transitional or squamous cell carcinoma in the duct. A Bartholin's abscess may present acutely with localized tenderness and surrounding induration or erythema. Incision and drainage is recommended with immediate improvement of symptoms. This may be performed with a local anesthetic. A small stab wound is made through the vestibular mucosa as close as possible to the hymeneal ring and into the cyst or abscess in an area that appears closest to the mucosal surface. Internal loculations should be disrupted with a straight hemostat, and the extent of the cyst explored. After exploration, the cavity should be rinsed thoroughly. At this point it is necessary to place a wick with packing into the gland, or preferably a Word catheter.15 This catheter is similar to a small pediatric catheter with an inflatable balloon to maintain its position within the cavity (Fig. 5). Normal saline should be used to inflate the bulb, as an air inflation may result in premature deflation. The end of the catheter can be tucked within the vagina for comfort. This catheter should remain in place for 3 to 4 weeks to ensure reepithelialization, thereby creating a new duct opening. Without this epithelialized tract, secretions due to the underlying functional gland tissue can reaccumulate, resulting in an unacceptably high recurrence rate. Bacteria present within Bartholin's abscess include normal vaginal flora, Escherichia coli, and occasionally Chlamydia and Neisseria. Appropriate cultures should be obtained. Women should be placed on metronidazole and penicillin for the next 7 days if there is any evidence of surrounding cellulitis. Diabetic women should return within 24 hours for reevaluation to ensure that they are responding adequately.
A recurrent or symptomatic but uninfected Bartholin's duct cyst may be addressed with surgical marsupialization. This technique is preferred to direct excision for recurrent cysts to maintain the functioning gland and to avoid the somewhat extensive dissection in this highly vascular area, which can result in scarring and vulvar pain. Surgical marsupialization involves directly approximating the ductal epithelium of the cyst or abscess to the overlying introital epithelium. Local infiltration of an anesthetic or a unilateral pudendal block are appropriate options for this procedure. Rarely is a general anesthetic necessary. A vertical ellipse of vestibular epithelium is excised from the center of the cyst, just outside the hymeneal ring (Fig. 6). The excision should be as wide as possible because the stoma will become smaller as it heals. The cyst wall is opened and the internal contents are drained and rinsed, as previously described. The lining of the cyst is everted and sutured directly to the vestibular mucosa with interrupted sutures of 2.0 delayed absorbable material. Antibiotics are not generally required. For patient comfort and healing, warm sitz baths twice daily are recommended for the week after surgery. The risk of recurrence after marsupialization is 10% to 15%.
Excision of a Bartholin's duct cyst is reserved for cases that have persistently recurred despite other measures, or for cases involving women older than 40 in whom a rare carcinoma may be detected. An elliptical incision is made in the vestibular mucosa adjacent to the hymenal ring immediately overlying the cyst (Fig. 7). Excising a small elliptical portion of the mucosa allows adequate exposure. The mucosal edges may be grasped with Allis forceps for traction. Blunt dissection may be possible; however, cyst formation is often preceded by inflammation, which causes adherence of the wall to the surrounding tissue. Tenotomy scissors are excellent for sharp dissection. A small gauze or the handle of the scalpel is used for blunt dissection. It is not unusual for the cyst to be larger and deeper within the tissue than originally suspected. If the cyst approaches the rectum, a finger inserted into the rectum during this dissection may help in distinguishing the cyst boundaries. The base of the cyst is a common place to encounter bleeding because of the venous channels of the vestibular bulb and underlying glandular tissue. Dissection across this area may be best handled with small Burlisher clamps with pedicles that are cut and tied individually for complete removal of the duct and gland if possible. The entire cavity is then obliterated with a small delayed absorbable suture material. Any direct areas of bleeding should be addressed, as a hematoma in this area may be particularly painful, can dissect into adjacent tissues, and potentially become infected. The vestibular mucosa is approximated with a continuous suture of 2.0 delayed absorbable material. If a hematoma of the labia develops after surgery, bed rest with ice packs and a pressure dressing is recommended, as reexploration of the surgical site often leads to no visible single source of bleeding. Although the blood will reabsorb with time, the hematoma may also liquefy in 4 to 5 days, allowing adequate drainage and evacuation.
