Treatment of Cervical Intraepithelial Neoplasia
Authors
INTRODUCTION
Cervical cancer screening programs have been effective in reducing the deaths from cervical cancer in screened populations.1 Despite the development and continued improvement of the Pap smear and other screening tools such as human papillomavirus (HPV) testing, the dream of detecting precursor lesions and eliminating all cancer death has not been realized and cervix cancer remains a significant women's health problem worldwide. In countries such as the United States where screening programs are widely available, 12,200 new cases of invasive disease are diagnosed annually and these cases are responsible for 4100 deaths each year.2 Continuing efforts to improve the diagnostic accuracy and treatment methods for preinvasive cervical disease are necessary. Unfortunately, changing terminology and management strategies can often be confusing to the practitioner performing cervical cancer screening. Screening strategies and the evaluation of the abnormal Pap smear result for the detection of cervical intraepithelial neoplasia are discussed elsewhere in this library. This chapter focuses on the treatment and posttreatment surveillance of preinvasive lesions of the cervix, with emphasis on choosing the strategy that best fits the clinical scenario.
DEFINITIONS
Cervical intraepithelial neoplasia (CIN) is a biological spectrum of disease that antedates invasive squamous cell carcinoma.3, 4 The histopathologic diagnosis requires the recognition of a disordered pattern of squamous cell maturation and nuclear atypia. The density of cells is increased and the normal cytoplasmic glycogen is diminished. The spectrum of disease is characterized by mild (CIN I), moderate (CIN II), and severe (CIN III) dysplastic changes.
HPV lesions are perhaps the earliest form of cervical intraepithelial neoplasia and are often indistinguishable from mild dysplasia. Mild dysplasia is characterized by pathologic changes confined to the lower-third of the epithelium. The lesion of moderate dysplasia involves the lower two-thirds of the epithelium. The pathologic changes associated with severe dysplasia and carcinoma in situ (CIS) occupy the full thickness of the epithelium. Carcinoma in situ and severe dysplasia are biologically and histologically indistinguishable.3
The introduction of the CIN classification in the 1960s by Richart was an attempt to clarify that severe dysplasia and carcinoma in situ were one disease process. Similarly, it is now suspected that changes associated with HPV and those of mild dysplasia are biologically and histopathologically indistinguishable.5 The Bethesda System, originally conceived in 1988 and subsequently modified in 1991 and 2001,6 takes this into account by grouping HPV and CIN I together as low-grade squamous intraepithelial lesion (LSIL), and CIN II and CIN III/CIS together as high-grade squamous intraepithelial lesion (HSIL) by Pap smear. The natural history and morphologic features of these lesions are similar and there is significant overlap.7 In addition, there is a lack of interobserver and intraobserver reproducibility among reporting grades of dysplasia and particularly between reporting of HPV changes and CIN I.8, 9 For practical treatment planning, preinvasive cervical lesions are best divided into two subgroups: low-grade cervical intraepithelial neoplasia (HPV and CIN I) and high-grade cervical intraepithelial neoplasia (CIN II–III/CIS).
DIAGNOSIS OF DYSPLASIA
The most important goal of colposcopy in the evaluation of an abnormal Pap smear result is to rule out invasive carcinoma. Once cancer has been excluded, the focus of the evaluation turns to defining the severity and extent of any preinvasive lesions on the cervix. Key features in the success of a colposcopic evaluation of the cervix include appropriate instruments and technique. The entire cervix should be carefully examined at low power, with emphasis on the details of the transformation zone. For the examination to be satisfactory, the entire transformation zone, including the entire squamocolumnar junction, must be visualized. Care must be used when deeming the colposcopic exam satisfactory if previous treatment to the cervix has occurred. The lower extent of the endocervical glandular epithelium should be seen. If visualization of the entire transformation zone is difficult, an endocervical speculum may be useful to complete the examination. Color changes, vascular detail, and the disruptions in the surface contour should be noted. Any vascular change detected at low power should be re-examined at a high magnification. After systematic evaluation with both low and high power and the liberal use of acetic acid, the most suspicious areas should undergo biopsy.10 The depth of the biopsy should be sufficient to obtain stroma, and the epithelium should be cut at right angles to avoid tangential cuts. An endocervical curettage (ECC) is indicated when the lesion extends up the endocervical canal or if the upper extent of the lesion cannot be visualized or cannot undergo biopsy.
Whether an ECC should accompany every colposcopy in nonpregnant women is controversial.10, 11, 12, 13, 14 The routine use of the ECC is accompanied by both a high false-positive rate and a high false-negative rate. In addition, routine ECC causes patient discomfort and a large percentage of inadequate specimens. False-positive results may increase needless excisional procedures. Recent evidence suggests an evaluation of the endocervical canal with a cytobrush is more sensitive than an ECC, and some authors suggest an ECC be performed in patients with satisfactory colposcopy only when the endocervical brush (ECB) test result is positive.15, 16 The goal is to identify occult cervical cancer, so the novice colposcopist should err on the side of an additional evaluation of the endocervical canal by either cytobrush or endocervical curettage. In a study of 66 patients with invasive cancer, failure to perform an ECC was the most common reason for failed diagnosis.11 A meta-analysis of the literature showed that colposcopy without endocervical curettage resulted in more missed invasive carcinoma (34%) than colposcopy with endocervical curettage (15%).17 While some authors suggest an ECC can be eliminated if the colposcopy is unsatisfactory, as these patients will undergo conization, this may result in a missed opportunity to diagnosis invasive cancer and avoid conization.
