This chapter should be cited as follows:
Vasireddy A, Johns J, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.413703
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 4
Fetal development and maternal adaptation
Volume Editor: Professor Asma Khalil, The Royal College of Obstetricians and Gynaecologists, London, UK; Fetal Medicine Unit, Department of Obstetrics and Gynaecology, St George’s University Hospitals NHS Foundation Trust, London, UK
Chapter
Early Pregnancy Failure and Miscarriage
First published: February 2021
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
Miscarriage is the most common complication encountered in early pregnancy – it is estimated that one in four women will experience a miscarriage in their lifetime and the majority of losses will be in the first trimester. The risk of miscarriage increases with maternal age reflecting the age of the ovum and its chromosomes. Clinicians who encounter women in early pregnancy, either via an acute admission through the emergency department or as an outpatient in the early pregnancy unit, must have a good grasp of basic embryology and physiology to enable identification of abnormal pathology and arrange appropriate care. Ectopic pregnancy is becoming increasingly more common and recognition and appropriate treatment is vital to reduce the risk of associated morbidity and mortality. This chapter gives a succinct overview of the basic principles, clinical care of women in early pregnancy and management of complications.
BASICS OF PHYSIOLOGY AND EMBRYOLOGY IN EARLY PREGNANCY
When women seek medical care in early pregnancy one of the first questions asked by the attending clinician is “when was the first day of the last period”. The date of the last menstrual period (LMP) is used to estimate where in embryological development the pregnancy should have reached and allows relevant interpretation of the early pregnancy ultrasound scan. Where the last menstrual period is not known, the ultrasound scan is used to date the pregnancy by measurement of the crown–rump length.
With reference to a regular 28-day cycle, where ovulation occurs on day 14, a home pregnancy test will be positive usually a few days before a missed period. In a longer menstrual cycles, the day of ovulation is usually later and must be corrected for according to the cycle length, in order to accurately assess a pregnancy. Most urinary pregnancy tests detect βhCG levels above 25 IU/L. Following ovulation, the corpus luteum releases progesterone, which sustains the pregnancy until the fetomaternal circulation is developed later in the first trimester and the placenta takes over.
With modern ultrasound technology, a transvaginal scan should demonstrate a normal intrauterine pregnancy from approximately 4 weeks' gestation from the LMP and an understanding of the sonographic landmarks is important for accurate assessment. Viability can usually be confirmed when a normal embryo is present at approximately 6 weeks' gestation. Embryological development and early pregnancy landmarks are shown in Figure 1.
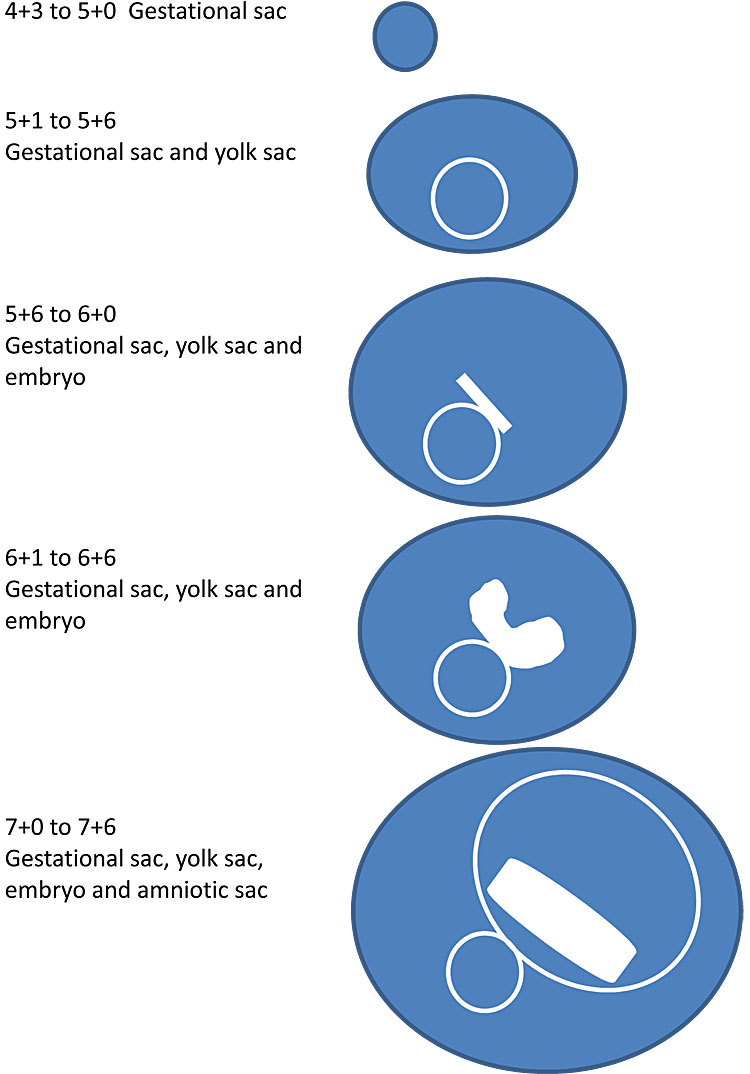
1
Embryological development and early pregnancy landmarks.1
BASIC PRINCIPLES OF ASSESSMENT OF THE EARLY PREGNANCY PATIENT
Clinical assessment – history taking
When assessing a woman in early pregnancy, the basics of history taking and examination are essential. Most women present to the early pregnancy unit (EPU) or emergency department (ED) with a history of vaginal bleeding or lower abdominal pain. Details regarding the symptoms, amount of bleeding, duration, relation to LMP (and cycle length), site of pain and other symptoms are useful in planning immediate management and decision-making. Women who have experienced a complete miscarriage may describe symptoms of bleeding with lower abdominal period-like pain that peaked and quickly resolved or those with a threatened miscarriage may describe painless heavy bleeding.
