This chapter should be cited as follows:
Swer M, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.413923
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 11
Labor and delivery
Volume Editor: Dr Edwin Chandraharan, Director Global Academy of Medical Education and Training, London, UK
Chapter
Clinical Assessment of Labor Progress
First published: February 2021
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
The process of labor occurs with the onset of regular contractions causing progressive cervical effacement and dilatation, leading to the descent of the fetus in the pelvis and eventual delivery. The ability of the fetus to successfully negotiate the pelvis during labor and delivery depends on the complex interactions of four variables: uterine activity, the fetus, the maternal pelvis and maternal wellbeing. This is also known as the four Ps: power, passage, passenger and psyche.
Progress has been charted on labor curves which have developed over time to accommodate changes in obstetric practice. Clinical assessment through the use of vaginal examination, abdominal palpation, and the use of the partogram have been traditionally used. More recent assessment tools have included ultrasound and amniotic fluid lactate level. These measures have helped to identify normal progress, aid in identifying abnormalities in labor progress and commence appropriate management.
NORMAL LABOR PROGRESSION
Stages and phases of labor
Conventionally, labor is defined by three stages and their phases:
First stage is from the onset of regular painful contractions associated with descent of the presenting part and progressive dilatation of the cervix until the cervix is fully dilated (10 cm). This consists of the latent phase (in which there is gradual cervical change) and the active phase (more rapid change).
Second stage is from full dilatation of the cervix up to the birth of the singleton baby or the last baby in a multiple pregnancy. At the start of the second stage, the fetal presenting part may or may not be fully engaged (meaning that the widest diameter has passed through the pelvic brim), and the woman may or may not have the urge to push. When pushing is delayed to allow descent, this is known as the passive phase. The active phase refers to the beginning of active pushing till birth of the baby.
Third stage is from the birth of the baby until expulsion of the placenta and membranes.
A 'fourth stage' is sometimes added in midwifery teaching, also termed 'immediate postpartum care', which represents the period of a few hours after expulsion of the placenta when close observation is desirable to avoid or detect postpartum hemorrhage, signs of sepsis or hypertension. During this period, close mother–baby contact is maintained and breastfeeding is initiated.
Four Ps (power, passenger, passage and psyche)
Progress in labor is determined by assessing the four following components, also known as the four Ps:
Power
The power refers to the strength of the uterine contractions as well as maternal expulsive efforts in the second stage of labor. This is assessed via abdominal palpation. Contractions leading to normal progress should be regular, frequent, lasting more than 60 s and leading to cervical effacement.
Passenger
This refers to the fetus and assessment of the size, position and attitude (relationship of the fetal parts to one another). There is also a need for an awareness of any underlying conditions that may lead to concerns with progress.
Passage
The structure of the bony pelvis needs to be considered together with soft tissue factors such as the presence of a full bladder or rectum, any space-occupying masses or presence of vaginal septa. The adequacy of the pelvis can be assessed only during labor.
Psyche
This takes into consideration the emotional state of the mother during her labor which can also have an overall effect on progress of labor. Factors to consider are levels of stress and underlying anxiety during the process and also whether there is adequate support from a birthing partner present, as well as ensuring the woman is in a welcoming and supportive environment.
Charting the progress of labor
Friedman’s curve
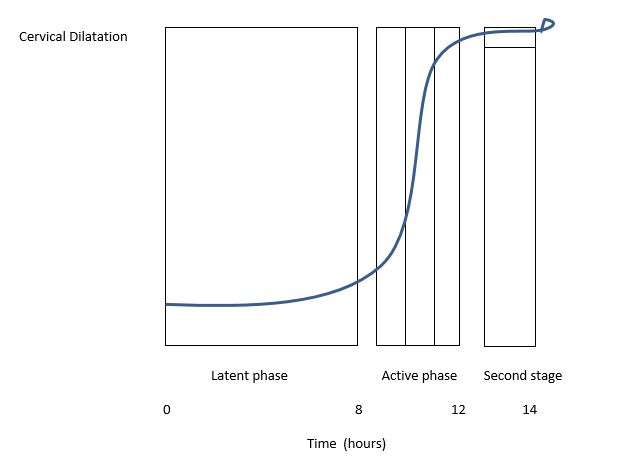
Traditionally, the criteria for labor progression have been based on the research undertaken by Friedman in the 1950s. This was centered on an evaluation of 500 nulliparous and 500 parous women. Friedman showed that looking at changes in cervical dilatation and fetal station over time were the most useful parameters for assessing labor progress.1,2 Based on these data, he formulated a 'labor curve' that has been widely adopted and used internationally over the past 60 years (Figure 1).