TREATMENT TECHNIQUES
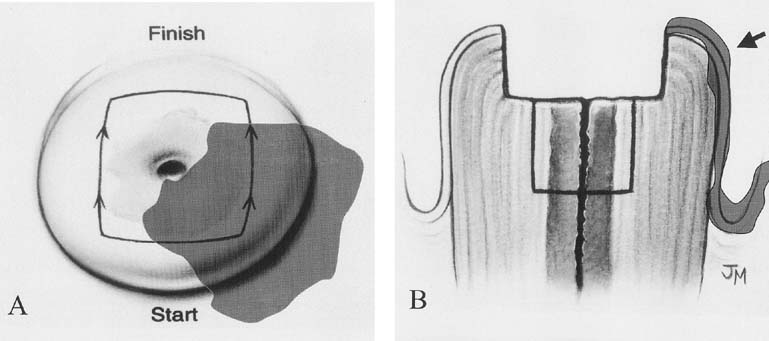
Over the past five decades, a variety of techniques have been developed to treat CIN each based on the concept of ablation or excision of lesions. Ablative techniques include cryosurgery and carbon dioxide (CO2) laser vaporization. Cryosurgery, as the name implies, uses a freezing technique to destroy the abnormal epithelium. It is an older technique that remains popular because it is easy to perform, requires minimal equipment or maintenance, and is associated with minimal patient discomfort in an outpatient/office setting. Either carbon dioxide gas or nitrous oxide is used as the refrigerant for the cryosurgery unit. A thin layer of water-soluble lubricant on the cryotherapy probe allows for a more uniform contact between the probe and the cervix and facilitates a complete freeze. The probe must cover the entire lesion and should create a 4–5-mm ice ball beyond the edge of the probe. The use of a flat cryoprobe without a nippled tip that extends into the cervical canal, as seen in Figure 1, will reduce the possibility of stenosis and is less likely to cause the squamocolumnar junction to recede into the endocervical canal, making follow-up evaluations difficult. The use of a double-freeze technique with 3-minute intervals each of freeze–thaw–freeze appears to improve the efficacy. Local lidocaine anesthesia reduces patient discomfort at the time of the procedure.18 Because the desiccated tissue at the transformation zone is not removed with the procedure, it will slough as a clear watery discharge for 10–14 days after treatment; however, this may persist for as long as 4–6 weeks and women should be prepared for this via pretreatment education.
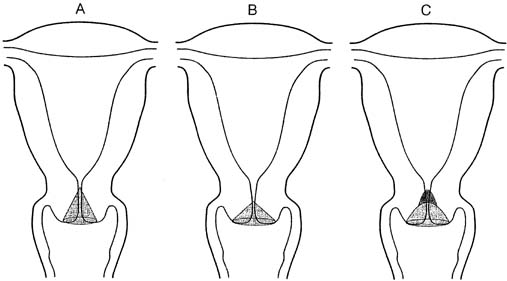
CO2 laser vaporization of the cervix gained popularity in the mid 1980s. It is also a procedure that is easy to perform in the outpatient clinic. Generally, a CO2 laser-mounted on a colposcopy unit is used and the outline of the lesion demarcated. The energy of the laser is absorbed by the water in the tissue and destruction occurs mainly by vaporization. Most instruments have varying power settings and the rate of tissue destruction is dependent on the power setting, the laser spot size, and the duration of tissue exposure. Unlike cryotherapy, the laser allows for very precise tissue destruction and can spare unnecessary destruction of normal tissue by conforming the treatment to the shape of the lesion. Vaporization to a depth of 6–7 mm is required to remove the entire transformation zone and its associated endocervical glands. The treatment causes only minor discomfort in the form of uterine cramps and can be generally performed with local infiltrative anesthesia or a paracervical block. Advantages of the procedure include the precision of the instrument to treat the entire lesion to the appropriate depth and the ability to treat coexisting preinvasive changes of the vagina and vulva, as seen in Figure 2. The disadvantages of the CO2 laser over other techniques include increased procedure time, the expense of the laser unit (and its maintenance), and increased discomfort and bleeding complications.
Ablative or destructive techniques for treating the cervical transformation zone are appropriate only when the extent of the dysplasia is known, colposcopy with directed biopsy is consistent with preinvasive cervical disease, and invasive carcinoma is not suspected. If these criteria are not met, an excisional (cervical conization) procedure must be performed. Although an excisional technique can be selected as therapy for most CIN cases cervical conization is first and foremost considered a diagnostic procedure. The indications for cervical conization are outlined in Table 1. Excisional techniques include cold knife conization, the loop electrosurgical excision procedure (LEEP) as a cone, and CO2 laser conization. The use of a scalpel to excise a cone-shaped piece of tissue or cold-knife conization is the classic technique and has the advantage of allowing cone biopsies of various shapes and sizes to fit the clinical scenario (Fig. 3). A disadvantage of this technique is the need for regional or general anesthesia in an outpatient surgical suite.