|
Hydrocele (Canal Of Nuck)
A hydrocele represents the dilatation of the peritoneum that accompanies the round ligament and extends from the inguinal canal into the vulva. It usually presents in the labia majora adjacent to the labia minora. It may be confused with a Bartholin's duct cyst. Dilatation in the inguinal canal is known as a cyst of the canal of Nuck. In rare instances a loop of intestine is found to follow this pathway to the vulva. Surgical therapy involves incision of the skin to expose the hernia sac, which is then opened and dissected free. After complete excision of the peritoneal lining, the external inguinal ring is closed along with the adjacent subcutaneous tissue.
Paraurethral And Skene's Glands
Paraurethral and Skene's glands may present with cystic dilatation immediately adjacent to the urethra. These cysts are most commonly lateral or posterolateral in location. A direct connection to the urethra may be identified with urethroscopy or with direct palpation producing a urethral discharge. It is not recommended that these cysts be primarily incised and drained, because such drainage may produce a fistulous tract from the urethra to the vestibule or perineum. Treatment of symptomatic cystic areas consists of incising the mucosa immediately over the cystic structure, but directed away from the urethral meatus. A Foley catheter may be inserted into the urethra to identify its location throughout the dissection. The cystic structure is then dissected, generally with a combination of blunt and sharp dissection, with careful attention to the dissection along the side that borders the urethra. Hemostasis should be meticulous, and the defect thus created closed with interrupted 3.0 absorbable suture. Retention of the Foley in the urethra throughout the closure ensures that the urethral mucosa is not incorporated into this closure. The overlying epithelium is then reapproximated with continuous 2.0 absorbable suture. The Foley catheter may be removed at this point. Spontaneous voiding is generally resumed immediately.
Distal Diverticulum
A distal diverticulum may be encountered in the midline immediately beneath the urethral meatus and present as a cystic structure at the introitus. Its tract into the urethra may be identified with urethroscopy, transvaginal sonography, voiding cystourethrography, or double balloon urethrography. Lee stated that 15% occurred in this distal location.16 The dissection at this point may be approached by the classic method of opening the anterior vaginal wall, mobilization of the underlying pubocervical fascia, and meticulous sharp dissection of the diverticular sac with transection across the neck of the diverticulum. At this point, the urethra is closed in a linear fashion over a urethral catheter with interrupted 4.0 delayed absorbable suture. The pubocervical fascia is then closed in a pants-over-vests fashion with 3.0 delayed absorbable suture followed by closure of the vaginal wall with 3.0 delayed absorbable suture. Hemostasis is meticulously maintained throughout this procedure. The urethral catheter is usually maintained for approximately 5 to 7 postoperative days. This discussion presents the basic components of the surgical technique used for a distal diverticulum, but does not address multiple tract openings or diverticula in the middle or upper third of the urethra, which require further attention to support the urethrovesical junction.
In contrast to this classic dissection and closure, another alternative that is applicable to patients with a distal diverticulum is that reported by Spence and Duckett.17 This procedure involves placing one blade of the scissors in the urethra and the other blade in the vagina at or under the diverticular sac to essentially create a common opening for the urethra which includes the sac epithelium. Hemostasis is maintained on the right and left lateral margins thus exposed with 3.0 or 4.0 delayed absorbable suture. This procedure may afford some benefits when a diverticulum is extremely distal and when a short surgical procedure is believed to be advantageous. It should be noted, however, that this may shorten the functional component of the urethra and could be a risk factor for incontinence.
ABNORMALITIES OF THE URETHRA
Urethral Caruncle
A urethral caruncle is a small, fleshly outgrowth usually at the posterior surface of the urethra. It is generally soft, smooth, and bright red, and may be somewhat friable. It is most common in postmenopausal women and its differential diagnosis includes primary carcinoma of the urethra and prolapse of the urethral mucosa. In a series of 394 women with urethral tumors reported by Marshall and colleagues,18 the diagnosis of urethral caruncle was made in 376 of the women and urethral carcinoma in 9 women. The diagnosis is established by biopsy under local anesthesia. Small, asymptomatic caruncles may not require treatment. Initial therapy is oral or topical estrogen and avoidance of any associated irritation. For large or symptomatic caruncles that do not respond to these conservative measures, further options include laser therapy, fulguration, or operative excision. A Foley catheter is generally required for 48 to 72 hours after a destructive or surgical procedure.