The labor curve indicated a slower rate of cervical dilatation in the first stage of labor to 3–4 cm (latent phase). The transition from the latent phase to the active phase of first stage of labor, occurring at 3–4 cm dilatation, led to an accelerated rate of dilatation of 1.2 cm/h for nulliparous women and 1.5 cm/h for parous women. The curve then noted a deceleration phase around 9 cm. The second stage of labor (at 10 cm) was defined to be prolonged if it was more than 2.5 hours in nulliparas and 1 hour in parous women.
1
Demonstration of average dilatation and progress in labor as demonstrated by Friedman et al. (1978).3
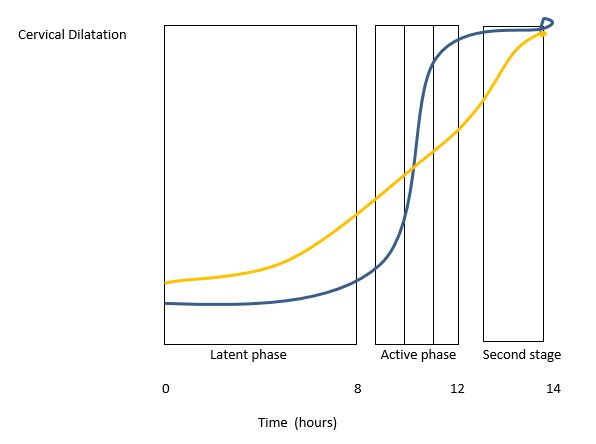
Zhang’s curve
In 2002, Zhang et al. presented a new labor curve that was based on data from 1329 low-risk women and later confirmed in a large cohort of 26,838 women in 2010 (Figure 2).4,5 Both curves demonstrate an increase in the rate of cervical dilatation as labor progresses. However, Zhang’s labor curve differs in the length of the active phase of the first stage of labor. Zhang’s data showed that the cervix dilated substantially slower in the active phase with a mean of 5.5 hours from 4 to 10 cm compared to 2.5 hours under the Friedman curve. There is also no distinct deflection of the curve between 9 and 10 cm (deceleration phase) compared to Friedman’s curve. Zhang’s evaluation of labor progress shows that, before 6 cm there is a shallower slope in the rate of dilatation, but after 6 cm the rate of dilatation is more rapid. This highlights that there is a longer duration of the first stage of labor with a slower rate of cervical change between 3 and 6 cm.
2
Comparison of Friedman et al.‘s labor progression curve (blue) vs Zhang’s labor progression curve (yellow), as demonstrated by Zhang et al. 2002.4
The contemporary curve of Zhang was influenced by changes in patient characteristics, anesthesia practices as well as more up-to-date obstetric practices. As a result, the physiologic pattern for normal labor progress has been revised and been acknowledged as the following, in keeping with modern obstetric practice: 'The active phase of the first stage of labor commences at 5–6 cm with the rate of dilatation being 0.5 cm/h until the second stage is achieved'.6
The Labour Progression Study (LaPS), a randomized controlled trial carried out in Norway comparing labor outcome in women managed with a partograph on the Friedman data compared with the Zhang data, showed no differences in intrapartum cesarean section rates and adverse outcomes7. This study was well designed but, in view of the low cesarean section rate and low BMI of the women in the study, it was felt that findings could not be generalized to the overall population. What it did identify is that a knowledge of labor progression is important to understand how to manage better an actual prolonged labor and decrease unnecessary interventions.7
The criteria for normal labor progression are a controversial issue, but it has been recognized by the International Federation of Gynecology and Obstetrics (FIGO) as the active phase of the first stage of labor commencing at 5–6 cm and that dilatation can be 0.5 cm/h.