Table 1. Indications for cervical conization
| An intraepithelial lesion or microinvasive carcinoma is present in the endocervical curettings |
| Cytologic assessment indicates an abnormality that is not consistent with the tissue diagnosis |
| The entire transformation zone is not visible |
| Microinvasive carcinoma is diagnosed by direct biopsy |
| Cytologic or biopsy evidence of premalignant or malignant glandular epithelium is detected |
(From American College of Obstetricians and Gynecologists: Technical Bulletin, No. 183, 1993)
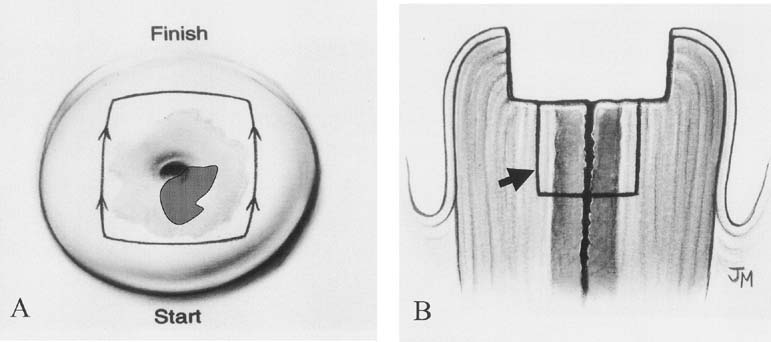
Electrocautery was used extensively in other countries as a destructive technique; the development of thin wire loops that excise the tissue and provide a histopathologic specimen is a more recent development (Fig. 4). The terms large loop excision of the transformation zone (LLETZ) and LEEP have both been used to describe a technique to excise the transformation zone with electrocautery current. This technique is alternatively called diathermy loop excision. It was initially described in Europe and has been extensively used in Great Britain.19 It has become the therapy of choice for many clinicians because it treats the transformation zone similar to ablative techniques and can be used in those clinical situations; however, it also provides a tissue specimen for histopathologic evaluation similar to surgical conization.
|
A cervical LEEP procedure can generally be performed in an outpatient office or clinic setting. Local infiltration of the cervix or paracervical block with lidocaine is recommended. When infiltrating the cervix itself, the use of lidocaine with 1:100,000 epinephrine causes local vasoconstriction that facilitates coagulation of small vessels in the cone bed, thus reducing bleeding from the procedure. Performing the procedure under colposcopic guidance facilitates visualization of the area to be removed. An appropriate loop size is selected to excise the transformation zone to a depth of 6–7 mm, extending 4–5 mm beyond the affected area. A 60–80-watt setting in the cut mode on the electrocautery unit will allow smooth excision and decrease tissue resistance (Fig. 5). In some cases, to avoid using excessively large loops, excision of the anterior and then the posterior portion of the transformation zone can be performed in two separate passes, with a third smaller loop to excise a specific endocervical specimen. Loops less than 20 mm in width and 15 mm in depth are helpful to avoid the excision of a large amount of normal cervical tissue. After removal of the specimen, bleeding areas are cauterized with the ball electrode using coagulation current, and then Monsel's solution (ferrous subsulfate) is applied to the cervix.
While LEEP is most often accomplished in the outpatient office setting, certain circumstances warrant the use of general anesthesia. Indications include cases in which good visualization and access to the cervix are difficult or impossible secondary to patient anatomy or discomfort, an atrophic or stenotic cervix flush with the vaginal wall, and large lesions that extend wide on the cervix or onto the vaginal epithelium.
As the CO2 laser gained popularity in the 1980s, techniques to perform laser conization were also developed. This technique is burdened by the need for regional or general anesthesia in an ambulatory surgery suite, although in some cases it can be performed in the outpatient setting. In addition, the laser cone surgical specimens may have significant cautery artifact which make histopathological evaluation cumbersome. Because the technique of LEEP is more time-efficient, has widespread applicability, and is more easily mastered, it has replaced laser cone in most centers. With appropriate power settings and technique LEEP excision produces minimal cautery artifact.20
TREATMENT INDICATIONS AND CHOICE OF TECHNIQUE
After colposcopy evaluation has been performed, decisions regarding treatment must include an assessment of the degree of dysplasia, the extent of the disease, the age of the patient, and her desires regarding fertility. The main rationale for the identification of CIN and subsequent treatment lies in the fact that a significant percentage of untreated CIN lesions will progress to invasive cervical carcinoma. Truly accurate predictions of the progression and regression rates of cervical dysplasia lesions are limited by many factors; however, it is generally accepted that low-grade lesions have high regression rates and low progression rates while high-grade lesions have a significantly greater risk of progression if left untreated. With this in mind, decisions regarding management of patients with cervical dysplasia can be divided into two subgroups: those with low-grade cervical intraepithelial neoplasia (HPV and CIN I) and those with high-grade cervical intraepithelial neoplasia (CIN II–III/CIS). In 2006 a panel of experts developed a set of consensus guidelines for treatment of CIN in each of these two groups.21
Controversy exists over the treatment recommendations for patients with low-grade CIN lesions, primarily because there is controversy regarding the natural history of these lesions. In a review of more than one dozen series including more than 4000 patients with CIN followed-up primarily by biopsy, Mitchell showed that 45% of these lesions regressed, 31% persisted, and 23% progressed. Of those that progressed, 14% progressed to CIS while only 1.4% progressed to invasive carcinoma.22 In contrast, her review of 353 patients with CIN III/CIS from several series demonstrated that 127 (36%) progressed to invasive carcinoma. While controversy and inconsistently reported results exist, it is generally accepted that low-grade CIN lesions have a high spontaneous remission rate and that most lesions will regress within a 2-year follow-up period.23 Because the time required to progress to invasive cancer is sufficiently long, the risk of invasive cancer occurring during the same 2-year follow-up period is negligible. In the past, it was impossible to determine which low-grade lesions would progress and which ones were more likely to regress. As the technology of HPV detection improves, the use of high-risk HPV testing during observation of low-grade lesions may fill this void.24, 25, 26, 27
