Authors
INTRODUCTION
In treating any patient with urinary incontinence, the goal is to provide the patient with a cure from her symptoms and improve her quality of life. To obtain this goal consistently, considering the variability among patients and the multiple factors contributing to the development of incontinence, physicians must be well aware of the various treatment options and their indications. Suburethral sling procedures have long been a mainstay in the surgical treatment for female stress urinary incontinence.
Traditionally, suburethral sling procedures were reserved for patients with recurrent stress urinary incontinence. During the past century, indications have been expanded to include not only those patients with the severe form of stress urinary incontinence, namely intrinsic sphincter deficiency (ISD), but also patients with routine stress incontinence in conjunction with comorbid conditions.
With hopes of improving the treatment of stress incontinence symptoms, interest in primary and secondary slings has increased. The sling procedure is now often considered in any patient with stress urinary incontinence. The suburethral sling procedure requires careful attention to patient selection, workup, surgical technique, and avoidance of complications. The history of the sling procedure, patient evaluation and indications, surgical techniques, and complications of the sling procedure will be discussed here.
HISTORY
Since the first reported case in the early 1900s, the suburethral sling procedure has seen many changes. All aspects of the sling, including its indications, materials, and techniques used, have undergone a generation of change. With each change, there was improvement on the previous modification.
The earliest described sling procedure was in 1907 by Giordano, who used the gracilis muscle. In 1926, Giordano's technique was applied to a case of epispadias by Denning. In 1910, Goebell first described the use of freed pyramidalis muscle suburethrally. This was followed in 1914 by Fragenheim's modification of Goebell's technique, which employed fascial attachments of the pyramidalis muscles and the recommendation for use of the rectus abdominis muscles when the pyramidalis muscles were inadequate. The final modification to this technique in 1917 was by Stoeckel, who combined a vaginal plastic operation with muscular plication at the vesical neck. This is known as the Goebell-Fragenheim-Stoeckel technique.
Further modifications of the sling procedure were reported in 1923 by Thompson, using rectus muscle and fascia, and later in 1929 by Martius, using bulbocavernosus muscle and its surrounding fatty tissue transplanted suburethrally.1
In the early 20th century, sling procedures were described that included the use of a number of autologous grafts. Muscle sling grafts were later abandoned secondary to difficulty in maintaining an adequate vascular and neural supply and therefore a viable graft. In 1942, Aldridge described yet another modification of the sling procedure using the aponeurosis of the external oblique muscles,. This procedure most resembles the modern fascial sling. In his procedure, Aldridge harvested two strips of fascia, maintaining medial attachment, and passed the lateral arms inferiorly to be sutured suburethrally at the level of the urethrovesical junction. In the same report, Aldridge discussed the advantages of autologous fascia lata over abdominal wall fascia.1
A more recent modification was described by Raz and colleagues2 in 1989. In this report, an in situ vaginal wall patch was used suburethrally in conjunction with suture arms. Cure of stress incontinence was reported in 94% of patients with ISD.
Difficulties with autologous grafts include inadequate length or poor quality of the tissue and the complications of a harvesting technique (i.e., additional incision, risk of incisional hernia at harvesting site). Surgeons continued to search for the ideal graft material and switched from organic graft to inorganic materials. First reported was a nylon sling by Bracht in 1956.3 Later use of inorganic grafts included Silastic sheets (silicone), Mersilene, Marlex, and Gore-tex slings. In 1962, Williams and TeLinde4 reported the use of a Mersilene sling in 12 patients. Complications included abscess formation with a persistent sinus tract and urethral trauma. At the time the authors did not believe the Mersilene to be the etiology of the infection, but rather believed it to be the vaginal surgical route and therefore equal to a fascial sling. In 1985, Stanton and colleagues5 reported on 30 Silastic sling procedures with an 83% subjective and objective short-term cure rate. Silastic sheets were chosen because of the consistent strength, lack of incorporation into surrounding tissues, local fibrous sheath response, and therefore ease of removal, if necessary. In 1988, Horbach and associates6 reported on the use of Gore-tex slings with a short-term 85% subjective and objective cure rate. The tension-free vaginal tape sling procedure (TVT), first described in Sweden by Ulmsten and Petros7 in 1995, incorporated several different materials in the original series. Since 1996, however, the TVT procedure has used a unique prolene mesh sling.8 Complications of inorganic graft materials have included urinary retention requiring surgical revision, urethral irritation, necrosis, and graft infection and erosion.
The most recent modification of the widely used synthetic slings includes single incision slings or "minislings". TVT Secur (Ethicon) was the first of these slings to be released in 2006 followed by Miniarc (AMS) in 2007. These slings are modifications of their predecessors with a shorter mesh placed via a single vaginal incision. These slings offer the potential for fewer complications such as less blood loss and a decreased probability of bladder or nerve injury due to use of a shorter mesh tape; however, comfirmative data is pending.
A return to the use of organic materials has occurred with the use of allografts such as cadaveric fascia lata, dermis, pericardium, dura, and heterologous grafts such as porcine small intestine submucosa and dermis.