Prolapse Of The Urethra
Prolapse of the urethra is a condition that may exist in premenopausal and postmenopausal women. It may require no treatment if asymptomatic. Therapy of a prolapsed urethra includes hot sitz baths and antibiotics to reduce inflammation and infection. In rare cases, it may be necessary to excise the redundant mucosa. The surgical procedure in cases where this is felt to be pertinent involves excising the redundant circular mucosal tissue with reapproximation of the urethral edge to the circumferential vulvar skin using a series of 3.0 interrupted suture (Fig. 8).
CONDITIONS OBSTRUCTING THE INTROITUS
Surgery Of The Hymen
In cases of imperforate hymen, a small pin-size hole is often identifiable, which allows probing to ensure the presence of the underlying vagina. In these cases, a cruciate incision may be made and the hymen excised in quadrants (Fig. 9). The circumferential vaginal edge thus produced is sutured to the vestibule with interrupted sutures. A hymenotomy may also be performed in cases where the vaginal opening is clearly visible, but functionally obstructed secondary to the presence and rigidity of the hymen. Incisions at 4 and 8 o'clock allow increased vaginal diameter. The patient must maintain this opening during the healing phase.
Nichols also describes patients with recurrent postcoital cystitis who may have thickened lateral bands connecting the urethral meatus to the hymenal margin.19 In this case, urethrolysis can be curative. The procedure involves a crush injury with forceps at the site of hymenal attachment to the urethra, which is at approximately 11 and 1 o'clock on the hymenal ring (Fig. 10). An incision is made through the crush material. A running locked suture is then placed along the cut edge of the incision, allowing a flap release of the urethra from this hymenal ring tension.
Labial Agglutination
Labial agglutination is seen in prepubertal females who have had a localized infection or inflammation, resulting in subsequent adherence of the labial tissues. Initial therapy is directed at improving the local environment and reducing the inflammation or infection, followed by topical estrogen therapy. Most cases will respond adequately to these measures. Separation will often occur spontaneously at menarche. Therefore surgical separation should be delayed if possible. Because of the potential traumatic impact, both physical and mental, of manual separation of the labia in the office, general anesthesia is recommended in cases where surgical therapy is considered. These cases are most commonly related to difficulty with urination. With the patient under general anesthesia and the area adequately exposed, a very thin white line of agglutination can be seen. This line can easily be separated with a combination of blunt and sharp dissection. Hemostasis is rarely a factor and may simply be controlled with cautery and occasionally a small suture. It is imperative that during the postoperative healing phase these tissues remain separated to prevent recurrence. Silvadene cream to the perineum, along with topical estrogen in limited amounts, is helpful for this purpose.
Introital Stenosis
A stenotic introitus may at times be treated with vaginal dilators and the addition of estrogen in postmenopausal women. Surgical therapy may be employed to increase the caliber of the introitus and to release submucosal fibrotic tissue. A midline incision may be made in the perineal body skin and extended just past the hymenal ring (Fig. 11). The underlying fibrosis is incised. The perineal epithelium and vaginal mucosa are undermined to produce mobility of the tissue. The incision is then closed transversely using interrupted mattress sutures.
In cases where a simple perineotomy is not effective, a Z-plasty may be curative, as described by Nichols and Randall.20 A Z-shaped incision is made right posterolaterally and left posterolaterally just at the introitus (Fig. 12). The full-thickness flaps are undermined, rotated and sewn into place.
SOLID TUMORS OF THE VULVAR
Fibromas
Fibromas are the most common benign solid tumor of the vulva and are of mesenchymal origin. The most common location on the vulva is in the labia majora. Treatment is by excision for symptoms or for continued growth.