Options for the management of low-grade CIN lesions include conservative treatment by ablation or excision of the transformation zone or close follow-up without treatment (observation, expectant management). Patients appropriate for follow-up without therapy must fit select criteria. First, the patient must have undergone complete colposcopic evaluation of the cervix, including cervical biopsies and endocervical curettage. The low-grade lesion should be entirely visualized and confirmed by biopsy. Secondly, the patient must be compliant and reliable for follow-up evaluation. This option is particularly appealing for young patients with limited risk factors for invasive cervical carcinoma who are desirous of fertility. The 2006 consensus guidelines recommend observation for CIN I lesions preceeded by a Pap smear diagnosis of atypical squamous cells – undetermined significance (ASC-US), ASC – cannot exclude high-grade squamous intraepithelial lesion (ASC-H), or low-grade squamous intraepithelial lesion (LSIL) and confirm prior recommendations that CIN I preceeded by high-grade squamous intraepithelial lesion (HSIL) or atypical glandular cells (AGC) requires referral for excisional biopsy.21 Traditionally, follow-up has included surveillance Pap smears every 4–6 months for 2 years then two times per year if low-grade changes persist. In this algorithm, women can return to annual screening only if consecutive normal Pap smear results are obtained. If the lesion progresses during the surveillance period, it should be treated. The use of high-risk HPV testing offers additional information to assist in the selection of patients appropriate for observation. In this population of women, there are extensive data indicating that persistent HPV colonization is necessary for progression of low-grade lesions. Using follow-up data from the ASCUS/LSIL triage study (ALTS), Guido27 compared two follow-up strategies, serial Pap smears (Paps at 6 and 12 months) versus repeat HPV testing at 12 months for women found to have low-grade lesions on colposcopy. In this group of women, the overall rate of progression to CIN III was 7%. Both follow-up strategies resulted in re-referral to colposcopy in approximately 50% of women. The repeat Pap algorithm detected 85% of CIN IIIs and re-referred 60% of women back to colposcopy, whereas HPV testing identified 95% of progression to high-grade lesions and sent 50% of women for repeat colposcopy. These data, coupled with the fact that persistent HPV infection is required for progression to CIN III, indicate that women with low-grade lesions on colposcopy who meet criteria for observation can be managed by a single follow-up visit at 12 months for repeat HPV testing. In this strategy, women with persistent HPV infection are re-referred for colposcopy with appropriate treatment of any high-grade lesions identified or continued close follow-up if a high-grade lesion is not found. In certain instances, observation strategies without therapy can be more costly and cumbersome for both patient and clinician, and treatment for persistent low-grade changes is an option at any time. In patients being observed after a histologic diagnosis of CIN I or less, the degree of information and education regarding HPV and dysplasia that the patient is given can dramatically reduce the amount of psychosocial stress the diagnosis of dysplasia can generate. Some women may find the anxiety associated with observation/no treatment unacceptable, even after they are well-educated about HPV, CIN, and the proposed observation strategies. Given the fact that both conservative treatment and observation with no treatment are reasonable options in the care of women with CIN I and with no conclusive evidence to uniformly support one strategy over the other, a woman's preference to be treated should be considered a key component in decision-making on an individual basis.28, 29, 30
In choosing a technique to treat a low-grade cervical lesion, the ablative techniques have excellent success rates, with more than 90% cure rates; however, with the ease of office LEEP it remains a very common treatment for low-grade lesions.31, 32, 33
Nonpregnant patients with high-grade cervical intraepithelial neoplasia (CIN II–III/CIS) require treatment. The 2006 consensus guidelines reinforce this concept.21 Ablative techniques are only appropriate when invasive cancer has been excluded and there is no indication for cervical conization (Table 1). Contraindications to ablative therapy are outlined in Table 2. If the lesion is small, the entire lesion is well-visualized, and there is no endocervical disease, then cryotherapy can be used for the management of high-grade lesions. However, large lesions that are greater than 2.5 cm-squared have a higher failure rate.34 Cryotherapy is not recommended for large, complex high-grade lesions. CO2 laser vaporization remains popular because it allows greater precision in the destruction of abnormal tissues. For smaller lesions, it has no specific advantage over cryotherapy.34, 35 The main advantage of the CO2 laser is in the treatment of lesions wide on the transformation zone and in situations in which the treatment of cervical dysplasia is concurrent with laser treatment of dysplastic lesions of the vagina and vulva (see Fig. 2).