As surgeons continue to search for the ideal graft material, organic (homologous and heterologous) and inorganic graft materials continue to be employed. No study has compared organic with inorganic grafts. As yet, the ideal material has not been identified, and the selection continues to be the surgeon's choice.
INDICATIONS
As recommended by the Agency for Health Care Policy and Research (AHCPR), all patients with complaints of urinary incontinence should undergo a basic evaluation that includes a medical history, physical examination, measurement of postvoid residual volume, and urinalysis. Particularly important in the history is a detailed exploration of the incontinence symptoms, including duration, frequency, precipitating factors, other lower urinary tract symptoms, and possible risk factors, including prior treatments. During the physical examination, a focus on the pelvic examination, with emphasis on site-specific support defects, will identify concurrent prolapse conditions while assessing the integrity of the urogenital tissue. Patients with a complicated history in terms of severity of disease, recurrence of symptoms, or presence of comorbid conditions should undergo further evaluation with urodynamic testing, endoscopy, and/or imaging studies.9
Genuine stress incontinence (GSI) is defined as the involuntary loss of urine occurring when, in the absence of a detrusor contraction, the intravesical pressure exceeds maximum urethral pressure.10 Patients with GSI are often categorized according to the presence or absence of urethral hypermobility. Early definitions of GSI classified patients as types I, II, and III. Type I was defined as straightening of the posterior urethrovesical angle to 180° or greater with straining. Type II consisted of the changes seen in type I, together with an increase of greater than 45° in the urethral axis in the vertical plane. Type III was associated with a fixed, “lead-pipe”, urethra.11
The term “intrinsic urethral sphincter deficiency” was first described by the AHCPR in 1992 as a cause of GSI.12 This condition is considered a more severe form of GSI and is defined as a subset of patients with GSI whose urethral sphincteric mechanisms fail to maintain sufficient resistance for urinary continence either at rest or in the presence of minimal physical exertion. The AHCPR guidelines recommend preoperative identification of patients with ISD, suggesting the use of various tests. However, despite these guidelines, a specific definition of ISD is not provided. Additional terms such as low-pressure urethra and type III incontinence have been used, but these entities are not interchangeable. Recommended management of the patient with ISD includes sling procedures, periurethral bulking agents, and artificial urethral sphincter.
Traditionally, as recommended by the AHCPR, sling procedures have been indicated in patients with either GSI caused by ISD or recurrent GSI. Expanded indications include patients with GSI with comorbid conditions that increase the risk of surgical failure. The high risk of surgical failure is associated with a tendency for repetitive increased abdominal pressure. High-risk conditions include chronic bronchitis/asthma, severe obesity, chronic steroid use, congenital tissue weakness, and a history of recreational or occupational heavy lifting or high impact.13
INTRINSIC SPHINCTER DEFICIENCY
Much clinical research has been done in an attempt to identify and define the patient with ISD. McGuire14 described a subset of patients whose symptoms had failed to respond to multiple operations for the treatment of stress incontinence. In this report, 75% of patients who failed to respond to multiple operations were defined as having type III incontinence (urinary loss associated with stress, with variable urethral mobility from none to marked, and urethral closure pressures less than 20 cmH2O). However, the finding of type III incontinence is not clearly noted as a cause of the surgical failure or an effect.
The association of multiple prior procedures with lower urethral closure pressure on urodynamic testing was confirmed in 1983 by Hilton and Stanton.15 In this report, continent and stress incontinent women were compared by urodynamic testing, specifically urethral pressure profilometry. Women with three or more prior anti-incontinence operations, age more than 60 years, and more severe symptoms of stress incontinence, as demonstrated objectively, were found to have lower mean maximum urethral closure pressures.
The relationship between low urethral closure pressure and outcome with a specific anti-incontinence procedure was later described.16 Subjects were grouped according to preoperative maximum urethral closure pressure (group 1, 20 cmH2O or less; group 2, more than 20 cmH2O), and all patients underwent Burch colposuspension (Tanagho modification). A 54% failure rate was seen in the low-pressure group. No significant difference was identified between the groups except for age. The low-pressure group was statistically older (mean age 53.3 years).
Further research evaluated 13 clinical characteristics as possible predictors of ISD, as defined by a maximum urethral closure pressure of 20 cmH2O or less.17 Clinical characteristics including age, gravidity, parity, estrogen status, prior hysterectomy, number and type of prior incontinence surgeries, associated presenting symptoms of urgency, frequency, or urge incontinence, maximum straining Q-tip angle, postvoid residual volume, and uroflow pattern were evaluated retrospectively. The only identifiable statistical predictor of ISD was an age older than 50 years.
Maximum urethral closure pressure evaluates the urethral sphincter mechanism at rest and therefore refers to the passive continence mechanism. An active test of the continence mechanism is the stress leak point pressure, either during a Valsalva maneuver or a cough. Comparison of maximum urethral closure pressure to stress leak point pressure in patients with GSI revealed a significant positive correlation. With stress leak point pressure as a diagnostic tool to define low-pressure urethra, a critical value of 45 cmH2O results in a sensitivity of 80% and a specificity of 90%. However, if stress leak point pressure is to be used as a screening tool, a critical value of 60 cmH2O shows an improved sensitivity of 90% with a reduced specificity of 64%.18
McLennan and Bent19 reported a comparison of stress leak point pressure and maximum urethral closure pressure with the supine empty stress test (postvoid residual volume less than 100 cc). The supine empty stress test was found to be a screening tool for low (60 cmH2O or less) stress leak point pressure but not for low (20 cmH2O or less) maximum urethral closure pressure. Similarly, Hsu and coworkers20 showed a sensitivity and specificity of at least 90% for the supine stress test (bladder volume = 200 cc) in comparison to low (100 cmH2O or less) stress leak point pressure.