In addition to the medical history (Table 1), questions regarding the current pregnancy, such as whether it is an unplanned or planned pregnancy must be asked sensitively to enable appropriate follow up care or contraception. A full gynecological and obstetric, medical and surgical history must also be taken. Clues within the history can help determine the presence of risk factors for early pregnancy complications such as history of recurrent miscarriage or previous pelvic surgery.
1
History-taking questions.
History–taking in early pregnancy | |
Presenting symptoms | Bleeding Abdominal pain Other |
Current pregnancy related | Last menstrual period Unplanned/planned and intention Spontaneous or assisted conception |
Gynecological history | Menstrual cycle Cervical smear history Previous gynecological diagnosis Previous gynecological surgery Other surgery |
Obstetric history | Previous live births Mode of delivery Previous miscarriage Previous ectopic Previous termination |
Medical history | Diabetes Hypertension Other Allergies |
Social history | Smoking status Alcohol status |
Clinical assessment – examination
All women attending with symptoms of bleeding or pain via the ED should already have had a basic assessment of cardiovascular status with observations of blood pressure, heart rate, oxygen saturation, respiratory rate and temperature on arrival. In women who attend early pregnancy units and are generally well and mobile without significant symptoms, routine observations need not necessarily be performed.
In a woman who presents unwell to the ED, clinical examination should include an abdominal examination to assess for pain or peritonism and in some cases a speculum examination to assess bleeding, take swabs if sepsis is suspected, and to see whether there is pregnancy tissue in the cervix. Products of conception seen in the external cervical os can be removed with sponge forceps and must always be confirmed via histological analysis. A digital examination adds little useful information in these women and, therefore, should be avoided. The findings of the examination and vital signs can be used to determine whether a woman can be discharged with a follow up scan arranged in the early pregnancy unit or whether she needs admission for urgent treatment. Bloods tests for full blood count, clotting screen and group and save should be taken depending on the severity of the bleeding. Anti-D should be arranged in line with national guidelines. Serum βhCG and progesterone is of little value in the initial assessment of early pregnancy problems, prior to ultrasound and should only usually be taken in the context of a pregnancy of unknown location or ectopic pregnancy where they can help determine management.
Early pregnancy ultrasound
In the assessment of early pregnancy, a transvaginal scan (TVS) is the gold standard as it provides higher resolution images and better identification of normal or abnormal pathology and is acceptable to most women. Scans are usually performed on stable women to establish the location and viability of the pregnancy. Most research evidence and guidelines are based on assessment with a TVS and cannot be extrapolated to transabdominal assessment. If a patient declines a TVS, it should be explained that a transabdominal (TAS) scan may not be able to provide as accurate an assessment and may be more likely to result in an inconclusive outcome. Where TAS findings are inconclusive or in the context of abnormal pathology, a follow up TAS or a TVS should be recommended to confirm the diagnosis.