Table 2. Contraindications to ablative therapy for CIN
| Microinvasive or invasive cervical cancer |
| Lesion extending into endocervical canal |
| Positive endocervical curettage |
| Lack of concordance with cytology and biopsy results (i.e., CIN I after HSIL or AGC Pap) |
| Cryotherapy for lesions >2.5 cm2 or covering two quadrants |
Because of its widespread availability and ease of use, the LEEP procedure has gained popularity for the treatment of high-grade CIN lesions. The main advantage of the LEEP over traditional ablative procedures is that there is a histologic specimen for evaluation. A number of series have demonstrated invasive cancer occurring within 2 years of ablative therapy, suggesting incomplete treatment of occult invasive carcinoma.11, 35 Other advantages include the ease of outpatient use and low complication rates. These techniques produce minimal discomfort like cryosurgery and laser therapy. The actual time required to perform the LEEP excision is less than that of laser ablation of the cervix. Since the introduction of the technique, a number of large series treating thousands of patients have documented excellent treatment outcomes ranging from 91% to 98%.19, 36, 37, 38, 39 In one series, LEEP was compared in a randomized fashion to CO2 laser and found to be superior with less hemorrhage, less patient discomfort, and decreased procedure time.39
Two unique problems have emerged with the increasing use of LEEP procedures, including the removal of excessive amounts of tissue and the danger of overtreatment. While many advocate a see and treat philosophy, there are pitfalls to this approach. Advantages to performing colposcopic evaluation and treatment at one office visit (see and treat) include avoidance of patients lost to follow-up in noncompliant populations and decreased expense from office visits. In an inner city population in New York, 26.9% of patients were noncompliant with scheduled appointments for CO2 laser vaporization after discussion of biopsy results.36 However, an aggressive approach with treatment before obtaining biopsy results can lead to overtreatment. The number of negative specimens in see and treat series range from 14% to 32.5%.38, 40 Negative specimens were associated with smaller lesions and with younger women. Factors contributing to a higher rate of negative see and treat specimens might also include more liberal use of colposcopy to evaluate low-grade lesions on Pap smear. This is particularly relevant for young women who desire preservation of fertility. The see and treat approach may be appropriate for noncompliant patients with a high-grade lesion on Pap that are unequivocal on colposcopy. The majority of women in the United States, however, would probably benefit from discussion and planned therapy after biopsy results are available. As with the anxiety associated with the initial abnormal Pap diagnosis and colposcopy process, a focus on patient education that stresses the importance of treatment in a nonthreatening way can dramatically reduce treatment-related anxiety, and thus improve compliance with planned therapy.29, 41
When indications for an excisional procedure exist, a cervical conization is mandatory. The indications for diagnostic conization are outlined in Table 1. As previously mentioned, techniques for cervical conization include cold-knife conization, laser conization, and the use of the LEEP as cone. While some practitioners continue to use a laser for conization of the cervix, use of the LEEP as a cone has replaced the laser by many because it is easier to use. The choice of technique will often be dictated by the nature of the lesion. As depicted in Figure 3, the conization specimens obtained will vary based on technique.
The surgeon has the most control and ability to obtain an intact specimen when a scalpel is used to perform the cone biopsy. While the wire loop may be used in certain circumstances to perform the cone biopsy, there are situations in which a traditional cold-knife conization is preferred. In cases of microinvasive carcinoma diagnosed by colposcopy-directed biopsy, an intact liberal cone biopsy specimen is important to establish the depth of invasion and margin status, which are important factors used to guide further treatment decisions. Similarly, a cone biopsy performed to evaluate premalignant or malignant glandular epithelium should include a cone of appropriate depth. While wire loops can in some cases achieve a narrow deep intact specimen, it is more difficult than with the use of a scalpel. A truly positive endocervical curettage should also be evaluated with careful attention to the depth of the conization specimen. Because the use of a LEEP to perform a cone biopsy is less expensive and able to be performed in the outpatient setting, there are circumstances when its use may be advantageous. When concern for an invasive carcinoma is low and the cytology is not consistent with tissue biopsy or the entire transformation zone is not visible, a LEEP excision may be appropriate to further evaluate the lesion. It may also be helpful in patients in whom a positive endocervical curettage or cytobrush is likely to be a false-positive or artifactual. The difficulty with the use of the LEEP for excisional purposes is that it is more difficult to tailor the excision to the indication, and fragmented cone biopsies are often difficult for the pathologist to evaluate and clearly determine margin status. In summary, while the LEEP can be used for a conization procedure in lieu of traditional cold-knife conization, its use in this manner should be limited to select cases.
CIN complicating pregnancy
The same screening and diagnostic maneuvers including cytology, HPV testing, and colposcopy are used to evaluate women during pregnancy. Pregnancy offers an opportunity to provide cervical cancer screening to women who otherwise might never be screened, because it is often one of the few times some women enter the health care system. Unless invasive cancer is highly suspect, diagnostic colposcopic biopsy with observation throughout pregnancy is currently recommended for all grades of dysplasia.42, 43, 44 Excisional procedures including conization and LEEP during pregnancy increase risks of preterm contractions and/or delivery and are both associated with substantial blood loss.42, 43 Conization should only be considered during pregnancy when invasive cancer is suspected and has not been diagnosed or satisfactorily excluded by colposcopic-directed biopsy. Women followed-up with dysplasias during pregnancy should be re-evaluated by colposcopy after complete involution of the uterus and cervix (6–8 weeks) with appropriate management based on abnormalities found at that time.44
TREATMENT OF RECURRENT DYSPLASIA
In general, both ablative or excisional treatment of CIN are successful; however, women treated for CIN remain at increased risk for the development of cervix cancer compared with women without CIN. Surveillance after treatment should be designed to identify women with treatment failures as well as those in whom recurrent CIN develops. Persistence of a lesion (incomplete treatment) or recurrent CIN has been described in 1–20% of cases. Factors associated with persistent or recurrent disease include age older than 40 years, glandular involvement, large lesions, and positive treatment margins. Serial repeat Pap smears performed at 3–6-month intervals for several years have been generally successful in identifying persistent or recurrent CIN; however, as has been the case in triage, diagnosis, and observation of low-grade lesions, the identification of persistent high-risk HPV types is proving to be an important part of posttreatment algorithms. Negative posttreatment HPV testing has been shown to predict treatment success in several trials. The majority of women with recurrent CIN have persistent positive high-risk HPV tests while recurrence is rare in the face of negative follow-up HPV testing.45, 46, 47, 48 The use of HPV testing is particularly attractive as it is often difficult to visualize the entire transformation zone after previous cryosurgery, CO2 laser, or LEEP. Practitioners may consider follow-up colposcopy 3–6 months after treatment in select cases, but this is not routinely necessary. When several consecutive smears are within normal limits and/or a repeat high-risk HPV test is negative for persistent infection, the patient can return to annual screening. If recurrent dysplasia is noted on follow-up Pap, the patient should undergo repeat colposcopy. Recurrent dysplasia documented by directed biopsy should be treated with cold-knife conization or LEEP conization. In cases in which invasive carcinoma has been excluded and fertility is not desired, vaginal hysterectomy can be considered. Care should be taken to evaluate for vaginal involvement in these recurrent cases, because failure to treat concomitant vaginal dysplasia may result in persistently abnormal smears.