Lipoma
Lipomas are slow-growing tumors of fat cell origin. As with fibromas, they frequently occur within the labia majora. Although small tumors may be monitored expectantly, larger or faster-growing tumors are usually removed for diagnosis.
Hidradenoma
A hidradenoma is a rare, benign, usually small vulvar tumor that originates from apocrine sweat glands. The location is generally the inner surface of the labia majora and the perineum. Hidradenomas may be cystic or solid. Excisional biopsy is the treatment of choice.
Excision of tumors within the subcutaneous or fibrous tissue of the vulva are usually addressed with an incision line that matches the contour of the labia or the introitus (Fig. 13). A Foley catheter placed in the urethra is particularly beneficial if there is any displacement of the urethra or urethral meatus. If the size of the mass has produced an apparent redundancy of the overlying skin, an elliptical incision with partial removal of this excess skin is advantageous. The skin edges are then grasped with Allis forceps. The underlying mass is identified and removed with sharp dissection. During the dissection an area with the tumor's blood supply may be best approached with a Burlisher, followed by transection and individual ligation with 3.0 absorbable suture. The subcutaneous tissue is closed with 3.0 absorbable suture, and the skin edges are closed with interrupted 2.0 absorbable sutures.
VASCULAR ABNORMALITIES
Varices
Varices are common on the vulva and are related to the pudendal veins. They can involve tributaries of the hypogastric vein with varicosities extending through the gluteal vessels over the buttocks. Treatment depends on size as well as symptoms, particularly discomfort after exercise or long periods of standing due to engorgement. In these occasions ligation with excision of the segment of vulvar skin that contains the varices is a treatment option.
Hemangioma
Hemangiomas are malformations of blood vessels and may occur on the vulva. Strawberry hemangiomas are congenital defects discovered in young children. Most vulvar hemangiomas discovered in neonates and children remain stable or regress in size. Cherry angiomas normally arise on the labia majora of postmenopausal women. They are often less than 3 mm in diameter, multiple, and red-brown to dark blue. Angiokeratomas are approximately twice the size of cherry angiomas. They may demonstrate rapid growth and a tendency to bleed with strenuous exercise. Their color is blue to purple, and the differential diagnosis includes Kaposi's sarcoma and angiosarcoma. Pyogenic granulomas represent an overgrowth of inflamed granulation tissue. The differential diagnosis includes malignant melanoma, basal cell carcinoma, vulvar condyloma, or nevus. Congenital hemangiomas rarely require treatment, whereas a biopsy specimen should be taken in an adult with an abrupt appearance of a pigmented lesion. Excisional biopsy may be diagnostic and therapeutic with smaller lesions. Large lesions may be difficult to remove. In these cases ligation of larger vessels may be beneficial if persistent bleeding is a problem.
TRAUMA
Hematomas
The vulva is richly supplied with vascular anastomotic channels, which make treatment of hemorrhage with compression or ligation of a single major vessel limited. Hematomas may result from sharp or blunt injury to the vulva. Most hematomas in women result from straddle injuries. A vulvar wound may be the only indication of deeper trauma, including vaginal injury, urethral compromise, and even pelvic fracture. Vulvar trauma in children or adults should be a marker to explore any evidence of potential abuse.
The management of vulvar hematomas is usually initiated with ice packs and pressure. The bleeding is usually venous in origin and therefore generally self-limiting. If the skin has not been violated and the hematoma is self-contained, it will gradually resorb with time. Any puncture wound or laceration at the time of the injury may introduce bacteria into the hematoma. In these cases broad-spectrum antibiotics should be initiated along with close observation for further evidence of infection, which will require incision and drainage. If drainage is necessary, it may be best accomplished after 4 to 5 days, as the hematoma liquefies. In cases of rapidly expanding hematomas, incision and drainage may also be necessary, with ligation of any active bleeding sites identified. Packing may be used temporarily to aid with compression, although it should be removed as quickly as believed prudent to decrease the risk of infection. Hematoma formation in children may require a general anesthetic for an adequate examination, which includes examination of the vagina, placement of a urethral catheter, and in some instances laparoscopy to ensure there has been no penetration into the peritoneal cavity.