Prior attempts to define the spectrum of GSI and its subset of patients with ISD by clinical and urodynamic evaluation emphasized age, prior surgical history, severity of incontinence history, extent of urethral mobility, maximum urethral closure pressure, and stress leak point pressure testing. In 1997, Bump and colleagues21 reported on the comparison of the latter three parameters. Low stress leak point pressure was consistently strongly associated with worse symptomatic incontinence. Sensitivities, specificities, and positive and negative predictive values among the three parameters were low, ranging from 40 to 85%. Subjects with all three parameters present had the worst incontinence. As previous work suggests, subjects with positive parameters were found to be significantly older and more likely to have had a prior hysterectomy or anti-incontinence or prolapse surgery, and averaged a higher number of prior procedures.
More recent studies support the idea that patients with urodynamic evidence of intrinsic sphincter deficiency have lower rates of dryness after surgical treatment of their stress urinary incontinence.22, 23 Furthermore, some studies suggest that they may have higher success rates with use of retropubic slings rather than transobturator slings.24 This information is important in counseling patients pre-operatively as well as choosing the procedure that offers them the best chance of cure.
In summary, recommendations for the diagnosis of ISD included a composite of historic, urodynamic, anatomic, and clinical severity criteria.21
SURGICAL TECHNIQUES
Once the incontinence workup is completed and the decision to proceed with a sling procedure has been made, options remain. First is the choice of graft material. Organic grafts require a harvesting procedure or can be obtained from a tissue bank. Autologous grafts include vaginal epithelium, rectus fascia, or fascia lata. Allografts include cadaveric dermis, fascia lata, dura, and pericardium. Heterologous grafts include porcine dermis and small intestine submucosa. Multiple inorganic grafts are readily available. Second is the choice of surgical approach. The various sling procedures performed today are technically somewhat similar. Previous sling procedures were performed using a combined abdominal and vaginal approach, with most of the dissection performed vaginally; however, the new obturator and single-incision slings require only vaginal dissection. As reported in the early 1900s, a complete abdominal approach is possible but may be associated with increased urethral injury. Early avoidance of a combined procedure was common because of concern about vaginal contamination and increased postoperative infection. With today's improved surgical techniques and antibiotic coverage, combined abdominal and vaginal procedures are safe. Sling variations include a full-length sling, a patch sling, a TVT sling, Obturator slings (TVT-Obturator, Monarch, TOT), or single-incision sling (TVT Secur, Miniarc).
As part of the preoperative preparation, the risks and benefits of the procedure, along with postoperative restrictions, are reviewed with the patient. Many surgeons teach all patients clean intermittent self-catheterization before surgery. On the day of surgery, the patient should receive appropriate antibiotic prophylaxis, according to patient allergy and medical history, 60 minutes before surgery. The patient is positioned in the dorsal lithotomy position and prepared and draped in a sterile fashion for abdominal and vaginal surgery. A Foley catheter is placed transurethrally.
Full-Length Sling
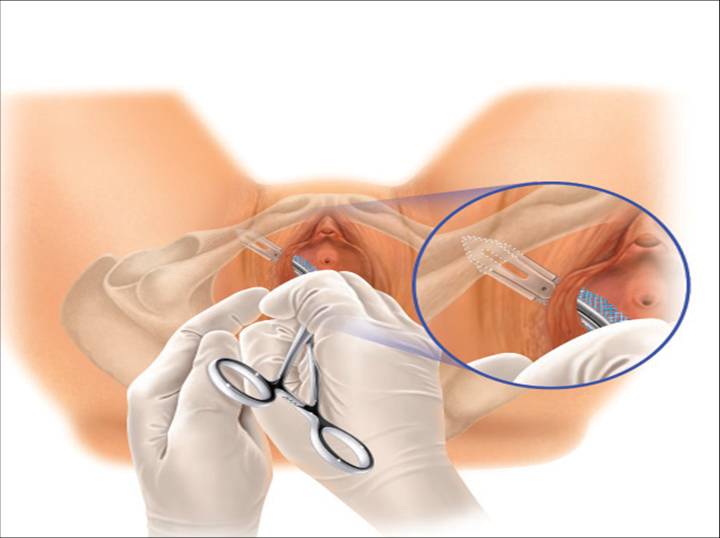
If a full-length sling is planned, the graft of choice is prepared and soaked in antibiotic solution. If an autologous fascial graft is planned, a harvesting procedure for either fascia lata or rectus fascia is completed using a Wilson fascial stripper or a vein stripper. Similarly, if an allograft is used, this too should be hydrated in an antibiotic solution. Generally, the graft should measure approximately 2 × 12–18 cm for a full-length sling, according to patient habitus. A transverse suprapubic incision is made 2 fingerbreadths superior to the symphysis pubis, measuring approximately 4 cm. The underlying rectus fascia should be exposed with either sharp or blunt dissection. The anterior vaginal epithelium is then infiltrated with either sterile saline or dilute anesthetic/epinephrine solution. A midline anterior vaginal incision is made, measuring about 3 cm, at the level of the urethrovesical junction. The vaginal epithelium is sharply dissected away from the periurethral and perivesical tissue. The dissection should be completed laterally to the inferior pubic rami. Gentle traction is applied to the Foley catheter to allow identification and palpation of the balloon, indicating the urethrovesical junction. The bladder is decompressed. With the surgeon protecting the urethra with the nondominant hand, the perineal membrane is perforated bilaterally, allowing entrance into the space of Retzius, using either Metzenbaum or curved Mayo scissors at a 45° angle, always lateral to the urethra and directly behind the symphysis pubis (Fig. 1). The midportion of the sling is secured using delayed, absorbable suture along the proximal urethra, with the most proximal edge at the bladder base to prevent folding or kinking of the graft material. As is done with a needle urethropexy, packing forceps are passed with guidance from a vaginal finger, from the abdominal incision through the space of Retzius to the vaginal incision. The graft arm is grasped and carried back through to the abdominal incision. This is repeated on the opposite side (Fig. 2). When passing through the space of Retzius, the surgeon takes care to start medial to the pubic tubercle to avoid ilioinguinal nerve injury. Once both sling arms are passed, urethrocystoscopy is performed to rule out urethral or vesical injury. Ureteral function is also confirmed by intravenous indigo carmine injection. A suprapubic catheter is placed under cystoscopic guidance for postoperative bladder drainage and voiding trials. The sling arms are then sutured to the rectus fascia using permanent suture to allow a urethrovesical junction angle of 0° with the horizontal plane. The incisions are irrigated with antibiotic solution. The vaginal and abdominal incisions are reapproximated using delayed, absorbable suture (Fig. 3).
Patch Sling
A variation of the full-length sling is the patch sling. This procedure can be performed with either a patch of in situ vagina, as described by Raz and associates in 1989,2 or other organic or inorganic grafts. The patch sling has been described as a variation of a Pereyra or Raz procedure.25 The patch should measure approximately 2 × 5 cm. Surgical preparation, the abdominal and vaginal incisions, and dissections are completed as described for the full-length sling. Entrance into the space of Retzius may or may not be accomplished, according to the surgeon's preference. As in the full-length sling procedure, the midportion of the patch graft is secured suburethrally using delayed, absorbable suture to prevent folding or kinking of the graft. In a helical fashion, permanent suture is passed along the long axis of the patch graft. A Stamey ligature carrier is passed with guidance from a vaginal finger, from the abdominal incision through the space of Retzius to the vaginal incision on each side for suture transfer. Once both suture arms have been transferred, urethrocystoscopy is performed after intravenous indigo carmine administration to rule out urethral, vesical, or ureteral injury. A suprapubic catheter is placed under cystoscopic guidance for postoperative bladder drainage and voiding trials. The suture arms are tied down to a urethrovesical junction angle of 0° with the horizontal plane. The incisions are irrigated with antibiotic solution. The vaginal and abdominal incisions are reapproximated using delayed, absorbable suture (see Fig. 3).
The full-length and patch sling procedures are most often performed under general anesthesia; however, if medically indicated, they may be completed under regional anesthesia.
Tension-Free Vaginal Tape Sling
The TVT system consists of a reusable stainless-steel introducer handle, a reusable rigid catheter guide, and the single-use device. The TVT device consists of a 1 × 40-cm ribbon of polypropylene mesh covered by a plastic sheath attached onto two curved stainless-steel needles (Fig. 4).
The TVT procedure is most often performed under local anesthesia with intravenous sedation. The procedure is performed with the patient in the dorsal lithotomy position with her lower extremities supported in Allen-type stirrups. An 18F Foley catheter is inserted to the urethra and the bladder is emptied. Local anesthetic is applied suprapubically at two points, 1–2 cm above the pubic symphysis and 2–3 cm lateral to the midline. The abdominal skin, underlying rectus muscle, and fascia, as well as the posterior aspect of the pubic bone, is infiltrated bilaterally. Two small abdominal skin incisions (0.5–1.0 cm) are then made at these points. No further abdominal dissection is necessary.
A Sims speculum is then inserted into the vagina to allow visualization of the anterior vaginal wall. The indwelling Foley bulb is used to identify the location of the internal urethral egress, while the external meatus is easily visualized. Using these two points as landmarks, the region of the midurethra is identified. The local anesthetic solution is injected into the vaginal submucosa in the midline and slightly lateral on each side of the urethra. Allis clamps are placed bilaterally for countertraction as a small sagittal incision (1.5 cm) is made in the midline at the level of midurethra. The incision should begin approximately 1 cm from the external urethral meatus. The Metzenbaum scissors are then used to minimally dissect the vaginal wall, freeing it from the underlying periurethral tissue and developing a small tunnel bilaterally. This dissection should be limited to a depth of 1–1.5 cm. Care should be taken not to puncture the pubocervical fascia or injure the urethra (Fig. 5). Additional local anesthetic solution should be injected bilaterally using a long spinal needle, placing the solution along the inferior and posterior aspects of the pubic symphysis.