An important part of posttreatment surveillance includes patient education regarding healthy lifestyle modifications that may potentially reduce the risk of recurrent disease or the progression of low-grade lesions once identified. A substantial collection of epidemiologic data has indicated that deficiencies in several dietary micronutrients is statistically associated with the development of and/or progression of cervical dysplasia already present.49, 50, 51, 52, 53, 54 Although epidemiologic data have linked low-serum levels of vitamin C, folic acid, vitamin B6, vitamin B12, beta-carotene, indol-3-carbinols, and lycopene to the presence of dysplasia, no clinical trial to date has been able to demonstrate a therapeutic effect of these micronutrients for the treatment of established dysplasia.55 Despite the lack of therapeutic data in established CIN, the epidemiologic data are strong enough to recommend a diet rich in antioxidant vitamins, beta-carotene, indol-3-carbinols, and lycopene as a potential prevention strategy.55 Other healthy lifestyle practices including avoidance of excess alcohol intake, obtaining adequate sleep, and regular exercise have all been shown to promote a healthy immune system, an important factor in the prevention of cervical neoplasia. By far, the most important and most well-documented lifestyle factor is cigarette smoking. Smoking has been directly linked to the promotion of cervical neoplasia. In multiple studies, the cessation of smoking has been shown to reduce the risk of recurrent dysplasia.56, 57, 58 Through education and patient support, these factors can all contribute to minimizing any individual woman's risk for persistent or recurrent dysplastic disease.
TREATMENT COMPLICATIONS
While cryotherapy, CO2 laser therapy, and LEEP excision all have excellent success rates in the treatment of dysplasia, each is associated with some risk of complication. Cryotherapy has the lowest rates of bleeding and infection but has higher failure rates when treating large lesions. Both laser and LEEP may be associated with bleeding, but complication rates are low. Posttreatment bleeding occurs in 2–7% of LEEP procedures,20, 38, 59, 60 with bleeding significant enough to result in hospitalization in only 1–2%. Long-term morbidity of these procedures is minimal. Scarring severe enough to result in unsatisfactory colposcopic examination occurs in 1.3% to 9% of patients undergoing LEEP and 1.3–3.8% have cervical stenosis after the procedure.59 The risk of cervical stenosis and its resulting hydro-hematometra is much higher in women who have a LEEP that extends 1.5 cm or more into the endocervical canal and in women who have had previous ablative therapy.
Ablative techniques such as cryotherapy or CO2 laser for treatment of dysplasia have less impact on future fertility than surgical conization. Several studies have addressed the impact of LEEP procedures on subsequent pregnancy outcome with favorable results. Two case–control studies showed that compared with controls, patients with a history of a cervical LEEP procedure had no higher rate of prematurity or cesarean delivery.61, 62 Impact on fertility is more difficult to obtain, but no clear association between decreased fertility and LEEP procedures has been demonstrated. In general, excision depth should be limited to less than 7–10 mm in patients desiring to preserve fertility, and repeat excisions should be performed with caution, and for good reason, in young patients.
INVESTIGATIONAL TREATMENTS
Targeting HPV through vaccination may ultimately prove to prevent a significant number of cervical dysplasias and cancers worldwide. Similar immunization strategies as treatment for dysplasias have met with moderate success. Current immunization strategies have used fragments of HPV-associated DNA, RNA, and proteins as tumor-associated antigens, and many different adjuvants have been used in immunization strategies. Most strategies put forth to date have been successful from an immunologic standpoint in that they result in the generation of tumor-specific/HPV-specific cytotoxic T cells. Unfortunately, these immunologic responses have not translated into significant clinical responses, and the majority of women treated continue to have persistent dysplasias.63,64,65 Further investigations into the immunosuppressive properties of HPV-associated dysplasia are ongoing and will be key to providing effective immunization as treatment for dysplasia or invasive cancer.
CONCLUSION
While the goal of eliminating all cases of cervical cancer has not been realized, there have been significant advances in the diagnosis and treatment of preinvasive lesions of the cervix. Refinements in treatment techniques have allowed many women to undergo conservative treatment and avoid surgical conization and hysterectomy. By carefully choosing treatment modalities for individual patients, physicians can avoid unnecessary discomfort and cost from overtreatment of benign lesions or, more seriously, undertreating or misdiagnosing a malignant lesion.