Laceration
Lacerations of the vulva, which may also extend into the vagina as a result of trauma, should be evaluated thoroughly and may require a general anesthetic for complete delineation of the severity of the injury. Necrotic and damaged tissue should be removed. The areas involved should be copiously irrigated. Antibiotic therapy should be initiated to cover flora of the skin, vagina, and rectum, as well as any sexually transmitted diseases if indicated. If healthy tissue is demonstrated during the operative procedure, the areas of laceration may be closed primarily.
VULVAR LESIONS
Vulvar lesions may present in numerous forms. They may present as pigmented areas; depigmented areas; white, thickened, or grayish areas; reddened areas; atrophic or thinned areas; and grossly ulcerated or polypoid. Although certain characteristics exist for specific disease processes, biopsy is used for a definitive diagnosis. Less dramatic appearing areas in the vulva that remain symptomatic despite previously employed therapies should also raise the suspicion of an unidentified lesion and should prompt a biopsy. The Keyes punch biopsy (see previous discussion) is an excellent choice for obtaining a portion of tissue in an area that is diffuse, large, multicentric, or believed to be probably benign in origin. An excisional biopsy is often useful in situations where the lesion is small or where both diagnosis and therapy may be accomplished.
Excisional Biopsy
Excisional biopsy is generally employed for circumscribed lesions when complete removal is desired. The incision should be made with a no. 15 blade at a right angle to the skin's surface. An elliptical incision is ideal, if possible, because this shape makes it generally easier to close the adjacent edges. A shallow wedge of subcutaneous tissue below the lesion should be included in the incision. The long axis of the incision should match the structure on which it is located on the vulva. Thus, incisions on the labia or lateral labial area should be parallel to the labial axis. Incisions at the introitus should match the curvature of the introitus, and incisions on the perineal body may be best performed with the long axis of the incision somewhat horizontal. These efforts will generally reduce the tension on the incision line. The vulvar skin is prepared with povidone-iodine and alcohol. The site is infiltrated with 1% lidocaine with epinephrine (Fig. 14). A 5- to 10-mm border of surrounding normal tissue is recommended for most lesions. The defect is closed with interrupted 3.0 delayed absorbable suture with direct reapproximation of the skin edges. A larger excisional biopsy may require a regional or general anesthetic. In these cases edema may be reduced with an ice pack during the first 24 hours, followed by daily warm sitz baths.
|
For treatment of a unifocal area of carcinoma in situ, Paget's disease, or small superficial melanomas, a wide local excision carried down to Colles' fascia is appropriate in order to achieve primary closure without tension. The defect may be slightly longer, wider, or a different shape than would be considered necessary for diagnosis alone. The goal should be to decrease tension as well as avoid unwanted folds and puckering. Deep layers of suture will not only assist with hemostasis but will relieve tension at the skin layer. A 3.0 delayed absorbable suture is ideal for closure.
Nevi And Melanomas
Vulvar nevi are common and generally asymptomatic. Because women do not tend to inspect this area closely, they are unaware of changes in the appearance of these lesions. Therefore, ideally vulvar nevi should be excised. This excision may be accomplished with local anesthesia. The obstetrician and gynecologist also has an excellent opportunity to inspect the vulva and remove any nevi at the time of an obstetric delivery or gynecologic surgery.
The vulvar area represents 1% of the skin surface of the body. In contrast, 5% to 10% of all malignant melanomas in women arise from this region. Approximately 30% of malignant melanomas arise from a preexisting nevus.21 The clinical features of an early malignant melanoma have been listed by Friedman and associates.22 These include asymmetry, border irregularity, color variegation, and a diameter usually greater than 6 mm. Melanomas with level I or II involvement have an excellent prognosis and demonstrate the principle that early removal of superficial lesions is the key to improved outcome.
Vulvar Dystrophy
Vulvar dystrophies represent a number of disorders of the epithelium that involve abnormalities of growth and maturation resulting in a white-appearing surface. Dystrophies include lichen sclerosus and hyperplasia with or without atypia. Although cases with atypia may have some premalignant potential, the majority of cases of chronic epithelial dystrophy show no increased risk of malignant change.