The rigid catheter guide is then inserted into the Foley catheter. The handle of the rigid guide is then moved to the ipsilateral side of the anticipated passage of the forthcoming TVT needle. With the aid of the introducer handle, the surgeon places the tip of the needle into the previously developed periurethral tunnel (Fig. 6). Two hands are required to pass the needle safely. The needle is directed slightly laterally, most often in direct alignment with the patient's ipsilateral axilla. The TVT needle is gradually advanced by applying gentle pressure with the palm of the vaginal hand, with continued vaginal finger guidance and slight pressure from the second hand on the introducer handle. As the needle tip passes through the endopelvic fascia, a distinct drop in resistance is appreciated. At that point, with downward deflexion of the introducer handle, the surgeon guides the needle superiorly through the space of Retzius, with the needle being immediately opposed to the back side of the pubic symphysis (Fig. 7). As the needle opposes the underside of the rectus muscle and fascial sheath, resistance is again appreciated. At this point, the introducer handle is used solely to direct pressure anteriorly, advancing the needle tip through the previously made small abdominal incisions. The surgeon's nondominant hand is used suprapubically to help guide the needle tip (Fig. 8).
The rigid catheter guide and Foley catheter are removed and diagnostic urethrocystoscopy is performed to evaluate for any unintentional injury of the urethra or bladder. Once correct needle placement is confirmed, the needles pass completely through the abdominal incision. The steps of the procedure are then repeated on the opposite side. Care should be taken to ensure the tape is not twisted under the urethra (Fig. 9).
After correct placement of the TVT device and before removal of the protective plastic sheath, a cough test is performed to identify the correct positioning of the tape. The cough test is conducted with a full bladder (250–300 mL saline) (Fig. 10). Once the proper positioning of the tape is obtained, the plastic sheath is removed and the prolene mesh is left in place without tension under the midurethra. The abdominal ends of the tape are cut just below the skin surface. The procedure is completed with closure of the abdominal and vaginal incisions (Fig. 11).
TVT Obturator
The obturator sling consists of a disposable stainless steel trocar on a plastic handle in a spiral shape for passage around the inferior pubic ramus in through the obturator space. It incorporates the same mesh as the original TVT device (Fig. 12).
Again, this sling can be performed under local anesthesia with intravenous sedation and is performed with the patient in the dorsal lithotomy position. The dissection for placement is the key difference with the obturator approach. After the midline vaginal incision is made beneath the midurethral in the same fashion as that in using the TVT, the paraurethral dissection is performed 45 degrees from the midline just underneath the pubic rami on either side. Prior to insertion of the sling, markings are made on the inner thighs, either using the urethral as a landmark, or by palpation of the obturator foramen, in order to mark the anticiapted exit sites of the trocars. These sites are also infiltrated with local anesthetic prior to incision. A steel-winged guide allows easier and safer placement of the trocar tips into the paraurethral dissection tunnels and serves as a "shoe-horn" to keep the trocar in the desired space. A rigid catheter guide is not necessary as this sling does not enter the space of Retzius or come as close to the bladder during placement (Fig. 13).
After the tip of the trocar is inserted along the hollow of the winged guide, the tip is gently pushed inward along the path of the guide until a slight increase followed by a decrease in resistance is felt and the obturator membrane is perforated. The winged guide is then removed, and the handle of the device is carefully rotated and brought in a vertical fashion toward the midline, bringing the trocar tip to the level of the skin and toward the previously drawn skin mark (Fig. 14).
The metal trocar is then backed out leaving the plastic cannula with attached sling in place. The mesh is then pulled through the incision and the plastic cannula is cut and removed from the mesh. The same procedure is repeated on the second side. After initial placement, a cystoscopy and cough test may be performed with the sling slowly tightened on each side equally as desired. Once final placement is determined, either visually or by cough test, the mesh is stabilized using a hemostat or other device and the plastic sheaths covering the mesh tape can be removed bilaterally. The incisions are then closed accordingly (Fig. 15).
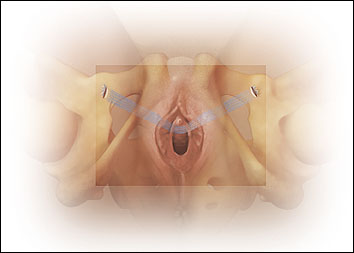 Fig. 15. The obturator tape lies in a "hammock" position 45 degrees away from the midline.
Fig. 15. The obturator tape lies in a "hammock" position 45 degrees away from the midline.
Single Incision Slings
TVT SECUR.