REFERENCES
Mitchell A, Lindsay J, Hill G: Mortality from cancer of the uterus in Canada and its relationship screening for cancer of the cervix. Int J Cancer 17: 602, 1976 |
|
American Cancer Society Inc: 2003. Cancer Facts and Figures 2003. Available at http://www.cancer.org |
|
Richart RM: Natural history of cervical intraepithelial neoplasia. Clin Obstet Gynecol 10: 748, 1967 |
|
McIndoe WA, McLean MR, Jones RW et al: The invasive potential of carcinoma in situ of the cervix. Obstet Gynecol 64: 451, 1984 |
|
Richart RM, Wright TC: Controversies in the management of low-grade cervical epithelial neoplasia. Cancer 71: 1413, 1993 |
|
Bethesda 2001: 2001 terminology and recommendations. Available at http://bethesda2001.cancer.gov. |
|
Kurman R, Malkasian G et al: From Papanicolaou to Bethesda: The rationale for a new cervical cytologic classification. Obstet Gynecol 77: 779, 1991 |
|
Ismail SM, Colclough AB, Dinne JS et al: Reporting cervical intraepithelial neoplasia (CIN: Intra-Inter pathologist variation and factors associated with disagreement). Histopathology 16: 371, 1990 |
|
Sherman ME, Schiffman MH, Erozan YS et al: Bethesda system. A proposal for reporting abnormal cervical smears based on the reproducibility of cytopathologic diagnoses Arch Pathol Lab Med 116: 1155, 1992 |
|
Hartenbach EM, Johnson PR, Twiggs LB: Colposcopy: anatomical and histopathological basis, technique, and interpretation. In: Rubin SC, Hoskins WJ, (eds): Cancer of the Cervix. pp 115–126, Vol 1: Philadelphia, Lippincott-Raven, 1996 |
|
Townsend DE, Richart RM, Marks E: Invasive cancer following outpatient evaluation and therapy for cervical disease. Obstet Gynecol 57: 145, 1981 |
|
Moseley KR, Dinh TV, Hannigan EV et al: Necessity of endocervical curettage in colposcopy. Am J Obstet Gynecol 154: 992, 1986 |
|
Andersen W, Frierson H, Barber S et al: Sensitivity and specificity of endocervical curettage and the endocervical brush for the evaluation of the endocervical canal. Am J Gynecol 159: 702, 1988 |
|
Hatch KD, Shingleton HH, Orr JW et al: Role of endocervical curettage in colposcopy. Gynecol 65: 403, 1985 |
|
Hoffman MS, Sterghos S, Gordy LW et al: Evaluation of the cervical canal with the endocervical brush. Obstet Gynecol 82: 573, 1993 |
|
Weitzman GA, Korhonen MO, Reeves KO et al: Endocervical brush cytology; and alternative to endocervical curettage? J Reprod Med 33: 677, 1988 |
|
Helmerhorst TJM: Clinical significance of endocervical curettage as part of colposcopic evaluation: A review. Int J Gynecol Cancer 2: 256, 1992 |
|
Sammarco MJ, Hartenbach EM, Hunter VJ: Local anesthesia for cryosurgery of the cervix. J Reprod Med 38: 170, 1993 |
|
Prendiville W, Cullimore J, Norman S: Large loop excision of the transformation zone (LLETZ). A new method of management for women with cervical intraepithelial neoplasia Br J Obstet Gynecol 96: 1054, 1989 |
|
Herzog TJ, Williams S, Adler LM et al: Potential of cervical electrosurgical excision procedure for diagnosis and treatment of cervical intraepithelial neoplasia. Gynecol Oncol 57: 286, 1995 |
|
Wright TC Jr, Massad LS, Dunton CJ et al: 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. J Low Genit Tract Dis 11: 223–239, 2007 |
|
Mitchell MF, Schottenfeld D: The natural history of cervical intraepithelial neoplasia and management of the abnormal papanicolaou smear. In: Rubin SC, Hoskins WJ, (eds): Cancer of the Cervix. pp 103–113, Vol 1: Philadelphia, Lippincott-Raven, 1996 |
|
Holowaty P, Miller AB, Rohan T, To T: Natural history of dysplasia of the uterine cervix J Natl Cancer Inst 91: 252, 1999 |
|
Solomon D, Schiffman MH, Tarone B et al: Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. Natl Cancer Inst 93: 293–299, 2001 |
|
Bosch FX, Lorincz A, Munoz N et al: The causal relationship between human papillomavirus and cervical cancer. J Clin Pathol 55: 244, 2002 |
|
Nobbenhuis M, Walboomers JM, Helmerhorst T et al: Relation of human papillomavirus status to cervical lesions and consequences for cervical cancer screening: a prospective study. Lancet 354: 354, 1999 |
|
Guido R, Solomon D, Schiffman M et al: Comparison of management strategies for women diagnosed with CIN I or less postcolposcopic evaluation: data from the ASCUS and LGSIL Triage Study (ALTS), a multicentered randomized trial. J Low Gen Tract Dis 6: 176, 2002 |
|
Bjork S, Hagstrom HG: Of what significance is abnormal results of smear test? Anxiety because of insufficient information in connection with abnormal results of cervical smear test Lakartidningen 98: 2796, 2001 |
|
Jones MH, Singer A, Jenkins D: The mildly abnormal cervical smear: patient anxiety and choice of management. J R Soc Med 89: 257, 1996 |
|
Wilkinson C, Jones JM, McBridge J: Anxiety caused by abnormal results of cervical smear test: a controlled trial. BMJ 300: 440, 1990 |
|
Benedet JL, Miller DM, Nickerson KG: Results of conservative management of cervical intraepithelial neoplasia. Obstet Gynecol 79: 105, 1992 |
|
Kaufman RH, Irwin JF: The cryosurgical therapy of cervical intraepithelial neoplasia. Am J Obstet Gynecol 131: 381, 1978 |
|
Hatch KD, Shingleton HM, Austin JM et al: Cryosurgery of cervical intraepithelial neoplasia. Obstet Gynecol 57: 692, 1981 |