Lichen sclerosus may occur in any age group and symptomatically is characterized by intense pruritus. Extensive excoriation may be visualized. The vulvar architecture is progressively destroyed, with adhesions, agglutination, edema, and scarring. The surface epithelium is generally pale, with a shiny and crinkled appearance and varying degrees of hyperkeratosis. Biopsy reveals thinning of the epidermis, loss of rete peg architecture, an underlying acellular homogenous dermis, and deep chronic inflammatory cells. Biopsy is therefore recommended for definitive diagnosis. Treatment is topical testosterone propionate 2% in petrolatum. Lifetime maintenance therapy is generally required, with application once or twice a week even after adequate therapy has returned the vulva to a normal appearance. Some patients will also require a combination of 7 parts betamethasone valerate (Valisone) and 3 parts crotamiton (Eurax) applied intermittently for relief of pruritus. If this therapy is continued, alternating with testosterone, a dominant testosterone effect will be seen over a longer period of time.
Women with hyperplasia of the vulva generally present with thickened white vulvar epithelium with pruritus as their primary symptom. Histologic evaluation reveals a thickened epithelium, elongated rete pegs, and inflammatory cells in the underlying dermis. Cellular atypia may be present, as demonstrated by abnormal maturation in the acanthotic epithelium. In atypia, mature abnormally keratinized cells may be seen in the basal layer of the epithelium. Diagnosis is obtained with a biopsy. A combination of 7 parts betamethasone valerate and 3 parts crotamiton applied twice daily is the recommended therapy. Once the condition has completely regressed, recurrence is less common. Therefore, development of new areas should promote rebiopsy.
Some women will present with mixed dystrophy, that is, both lichen sclerosus and hyperplastic changes. When both lesions are present, corticosteroids are usually given as the initial treatment. Testosterone therapy is instituted once the hyperplastic areas have receded. Corticosteroids and testosterone preparations may also be used on alternate days and may be equally effective, but slower in producing resolution.
Paget's Disease
Paget's disease of the vulva is a lesion of apocrine origin with primary presenting symptoms of itching and burning. The lesions are usually velvet red with dotted white epithelial islands that are grossly suggestive of carcinoma in situ. Histologically the vulvar Paget cell is large, containing abundant almost-clear cytoplasm and a pale nucleus with a prominent nucleolus. This cell appears in the basal level of the epithelium, the basal cell layer being otherwise intact. One fourth to one third of patients with extramammary Paget's disease of the vulva have invasive adenocarcinoma of the underlying apocrine gland structures. Therefore, if this diagnosis is made on the basis of a biopsy, referral should be made to a surgeon who will be prepared to perform a wide subtotal or total vulvectomy with frozen sections of the margins to guide excision intraoperatively. A skinning vulvectomy is not recommended in Paget's disease, as these underlying areas of apocrine glands would not be adequately addressed. Local recurrences may be seen despite histologically clear margins.23
Carcinoma In Situ
Carcinoma in situ may present with a symptom of pruritus, bleeding, pain, or a lump on the vulva. Lesions may be focally red or white and are often raised or ulcerated. Because lesions can mimic many of the other vulvar abnormalities previously described, a biopsy is imperative. A biopsy with a Keyes punch may be performed in the office setting under local anesthesia. Multifocal areas of neoplasia are common. Treatment options include wide local excision for unifocal areas, vulvectomy for larger or multifocal areas, and carbon dioxide laser therapy. CO2 laser therapy may be particularly useful in areas where excision would hamper preservation of the anatomy, such as in the clitoral area. It should be employed, however, with liberal use of biopsies to exclude an occult invasion. Laser treatment of vulvar carcinoma in situ must also address extension of disease into hair follicles and therefore mandates deeper laser vaporization beyond the papillary dermis and into the upper reticular dermis or the third surgical plane. Baggish and co-workers24 identified skin appendage involvement in 36% of cases of vulvar carcinoma in situ, predicting that laser vaporization to a depth of 2.5 mm would effectively treat 95% of involved appendages. Power densities of greater than 750 W/cm2 are recommended to decrease thermal injury of underlying tissue produced with lower powered densities, thus decreasing the risk of scarring.