Like its predecessors, TVT and TVT Obturator (Ethicon, Somerville, NJ), TVT Secur is a polypropylene mesh or “tape.” The tape’s geometry is very different with TVT Secur than previous versions, measuring only 8 cm in length by 1 cm in width. Further, its edges are cut with a laser rather than a mechanical knife, thus thermally sealing the edges, which maintains its flat shape by preventing curling when force is applied. The ends of the mesh are laminated with Vicryl (Ethicon, Somerville, NJ) and polydioxanone fleece jackets that help secure the mesh in the target tissue so that the insertion devices can be backed out after final placement. TVT Secur allows the flexibility of placement in either a “U” (comparable to the retropubic sling approach) or “hammock” (comparable to TVT-O) configuration using the same instrument. Although similar sharp dissection techniques are required compared with predecessor slings, slightly larger paraurethral and vaginal incisions (~1.5 cm) must be made to accommodate the larger width of the device. The urogenital diaphragm, obturator internus muscle and obturator membrane should not be penetrated during sharp dissection because this may decrease the holding ability of the fixation tips. Likewise, care should be given not to overinfiltrate with local anesthetic into the target holding tissue, which may negatively affect pull-out force. A needle driver is used for stabilization while the surgeon’s thumb applies pressure during insertion. Cystoscopy is still recommended for both approaches; however, the manufacturer notes that cystoscopy is at the physician’s discretion for the hammock configuration (Fig. 16).
 Fig. 16. TVT Secur (Gynecare, Somerville, NJ)
Fig. 16. TVT Secur (Gynecare, Somerville, NJ)
The U configuration placement is most similar to the original TVT placement, with the tip of the device rotated about 45 degrees from the vertical midline. The flat tip of the device must be in direct and immediate contact with the back of the pubic bone while being pushed into the dense connective tissue of the urogenital diaphragm. A rigid catheter guide is recommended to shift the bladder and urethra to the opposite side during insertion (Fig. 17).
 Fig. 18. "Hammock" configuration
Fig. 18. "Hammock" configuration
This placement is identical to that of the obturator sling approach. The tip of the insertion device is tilted inward at a 45-degree angle from the sagittal midline as the tip is pushed just beneath the posterior edge of the inferior ischiopubic ramus and into the obturator internus muscle. Again, close contact with the bone is imperative during placement (Fig. 18).
Miniarc
The MiniArc uses a 2.3 mm needle separate from the mesh which has attached self-fixating tips different from that of TVT Secur. It also has an optional redocking feature giving the surgeon the opportunity for further intra-operative tensioning during placement if desired. Like its predecessors, MiniArc requires only a single, 1.5 cm vaginal incision and can be performed with local, spinal or general anesthesia. The permanent tips are placed just beyond the obturator membrane and hold the sling in place. The Miniarc has only one placement in the same fashion as the TVT Secur Hammock configuration, with the arms placed at a 45 degree angle off of the midline. However, desired placement is not into the obturator internus muscle, but just into the obturator membrane (Fig.19).
Fig. 19. Miniarc (American Medical Systems, Minnetonka, MN)
RESULTS
All of the above sling procedures have been successfully reported in patients with recurrent stress incontinence as well as patients with ISD. Cure rates for sling procedures vary from 70 to 100%.26, 2728, 29 Comparison of various sling case series is difficult, given the variation in surgical technique. However, two recent randomized studies noted that the success rates for the transobturator approach was not inferior to, nor significantly different from, the retropubic approach for synthetic mesh slings but both noted less incidence of cystotomy with the obturator approach.30, 31
GRAFT MATERIALS
The use of inorganic graft materials in gynecologic and urologic surgery has developed from the use of these materials in general surgical techniques such as herniorrhaphy and orthopedic repairs. Inorganic materials can be compared by their mechanical and biologic properties.
Chemical components of inorganic grafts include monofilament and multifilament types. Monofilaments include polypropylene (Marlex, Prolene, and Atrium). Multifilaments include polytetrafluoroethylene (Teflon), expanded polytetrafluoroethylene (Gore-tex), polyethylene terephthalate (Mersilene), polyglycolic acid (Dexon), and polyglactin 910 (Vicryl). Of the multifilaments, only two are absorbable (Dexon and Vicryl). One theoretical disadvantage of multifilament mesh is that its interstices may allow penetration by small bacteria (less than 1 μm), but not larger macrophages and polymorphonuclear leukocytes. The porosity of the mesh also contributes to the development of fibrous tissue. The number, size, and shape of the pores appear to be related to tissue-bonding. Mersilene is the most porous compared with Teflon and Marlex. Mesh flexibility is another property related to clinical outcome in that complications such as mesh extrusion may relate to the rigidity of the mesh.32 Currently, the length or amount of mesh placed is under consideration as seen with the new single-incision slings. Shorter mesh tapes may be desirable in decreasing the amount of human tissue, especially muscle fibers, that are traversed during mesh placement. Shorter mesh tapes may decrease post-operative pain in the short and long term as well as decrease intraoperative complications including bowel and bladder perforation, blood loss, and nerve and vessel injury.
Organic grafts can be autologous or heterologous. Autologous grafts require a separate harvesting procedure. Allografts and heterologous grafts can be purchased from various tissue banks. It is recommended that grafts be purchased from accredited tissue banks. The American Association of Tissue Banks inspects the bank to ensure high-quality tissue production. Autologous grafts used include various muscles, rectus fascia, and fascia lata. Allografts include dermis, dura, pericardium, and fascia lata. Heterologous grafts include porcine small intestine submucosa (SIS) and porcine dermal collagen (Pelvicol). Alloderm is an acellular, freeze-dried, human dermal graft. Fascia lata grafts are available as either solvent-dehydrated, gamma-irradiated (Tutoplast) or freeze-dried (FasLata). Pericardium is available as a solvent-dehydrated, gamma-irradiated graft (Tutoplast).