Progress of labor with induction
Considering the revised criteria for labor progression, it should be borne in mind that the first stage of labor in women undergoing induction is longer than that in spontaneous labor. This was especially seen in the latent phase where a retrospective study looking at both nulliparous and parous women showed a significantly longer latent phase in those undergoing induction compared to those with spontaneous onset of labor..8 However, the active phase (i.e. from 6 to 10 cm) was the same in both types of labor as was the second stage.
ABNORMAL LABOR PROGRESSION
Types of abnormal labor progression
Approximately 20% of all labors ending in a live birth are involved in either protraction or an arrest in progression..9 In low-resource countries, abnormal labor progression due to labor dystocia is associated with significant maternal and neonatal morbidity. It is also the most common reason for primary cesarean delivery. It is therefore important to have an understanding of what constitutes abnormal labor progress and assess it appropriately.
The types of abnormal progression that can occur are defined according to the phases and stages of labor at which it occurs:
Prolonged latent phase of first stage
There is no uniformly accepted definition for a prolonged latent phase due to the difficulty in diagnosing the exact transition of latent to active phase of labor. It had been defined by Friedman as a nullipara who has not entered the active phase 20 h after the onset of the latent phase and a parous woman who has not entered the active phase 14 h after the onset of the latent phase..10 However, more contemporary data by Zhang have shown that many women with latent phases longer than the upper limit described by Friedman go on to have a normal active phase and vaginal delivery.5 In women with induction whose latent phase is longer, caution should be exercised in diagnosing a prolonged latent phase.
Assessment of the latent phase of labor should ideally occur away from the delivery suite and women should be offered analgesia, rest and observation during this stage especially if they are not coping well in this phase.
Arrest in latent phase of first stage
This is not considered a clinical diagnosis and management with cesarean section should not be considered in women in this phase when laboring spontaneously. Clinical assessment of the need of amniotomy and/or use of oxytocin can be considered.
Prolonged active phase of first stage
A dilatation of less than 1–2 cm/h after a woman reaches the active phase (≥6 cm) is considered a delay in progress of labor. In such cases, an assessment for amniotomy and oxytocin is reasonable with a meta-analysis showing a reduction in time to delivery by 1.5 h.11
Arrest in active phase of first stage
Active phase arrest is diagnosed at cervical dilatation ≥6 cm in a patient with ruptured membranes where there is:
- No cervical change for ≥4 h despite adequate contractions;
- No cervical change for ≥6 h with inadequate contractions.12
This definition, as proposed by the USA National Institute of Child Health and Development (NICHD), Society for Maternal-Fetal Medicine (SMFM) and American College of Obstetricians and Gynecologists (ACOG), takes into account the use of oxytocin for augmentation when safely indicated.
Prolonged second stage of labor
The maximum amount of time allowed for diagnosis of second stage of labor is still not clearly defined largely due to the impact of deciding optimal intervention for operative delivery as well as risks of second stage cesarean section if indicated.
As mentioned above, Freidman’s data supported a prolonged second stage as more than 2.5 h for nulliparous and 1 h for parous women. In order to reduce unnecessary intervention, these time limits have been agreed to be lengthened with the following recommendations, provided maternal and fetal conditions are optimal:12
- Nulliparous: 4 h of second stage or 3 h of active pushing;
- Parous: 3 h of second stage or 2 h of active pushing.
However, assessment is especially important since it is thought to be reasonable to diagnose arrest sooner if there is no descent with effective pushing and the probability of a vaginal delivery is low when considering other factors (maternal and fetal).
Risk factors
There are a number of factors that need to be taken into consideration that contribute to an abnormal labor progression. These are associated with one or more of the four Ps mentioned above.
Power
Hypocontractile activity – this refers to the lack of strength and/or coordination of uterine activity to not allow optimal dilatation of the cervix and delivery of the fetus. It is the most common risk factor in explaining labor dystocia.