REFERENCES
Bhatia NN, Bergman A, Broen EM: Advanced hidradenitis suppurativa of the vulva. J Reprod Med 29: 436, 1984 |
|
Dicken CH, Powell ST, Spear K: Evaluation of isotretinoin treatment of hidradenitis suppurativa. J Am Acad Dermatol 11: 500, 1984 |
|
Stephenson H, Dotter DJ, Katz V, Droegemueller W: Necrotizing fasciitis of the vulva. Am J Obstet Gynecol 166: 1324, 1992 |
|
Reid R, Greenberg M, Jenson AB et al: Sexually transmitted papillomaviral infections: I. The anatomic distribution and pathologic grade of neoplastic lesions associated with different viral types. Am J Obstet Gynecol 156: 212, 1987 |
|
Reid R, Elfone EA, Zirkin RM, Fuller TA: Superficial laser vulvectomy: II. The anatomic and biophysical principles permitting accurate control over the depth of dermal destruction with the carbon dioxide laser. Am J Obstet Gynecol 156: 261, 1985 |
|
Ferenczy A, Mitao M, Nagai N et al: Latent papillomavirus and recurring genital warts. N Engl J Med 313: 784, 1985 |
|
Reid R: Superficial laser vulvectomy III. Am J Obstet Gynecol 166: 815, 1992 |
|
Woodruff JO, Babaknia A: Local alcohol injection of the vulva: Discussion of 35 cases. Obstet Gynecol 54: 512, 1979 |
|
Mering JH: A surgical approach to intractable pruritus vulvae. Am J Obstet Gynecol 64: 619, 1952 |
|
Turner ML, Marinoff SC: Association of human papillomavirus with vulvodynia and the vulvar vestibulitis syndrome. J Reprod Med 33: 533, 1988 |
|
Friedrich EG Jr: Therapeutic studies on vulvar vestibulitis. J Reprod Med 33: 514, 1988 |
|
Horowitz BJ: Interferon therapy for condylomatous vulvitis, Part I. Obstet Gynecol 73: 446, 1989 |
|
Reid R, Greenberg MD, Daoud Y et al: Colposcopic findings in women with vulvar pain syndromes: A preliminary report. J Reprod Med 33: 523, 1988 |
|
Oates JK: Focal vulvitis and localized dyspareunia. Genitourin Med 66: 28, 1990 |
|
Word B: Office treatment of cyst and abscess of Bartholin's gland duct. South Med J 61: 514, 1968 |
|
Lee RA: The repair of urethral injuries, diverticula, and fistula. In Nichols DA (ed): Gynecologic and Obstetric Surgery, p 829. St. Louis, Mosby-Year Book, 1993 |
|
Spence HM, Duckett JW Jr: Diverticulum of the female urethra: Clinical aspects and presentation of a simple operative technique for cure. J Urol 104: 432, 1970 |
|
Marshall FC, Uson AC, Melicow MM: Neoplasms and caruncles of the female urethra. Surg Gynecol Obstet 110: 723, 1960 |
|
Nichols DH: Gynecologic and Obstetric Surgery. St. Louis, Mosby-Year Book, 1993 |
|
Nichols DH, Randall CL: Vaginal Surgery, 3rd ed. Baltimore, Williams & Wilkins, 1989 |
|
Silvers DN, Halperin AJ: Cutaneous and vulvar melanoma: An update. Clin Obstet Gynecol 21: 1117, 1978 |
|
Friedman RJ, Rigel DS, Kopf AW: Early detection of malignant melanoma: The role of physician examination and self-examination of the skin. CA 35: 1130, 1985 |
|
Nichols DH: Gynecologic and Obstetric Surgery, p 289. St. Louis, Mosby-Year Book, 1993 |
|
Baggish MS, Sze EH, Adelxon MD et al: Quantitative evaluation of the skin and accessory appendages in vulvar carcinoma in situ. Obstet Gynecol 74: 169, 1989 |