|
Townsend DE, Richart RM: Cryotherapy and carbon dioxide laser management of cervical intraepithelial neoplasia: a controlled comparison. Obstet Gynecol 61: 75, 1983 |
|
Ferenczy A: Management of patients with high grade squamous intraepithelial lesions. Cancer 76: 1928, 1995 |
|
Spitzer M, Schernys AE, Seltzer VL: The use of large-loop excision of the transformation zone in an inner-city population. Obstet Gynecol 82: 731, 1993 |
|
Wright TC, Gagnon S, Richart RM et al: Treatment of cervical intraepithelial neoplasia using the LOOP electrosurgical excision procedure. Obstet Gynecol 79: 173, 1992 |
|
Ferenczy A, Choukroun D, Arseneau J: Large loop excision procedure for squamous intraepithelial lesions of the cervix: advantages and potential pitfalls. Obstet Gynecol 87: 332, 1996 |
|
Gunasekera PC, Phipps JH, Lewis BV: Large loop excision of the transformation zone (LLETZ) compared to carbon dioxide laser in the treatment of CIN: a superior mode of treatment. Br J Obstet Gynaecol 97: 995, 1990 |
|
Alverez RD, Helm CW, Edwards RP et al: The prospective randomized trial of LLETZ verses laser ablation in patients with cervical intraepithelial neoplasia. Gynecol Oncol 52: 175, 1994 |
|
Marteau TM: Psychological effects of an abnormal smear result. Large Loop Excision of the Transformation Zone. A Practical Guide to LLETZ. pp 65–72, London, Livingston Int, 1993 |
|
Goldberg G, Altaras MM, Bloch B: Cone cerclage in pregnancy. Am J Obstet Gynecol 77: 315, 1991 |
|
Robinson W, Webb S, Tirpack J et al: Management of cervical intraepithelial neoplasia during pregnancy with LOOP excision. Gynecol Oncol 64: 153, 1997 |
|
Connor JP: Noninvasive cervical cancer complicating pregnancy. Obstet Gynecol Clin North Am 25: 331, 1998 |
|
Paraskevaidis E, Lolis ED, Koliopoulos G et al: Cervical inreaepitheal neoplasia outcomes after large loop excision with clear margins. Obstet Gynecol 95: 828, 2000 |
|
Bodner K, Bodner-Adler B, Wierrani F et al: Is therapeutic conization sufficient to eliminate high risk HPV infection of the uterine cervix? A clinicopathologic analysis. Anticancer Res 22: 3733, 2002 |
|
Chua K-L, Hjerpe A: Human papillomavirus analysis as a prognostic marker following conization of the cervix uteri. Gynecol Oncol 66: 108, 1997 |
|
Acladious NN, Sutton C, Mandal D et al: Persistent human papillomavirus infection and smoking increase risk of failure of treatment of cervical intraepithelial neoplasia (CIN). Int J Cancer 98: 435, 2002 |
|
Ho G, Palan PR, Basu J et al: Viral characteristics of human papillomavirus infection and antioxidant levels as risk factors for cervical dysplasia. Int J Cancer 78: 594–599, 1998 |
|
Romney SL, Palan PR, Basu J et al: Nutrient antioxidants in the pathogenesis and prevention of cervical dysplasias and cancer. J Cell Biochem 23: 96–103, 1995 |
|
Wylie-Rosett JA, Romney SL, Slagle NS et al: Influence of vitamin A on cervical dysplasia and carcinoma in situ. Nutr Cancer 6: 49–57, 1984 |
|
Liu T, Soong SJ, Wilson NP et al: A case control study of nutritional factors and cervical dysplasia. Cancer Epidemiol Biomarkers Prev 2: 525–530, 1993 |
|
Palan PR, Mikhail MS, Goldberg GL et al: Plasma levels of beta-carotene, lycopene, canthaxanthin, retinol, and alpha-and tau-tocopherol in cervical intraepithelial neoplasia and cancer. Clin Cancer Res 2: 181–185, 1996 |
|
Alberg AJ, Selhub J, Shah KV et al: The risk of cervical cancer in relation to serum concentrations of folate, vitamin B12, and homocysteine. Cancer Epidemiol Biomarkers Prev 9: 761–764, 2000 |
|
Palan PR, Chang CJ, Mikhail MS et al: Plasma concentrations of micronutrients during a nine-month clinical trial of beta-carotene in women with precursor cervical cancer lesions. Nutr Cancer 30: 46–52, 1998 |
|
Barton SE, Maddox PH, Jenkins D et al: Effects of cigarette smoking on cervical epithelial immunity: A mechanism for neoplastic change? Lancet 2: 652, 1988 |
|
Prokopczyk B, Cox JE, Hoffmann D et al: Identification of tobacco specific carcinogen in the cervical mucus of smokers and none-smokers. J Natl Cancer Inst 89: 868, 1997 |
|
Moore T, Moore A, Carrasco D et al: Human papillomavirus, smoking, and cancer. J Cutan Med Surg 5: 323, 2001 |
|
Wright TC, Richart RM: Loop excision of the uterine cervix. Curr Opin Obstet Gynecol 7: 30, 1995 |
|
Prendiville W: Large loop excision of the transformation zone. Clin Obstet Gynecol 38: 622, 1995 |
|
Haffenden DK, Bigrigg A, Codlinhg BW et al: Pregnancy following large loop excision of the transformation zone. Br J Obstet Gynaecol 100: 1059, 1993 |
|
Blomfield PI, Buxton J, Dunn J et al: Pregnancy outcome after large loop excision of the cervical transformation zone. Am J Obstet Gynecol 169: 620, 1993 |
|
Sherman M, Schiffman M, Stickler H et al: Prospects for a prophylactic HPV vaccine: Rationale and future implications for cervical cancer screening. Diag Cytopathol 18: 5, 1998 |
|
Hines J, Ghim S, Jenson AB: Prospects for human papillomavirus vaccine development: emerging HPV vaccines. Curr Opin Obstet Gynecol 10: 15, 1998 |
|
Adams M, Mborysiewicz L, Fiander A et al: Clinical studies of human papillomavirus vaccines in pre-invasive and invasive cancer. Vaccine 19: 2549, 2001 |