Passenger
- Non-occipitoanterior position – the fetus usually enters the pelvis in an occipital transverse (OT) or occiput posterior (OP) position before rotating to occipitoanterior (OA) prior to delivery. When the rotation is protracted or does not occur, this leads to malposition which is associated with a prolonged second stage;
- Fetal anomaly;
- Macrosomia.
The above features can contribute to cephalopelvic disproportion in which there is a disproportion between the fetus and the maternal bony pelvis. Cephalopelvic disproportion is a subjective clinical assessment that is made at the time of labor. True cephalopelvic disproportion does not refer to malposition, but instead reflects any known anomaly or size that may lead to the disproportion.
Passage
- Obesity – this is associated with an increased length of the first stage of labor, but there has been no correlation with the second stage.
- Pelvic adequacy can be assessed only at the time of labor progression, although signs of a narrow pubic arch or prominent spines or sacrum can lead to abnormal labor progress.
- Other maternal features include short stature, longer cervical length at mid pregnancy, and post-term pregnancy.
- Uterine features:
- Bandl’s ring – occurs in 1 in 5000 births and refers to a constriction forming between the lower and upper segments of the uterus that leads to labor dystocia in the second stage. Diagnosis is made at time of cesarean section.
- Uterine abnormality.
Psyche
- Women experiencing increased pain or high levels of anxiety release catecholamines, which can have an inhibitory effect on uterine contractility leading to abnormal labor progression. For this reason, adequate analgesia as well as proper emotional support is important in ensuring adequate progress.
- As a consequence, offering regional anesthesia should be guided by a person’s wishes taking into consideration other factors such as parity and previous fast labor, and not dependent on cervical dilatation. Avoiding regional anesthesia to potentially reduce labor abnormalities is not recommended.
Clinical assessment tools
Labor progress is assessed through a number of tools as mentioned below. The most commonly used and tested are a thorough vaginal and abdominal examination and the use of the partograph. More up-to-date means of assessment are also discussed.
Vaginal examination
Vaginal examination should take into consideration the cervical dilatation, effacement and station of fetal head. It is important that an abdominal examination is carried out at the same time to assess how many fifths palpable the presenting part is in relation to the pelvic brim. These findings should always be documented clearly.
Cervical dilatation ranges from closed to 10 cm when no cervix is present (full dilatation). A rough guide is 1 cm is equal to a single index finger. Effacement refers to the remaining length of the cervix and is documented in cm or percentage remaining. 100% usually refers to 2 cm length (not in labor). The station of the fetal head is in reference to the plane of the maternal ischial spines with the leading part of the head at this level referred to as station 0. This is important especially in active labor and at full dilatation in order to assess appropriate intervention if indicated. Caput and molding should be taken into account.
Vaginal examinations should be performed for the following indications:
- On admission in labor;
- 4-hourly in the first stage (2-hourly after amniotomy);
- Prior to administering analgesia;
- Patient urge to push;
- Any concern with fetal heart rate (to rule out cord prolapse, uterine rupture or fetal descent).
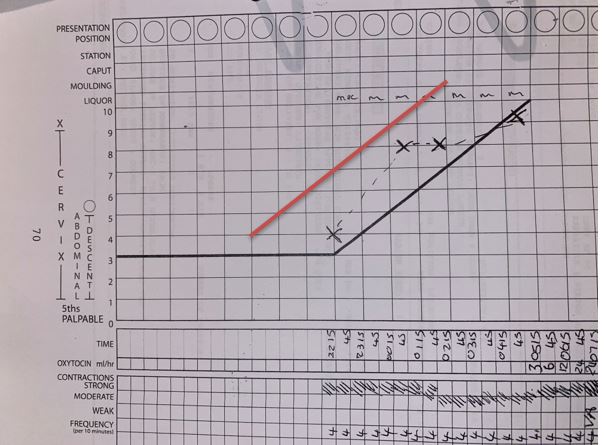
Partogram
The partogram is a graphical representation of observations made regarding progress of labor in the active phase (Figure 3).13The aim is to provide a pictorial overview of the patient's cervical dilatation over time in comparison with the expected lower limit of normal progress. This is done by looking at a number of observations including cervical dilatation, descent of fetal head and uterine contractions, as well as fetal heart rate, presence of membranes and color of amniotic fluid if rupture has occurred, and molding. The partogram is thought to be useful in alerting clinicians to deviations from normal progress or fetal wellbeing. This is through the use of alert and action lines highlighting when action needs to be taken or transfer to appropriate facilities should occur.