In all early pregnancy scans, the location and viability of the pregnancy is key in both establishing a diagnosis and guiding further management (Table 2). As part of the scan, the gynecological organs (uterus, cervix, ovaries) are visualized systematically and this assessment should never be forgotten. Assessment of the early pregnancy should only be made once the pelvic anatomy has been assessed. Other gynecological pathology such as fibroids or ovarian cysts can also be visualized and assessed. Depending on the findings of the scan, the pregnancy can be accurately dated by crown–rump length (CRL). If there is a mismatch between expected gestation by LMP and the scan findings by more than 7 days in an ongoing pregnancy then it should be re-dated by the measurement of the CRL or a follow up scan may be offered to assess the pregnancy further if uncertainty remains. It is not the scope of this chapter to discuss early pregnancy ultrasound assessment in further detail.
2
Information required from an ultrasound scan in early pregnancy.
Basic information required from ultrasound scan report | |
Route | Transvaginal Transabdominal Other |
Early pregnancy assessment | Location of the pregnancy Gestational sac measurement Yolk sac Amniotic sac Embryo Fetal heart rate |
Maternal structures | Uterus (size, position) Uterine anomalies Right ovary (size, morphology, presence of corpus luteum) Left ovary (size, morphology, presence of corpus luteum) Pouch of Douglas (presence of fluid) |
Other investigations
Blood tests for full blood count or cross match are necessary for the woman who is actively bleeding and/or hemodynamically unstable. Routine full blood count is unnecessary for all other women unless clinically indicated. As previously mentioned blood tests for βhCG and progesterone are not useful unless performed as part of the workup following a diagnosis of a pregnancy of unknown location or an ectopic pregnancy.
EARLY PREGNANCY FAILURE AND MISCARRIAGE
Miscarriage is defined as a pregnancy loss before the time that a fetus can survive independently. In general, this is defined as a pregnancy loss under 24 weeks. WHO defines miscarriage as the expulsion or extraction of an embryo or fetus weighing 500 g or less.2
Definitions
Early embryonic demise or missed miscarriage
- Early embryonic demise or missed miscarriage refers to a pregnancy where the embryo has formed but has stopped growing early in its development, therefore never having reached viability, or initially appears to grow normally with a fetal heartbeat that stops later on in the first trimester. Terms such as anembryonic pregnancy and blighted ovum are outdated and inaccurate and should no longer be used.
- The etiology of miscarriage is multifactorial. The commonest cause of first trimester miscarriage is sporadic chromosomal abnormalities. Factors associated with miscarriage include increasing maternal or paternal age, maternal medical conditions (e.g. poorly controlled diabetes), previous miscarriages and sociodemographic factors.
Recurrent miscarriage
- Recurrent miscarriage refers to the loss of three or more consecutive pregnancies before 24 weeks. This affects 1–2% of couples.3 The etiology of first trimester and second trimester recurrent miscarriage is different (Table 3). Management is based on the underlying cause. A detailed discussion is outside the scope of this chapter.
3
Evidence-based investigation and management of recurrent miscarriage.
Underlying causes of recurrent miscarriage | Investigation | Treatment |
Congenital uterine malformations | Two- or three-dimensional scan Magnetic resonance imaging/hysteroscopy/laparoscopy if required | No specific treatment Insufficient evidence to assess uterine septum resection |
Chromosomal abnormalities of pregnancy | Karyotyping of miscarriage tissue +/− parental genetic bloods to assess for parenteral chromosome rearrangements | Genetic counseling Preimplantation genetic diagnosis Egg/sperm donation – alternative options |
Inherited thrombophilia | Bloods tests for factor V Leiden, prothrombin gene mutation, protein S deficiency | Consider heparin |
Antiphospholipid syndrome | Bloods tests for lupus anticoagulant, beta-2-glycoprotein, cardiolipin antibodies | Consider low-dose aspirin and heparin |
Incomplete miscarriage
- This is a scan diagnosis based on findings of heterogeneous tissue distorting the midline with or without a vascular supply following a history of pain and bleeding in a woman who has previously had an intrauterine pregnancy demonstrated on ultrasound. The finding of tissue with typical trophoblastic flow on power Doppler can be highly suggestive of an incomplete miscarriage in women who have not previously had a scan demonstrating an intrauterine pregnancy, but is not currently diagnostic – “pregnancy of unknown location” protocols must be followed in these circumstances.