Graft materials vary in mechanical and biologic properties. These properties are associated with a variety of success and complication rates when used in anti-incontinence surgery. Without randomized comparison studies, the decision remains with the surgeon. It is therefore of utmost importance that the surgeon be familiar with these graft materials and their properties.
COMPLICATIONS
The complications associated with sling procedures can be categorized as those common to anti-incontinence surgery (transvaginal or retropubic) and those specific to the sling technique.
Complications common to anti-incontinence surgery include injury to the bladder, urethra, or ureter, retropubic or vaginal hematoma, wound infection, cystitis, nerve damage, and recurrent or persistent urinary incontinence. The use of urethrocystoscopy at the time of sling procedures can aid in identifying intraoperative lower urinary tract injury, therefore allowing immediate attention and repair of the injury. Intraoperative hemorrhage and hematoma formation should be prevented by meticulous surgical technique. Knowledge and attention to surgical anatomy, as well as experience with the technique, are essential for avoidance and management of vascular injury. Nerve damage may occur secondary to positioning for abdominal or vaginal surgery. Injury is commonly due to compression or stretch of the nerve fibers but may also be secondary to direct transection. Attention to intraoperative positioning and surgical technique, along with early recognition and evaluation of any postoperative complaints, is recommended to avoid injury. Persistent or recurrent urinary incontinence can occur due to surgical failure, de novo or persistent detrusor instability, overflow incontinence, or fistula formation. This complication should be addressed with a thorough workup and appropriate treatment.
Complications specific to the sling procedure include voiding dysfunction and urinary retention, detrusor instability, and graft erosion and infection. Voiding dysfunction and urinary retention are associated with the level of tension of the sling and resultant outlet obstruction. Many techniques are used during surgery for sling adjustment, but no one method is recommended, and the selection remains a matter of the surgeon's experience. Rates of persistent urinary retention have been reported to be 2–10%.13, 26, 33 Symptomatic de novo postoperative detrusor instability is thought to be related to the degree of outflow obstruction. Reported rates vary from 2 to 22%.13 Graft erosion and infection have been reported with an increased incidence associated with inorganic materials. Due to the increased incidence of graft erosion and infection with inorganic materials, there has been a trend toward the use of organic grafts. Organic grafts, however, are not free from similar complications.
CONCLUSION
Few randomized controlled trials exist comparing sling procedures with colposuspensions.34 One prominent trial demonstrated increased success with fascial slings versus the Burch colposuspension and began to change our opinion regarding the gold standard treatment for SUI.35 With mesh slings having been utilized for over 13 years, more long-term data on efficacy are available suggesting sustained dryness rates over time.36 The use of mesh slings has changed the treatment of SUI significantly by creating a minimally invasive approach that can be performed on an outpatient basis. The new single-incision slings further challenge this approach by offering the potential for an-office based procedure that, potentially, is associated with fewer complications.
Variation exists with regard to surgical technique, graft material, and success and complication rates for the suburethral sling procedure. Despite this variation, the suburethral sling procedure is an effective, safe technique for the treatment of GSI and ISD and continues to evolve.
REFERENCES
Aldridge AH: Transplantation of fascia for the relief of urinary stress incontinence. Am J Obstet Gynecol 44: 398, 1942 |
|
Raz S, Siegel AL, Short JL, Synder JA: Vaginal wall sling. J Urol 141: 43, 1989 |
|
Kohli N, Karram MM: Surgery for genuine stress incontinence. In: Urogynecology and Reconstructive Pelvic Surgery, 2nd edn, p 178. St. Louis, Mosby, 1999 |
|
Williams TJ, TeLinde RW: The sling operation for urinary incontinence using Mersilene ribbon. Obstet Gynecol 19: 241, 1962 |
|
Stanton SL, Brindley GS, Holmes DM: Silastic sling for urethral sphincter incompetence in women. Br J Obstet Gynecol 92: 747, 1985 |
|
Horbach NS, Blanco JS, Ostergard DR et al: A suburethral sling with polytetrafluoroethylene for the treatment of genuine stress incontinence in patients with low closure pressure. Obstet Gynecol 71: 648, 1988 |
|
Ulmsten U, Petros P: Intravaginal slingplasty (IVS): An ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 29: 75, 1995 |
|