3
An example of a partogram used in the UK showing alert and action lines.
Although useful for visualizing labor progress, routine use of partograms has not been proven to significantly improve obstetric outcome. A Cochrane review in 2018 confirmed this and showed that no specific partograph has been proven to be superior to others in comparative trials.14
Ultrasound
Although not widely used clinically, intrapartum ultrasound examination has been shown to be a more precise and reproducible assessment tool than vaginal examination. Transabdominal ultrasound can be used for assessment of fetal lie and position in the axial and sagittal planes. Landmarks used are fetal orbits (occiput posterior position), cervical spine and occiput (occiput anterior position) and the midline cerebral echo (occiput transverse).15
Transperineal ultrasound can be used for assessment of fetal station in the mid-sagittal or axial plane. One technique is to measure the angle between the symphysis pubis and the leading part of the fetal skull (called the angle of progression) which is then correlated to head station in cm from −3 cm to +5 cm using an algorithm.16 Another measurement used is the head-to-perineum distance (HPD) which represents the part of the birth canal yet to be passed. However, the HPD measurement does not account for the curvature of the birth canal. Midline angle (MLA) is useful for looking at the angle of head rotation which can also be an indicator of progress.
Ultrasound assessment can be used to provide more precise assessment of fetal position and station which can be useful for assessing suspected abnormal labor progress, and is also useful in predicting outcome of operative vaginal delivery. However, at present, it has not been shown to improve overall management of labor and delivery, so its use is dependent on the expertise and equipment available in individual settings .17
Amniotic fluid lactate
Lactate plays an important role in uterine activity and pathophysiological processes of labor. The uterus is highly glycolytic, primarily because repeated transient hypoxia is a normal feature of labor, which results in lactate production even under normoxic conditions. Studies show a significant correlation between lactate production, hypoxia and the effect of oxytocin.18 This is an important interaction if labor is to end normally.
A close correlation has been described between lactate produced by the uterus and the level of lactate in amniotic fluid. Studies have shown that high levels of amniotic fluid are noted in labor with abnormal progress compared to normal progressing labors.
A recent study has been developed to look at levels of amniotic fluid collected at the vaginal introitus and analyzed on the delivery suite. The results have shown that higher levels of amniotic fluid were more likely to be associated with longer and increased complications in labor (i.e. need for intervention).19 A new, non-invasive method has been developed that makes it possible to detect the amniotic fluid level in a small sample of amniotic fluid collected from the vaginal pouch and analyzed at the bedside in the delivery room. Levels of amniotic fluid can be measured immediately and a result provided. This is especially useful in the cases in which oxytocin is used to augment labor and the amniotic fluid levels can help predict the success of labor especially in those showing signs of abnormal progression. This is still a relatively new assessment tool, but it is important to consider for future routine use, especially in conjunction with oxytocin.
CONCLUSION
An understanding of what a proper clinical assessment of labor progress entails is essential in ensuring the best maternal and neonatal outcomes. It is important to have a good foundation as to what constitutes a normal progress of labor by identifying correctly various stages and phases, and understanding of the factors that lead to progress. It is especially important to be aware of recent criteria for assessment of progress of labor which have taken into consideration new patient cohorts and changes in obstetric practice in the past 40 years.
An understanding of normal labor progress also helps to identify better when abnormal labor progression is occurring. This is especially important in order to ensure that appropriate intervention is used in a timely and appropriate manner. The tools discussed above are important to be used to give a thorough clinical assessment of labor progress. Most of all it is important to look at labor progress in a holistic fashion with an awareness of all the factors involved and full consideration of them especially when making a diagnosis of labor dystocia.