Complete miscarriage
- A diagnosis of complete miscarriage is an easy one to make when a patient has already had an intrauterine pregnancy demonstrated on a previous scan. The subsequent symptoms experienced by the woman will preempt the diagnosis with an empty uterus on scan. In women who are seen for the first time and who give a typical history of a complete miscarriage (cramping pain and heavy bleeding with passing of tissue), it is important not to assume that the absence of a pregnancy on scan confirms the diagnosis – in this circumstance, women should be managed as a pregnancy of unknown location and followed up according to local protocols with bloods taken for βhCG and progesterone.4
Threatened miscarriage
- A threatened miscarriage refers to ongoing vaginal bleeding in the presence of a viable intrauterine pregnancy on ultrasound and occurs in 15–20% of ongoing pregnancies. Advise the patient to ensure that they seek emergency services or attend the early pregnancy unit should the bleeding become heavy.
ULTRASOUND DIAGNOSIS OF MISCARRIAGE
It is important to understand what is normal in embryological development before performing a scan in early pregnancy as described earlier in this chapter. After a systematic TVS documenting measurements of the pregnancy and comparing this with diagnostic criteria as published by NICE, a diagnosis of miscarriage can be made (Table 4).5
4
NICE miscarriage diagnosis criteria.
Mode of scanning | Ultrasound markers | Second opinion | Diagnosis confirmed | Follow up scan required |
Transvaginal ultrasound | CRL (crown–rump length) is 7 mm or more and no visible heartbeat OR Mean gestational sac diameter 25 mm or more and no visible fetal pole | Yes to confirm non-viable pregnancy | Yes – early embryonic demise | Optional if no second opinion or diagnosis uncertain then rescan in 1 week before confirming diagnosis |
Transvaginal ultrasound | CRL (crown–rump length) is less than 7 mm and no visible heartbeat OR Mean gestational sac diameter less than 25 mm and no visible fetal pole | Not needed as requires a follow up scan | No – needs follow up scan | Rescan in 1 week (minimum interval) Further scans may be required before confirming a diagnosis |
Transabdominal ultrasound | CRL (crown–rump length) is 7 mm or more and no visible heartbeat OR Mean gestational sac diameter 25 mm or more and no visible fetal pole | Not needed as requires a follow up scan | No – needs follow up scan | Rescan in 2 weeks to confirm the diagnosis |
Prior to scanning women, it is important to explain the nature and purpose of the scan assessment of the pelvic organs and the pregnancy, and to manage expectations.
Following the scan, time should be spent explaining the diagnosis in simple terms – the diagnostic terms early intrauterine pregnancy or pregnancy of uncertain viability can be used in medical paperwork where viability cannot be confirmed, however, these technical terms will need explaining to the woman.
It is important to explain clearly to women that a diagnosis cannot always be made during the first visit. Many women require follow up scans to confirm viability or to confirm the diagnosis of a miscarriage (Figure 2). Some women may find the uncertainty difficult to manage, therefore, it is important that an explanation is given clearly and honestly describing the limitations of one ultrasound scan. Always give safety netting advice for women waiting for reassessment and ask them to return to the early pregnancy unit or emergency department should they experience very heavy bleeding or severe pain.