Ulmsten U, Henriksson L, Johnson P, Varhos G: An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol 7: 81, 1996 |
|
Dietz HP, Vancaillie P, Svehla M et al: Mechanical properties of implant materials used in incontinence surgery [abstract 98]. 31st Annual Meeting of the International Continence Society, Seoul, Korea, 2001 |
|
Urinary Incontinence in Adults Guideline Update Panel. Urinary Incontinence in Adults: Acute and Chronic Management, Clinical Practice Guideline. AHCPR Pub No. 96-0682. Agency for Health Care Policy and Research, Public Health Service, U.S. Dept. of Health and Human Services, March 1996 |
|
International Continence Society Committee on Standardization of Terminology. The standardization of terminology of lower urinary tract function. Scand J Urol 114: 5, 1988 |
|
McGuire EJ, Lytton B, Pepe V, Kohorn EJ: Stress urinary incontinence. Obstet Gynecol 47: 255, 1976 |
|
Swift SE: Intrinsic urethral sphincter deficiency. In: Urogynecology and Urodynamics, Theory and Practice, 4th edn, p 151. Baltimore, Williams & Wilkins, 1996 |
|
Horbach NS: Suburethral sling procedures. In: Urogynecology and Urodynamics, Theory and Practice, 4th edn, p 570. Baltimore, Williams & Wilkins, 1996 |
|
McGuire EJ: Urodynamic findings in patients after failure of stress incontinence operations. Prog Clin Biol Res 78: 351, 1981 |
|
Hilton P, Stanton SL: Urethral pressure measurement by microtransducer: The results in symptom-free women and in those with genuine stress incontinence. Br J Obstet Gynaecol 90: 919, 1983 |
|
Sand PK, Bowen LW, Panganiban R, Ostergard DR: The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol 69: 399, 1987 |
|
Horbach NS, Ostergard DR: Predicting intrinsic urethral sphincter dysfunction in women with stress urinary incontinence. Obstet Gynecol 84: 188, 1994 |
|
Swift SE, Ostergard DR: A comparison of stress leak-point pressure and maximum urethral closure pressure in patients with genuine stress incontinence. Obstet Gynecol 85: 704, 1995 |
|
McLennan MT, Bent AE: Supine empty stress test as a predictor of low valsalva leak point pressure. Neurourol Urodynam 17: 121, 1998 |
|
Hsu THS, Rackley RR, Appell RA: The supine stress test: a simple method to detect intrinsic urethral sphincter dysfunction. J Urol 162: 460, 1999 |
|
Bump RC, Coates KW, Cundiff GW et al: Diagnosing intrinsic sphincteric deficiency: comparing urethral closure pressure, urethral axis, and Valsalva leak point pressures. Am J Obstet Gynecol 177: 303, 1997 |
|
Jeon MJ, Jung HJ, Chung SM et al: Comparison of the treatment outcome of pubovaginal sling, tension-free vaginal tape, and transobturator tape for stress urinary incontinence with intrinsic sphincter deficiency. Am J Obstet Gynecol. 2008 Jul;199(1):76.e1-4. Epub 2008 Jan 25. |
|
Viereck V, Nebel M, Bader W et al: Role of bladder neck mobility and urethral closure pressure in predicting outcome. Ultrasound Obstet Gynecol 2006 Aug;28(2):214-20. |
|
Jeon MJ, Jung HJ, Chung SM et al: Comparison of the treatment outcome of pubovaginal sling, tension-free vaginaltape, and transobturator tape for stress urinary incontinence with intrinsicsphincter deficiency. Am J Obstet Gynecol. 2008 Jul;199(1):76.e1-4. Epub 2008 Jan 25. |
|
Karram MM, Bhatia NN: Patch procedure: Modified transvaginal fascia lata sling for recurrent or severe stress urinary incontinence. Obstet Gynecol 75: 461, 1990 |
|
Sarver R, Govier FE: Pubovaginal slings: Past, present, and future. Int Urogynecol J 8: 358, 1997 |
|
Haab F, Zimmern PE, Leach GE: Female stress urinary incontinence due to intrinsic sphincteric deficiency: Recognition and management. J Urol 156: 3, 1996 |
|
Neuman M: Perioperative complications and early follow-up with 100 TVT-SECUR procedures. J Minim Invasive Gynecol. 2008 Jul-Aug;15(4):480-4. Epub 2008 Jun 9. |
|
Debodinance P, Lagrange E, Amblard J et al: [TVT Secur: more and more minimally invasive. Preliminary prospective study of110 cases] J Gynecol Obstet Biol Reprod (Paris). 2008 May;37(3):229-36. Epub 2008 Mar 17. |
|
Barber MD, Kleeman S, Karram MM et al: Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2008 Mar;111(3):611-21. |
|
Barry C, Lim YN, Muller R et al: A multi-centre, randomised clinical control trial comparing the retropubic (RP)sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Feb;19(2):171-8. Epub 2007 Jul 19. |
|
Iglesia CB, Fenner DE, Brubaker L: The use of mesh in gynecologic surgery. Int Urogynecol J 8: 105, 1997 |
|
Ghoniem GM, Shaaban A: Suburethral slings for treatment of stress urinary incontinence. Int Urogynecol J 5: 228, 1994 |
|
McGuire W: Women's health: Stress incontinence. Clin Evidence 5: 1352, 2001 |
|
Albo ME, Richter HE, Brubaker L et al: Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007 May 24;356(21):2143-55. Epub 2007 May 21. |
|
Liapis A, Bakas P, Creatsas G: Long-term efficacy of tension-free vaginal tape in the management of stress. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Nov;19(11):1509-12. Epub 2008 Jun |