PRACTICE RECOMMENDATIONS
- Labor is conventionally defined by three stages. The first stage is the progressive dilatation to 10 cm (fully). The second stage is from full dilatation to birth. The third stage is from birth of the baby to expulsion of the placenta. A fourth stage is sometimes identified and refers to the immediate postpartum period after expulsion of the placenta.
- The criteria for active and latent phases of the first stage of labor have changed over the past 40 years. It is now recognized that the active phase of the first stage of labor commences at 5–6 cm with normal dilatation occurring at 0.5 cm/h.
- Progress in labor is determined by the assessment of four components (four Ps):
- Power (strength of uterine contractions);
- Passenger (size and position of the fetus);
- Passage (awareness of adequacy of the pelvis);
- Psyche (emotional state of the mother during labor).
- An arrest in the active phase of the first stage is when there is no cervical change for ≥4 hours despite adequate contractions or ≥6 hours with inadequate contractions despite use of oxytocin if safely indicated.
- A prolonged second stage in nulliparous women is 4 hours or 3 hours of active pushing. In parous women, it is 3 hours or 2 hours of active pushing.
- Clinical assessment tools traditionally include digital vaginal examination with abdominal palpation and the use of the partogram. Intrapartum ultrasound (either transabdominal or transperineal) is another assessment tool, which is particularly beneficial prior to operative vaginal delivery. There is also a role developing for the use of amniotic fluid lactate levels to determine abnormal labor progress.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Friedman EA. The graphic analysis of labor. Am J Obstet Gynecol 1954;68:1568–75. | |
Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol 1955;6:567–89. | |
Friedman EA. Labor: Clinical Evaluation and Management, 2nd edn. New York: Appleton-Century-Crofts, 1978. | |
Zhang J, Troendle J, Yancey MK. Reassessing the labor curve in nulliparous women. Am J Obstet Gynecol 2002;187:824–8. | |
Zhang J, Troendle J, Mikolajczyk R, et al. The natural history of the normal 1st stage of labor. Obstet Gynecol 2010;115:705–10. | |
Zhang J, Duan T. The physiologic pattern of normal labour progression. BJOG 2018;125:955. | |
Bernitz S, Dalbye R, Zhang J, et al. The frequency of intrapartum caesarean section use with the WHO partograph versus Zhang's guideline in the Labour Progression Study (LaPS): a multicentre, cluster-randomised controlled trial. Lancet 2019;393:340 | |
Harper LM, Caughey AB, Odibo AO, et al. Normal progress of induced labor. Obstet Gynecol 2012;119:1113. | |
Zhu BP, Grigorescu V, Le T, et al. Labor dystocia and its association with interpregnancy interval. Am J Obstet Gynecol 2006;195:121. | |
Friedman EA. The Labor Curve. Clin Perinatol 1981;8(1):15-25. | |
Wei SQ, Luo ZC, Xu H, Fraser WD. The effect of early oxytocin augmentation in labor: a meta-analysis. Obstet Gynecol 2009;114:641. | |
Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol 2012;120:1181. | |
The WHO partograph. World Health Organization (2008) Managing Prolonged and Obstructed Labour. | |
Lavender T, Cuthbert A, Smyth RM. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev 2018;8:CD005461. | |
Youssef A, Bellussi F, Montaguti E, et al. Agreement between two- and three-dimensional methods for the assessment of the fetal head-symphysis distance in active labor. Ultrasound Obstet Gynecol 2014;43:183–8. | |
Tutschek B, Braun T, Chantraine F, et al. A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. BJOG 2011;118:62. | |
ISUOG practice guideline. Intrapartum ultrasound. Ultrasound Obstet Gynecol 2018;52:128–39. | |
Murphy M, Butler M, Coughlan B, et al. Elevated amniotic fluid lactate predicts labor disorders and cesarean delivery in nulliparous women at term. Am J Obstet Gynecol 2015;213(5):673 e1-8 | |
Wiberg-Itzel E, Pembe AB, Järnbert-Pettersson H, et al. Lactate in Amniotic Fluid: Predictor of Labor Outcome in Oxytocin-Augmented Primiparas' Deliveries. PLoS One 2016;11:1-13. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards programme CLICK HERE)