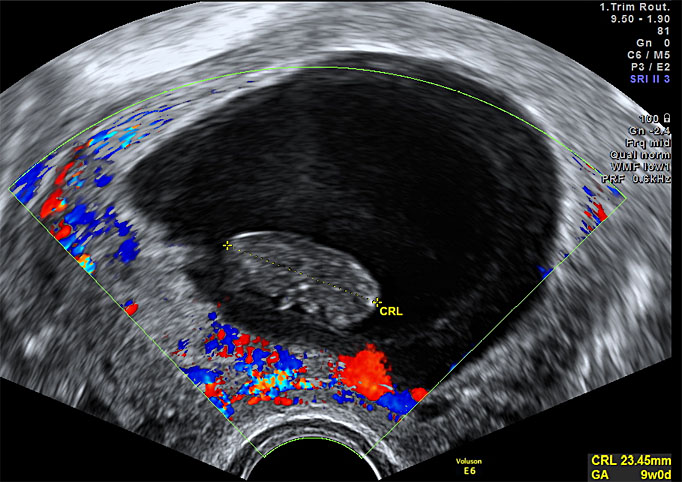
2
Ultrasound of early embryonic demise.
DISCUSSING DIAGNOSIS
Miscarriage is a sensitive matter and time should be taken to explain to the patient the diagnosis and what this means for the current pregnancy and the future. It is important not to make assumptions about how the patient might feel about the diagnosis based on whether the pregnancy was planned or even if the patient initially was seeking a termination. Remember to use lay terms avoiding jargon and leave enough time for questions. Some women may need to have more time to process the information; therefore, reschedule a second visit to discuss further management. Keep the woman at the center of care and do not rush her to make a decision. Ensure she is well informed about what to expect, such as the symptoms of spontaneous miscarriage, and give her a point of contact in case of any questions. For women who are finding the diagnosis difficult to accept or process, offer them a second scan a week later for further confirmation or referral to a psychologist or counselor if available. Resources such as the Miscarriage Association provide useful information regarding good practice points when speaking to women with miscarriage.6
MANAGEMENT OF MISCARRIAGE
Miscarriage can be managed with expectant, medical and surgical treatment. In 2012, NICE guidance was updated with the recommendation that expectant management should be offered as first line treatment as it is as successful and avoids intervention (Table 5).5 The guidance goes on to explain that other options can be explored if the woman is at risk of bleeding (either at late gestations or in the context of a bleeding disorder), infection or does not wish to have expectant management. In practice, all options should be discussed and women should be given the opportunity to choose which management fits with their personal preference as well as social factors such as work and childcare.
The MIST trial published in 2006 was a large randomized controlled trial comparing expectant and medical management with surgery – the primary outcomes were the incidence of infection and the need for unplanned admission and surgical intervention.7 The results showed that the overall risk of infection was low (2–3%) in all management groups. Emergency admissions were significantly higher in the expectant and medical groups than after surgery.
5
NICE guidance for the management of miscarriage.
Expectant management | Medical management | Surgical management |
First line | Second line
| Second line
|
Give oral and written information regarding what to expect | Give oral and written information regarding what to expect | Give oral and written information regarding what to expect |
If bleeding/pain stopped during 7–14 days of expectant management then advise woman to perform pregnancy test in 3 weeks to confirm this is negative | Vaginal misoprostol – can offer oral if patient prefers Single dose of 800 μg misoprostol for missed miscarriage Single dose of 600 μg for incomplete miscarriage | Arrange manual vacuum aspiration under local anesthetic in outpatient clinic setting |
Review patient at 7–14 day who are persistently bleeding or patient with a positive pregnancy test at 3 weeks – individualize care | Advise women regarding what symptoms to expect Advise women to perform urine pregnancy test at 3 weeks | Arrange surgical management in a theater under general anesthetic |
Offer repeat scan if after the period of expectant management bleeding or pain has not yet started (spontaneous process not before) | Advise women with positive pregnancy test after three weeks or worsening symptoms to return for review |
Expectant management
Expectant management is the process of allowing up to 2 weeks from diagnosis of a missed or incomplete miscarriage for the woman to be given the chance to miscarry spontaneously. This timeframe can be extended beyond 2 weeks if the woman prefers this option, provided she is well. If she does not experience any symptoms within 2 weeks from diagnosis or if she has persistent bleeding at 2 weeks then she should be advised to see an early pregnancy specialist to discuss alternative modes of treatment. Expectant management is usually recommended with a diagnosis of incomplete miscarriage as the symptoms have already started. Success rates vary in the literature and local audit of outcomes for all modes of management should guide counseling.
Women should be advised of the risk of heavy bleeding, emergency admission and the risk of surgical intervention. A Cochrane review revealed women opting for expectant management versus planned surgical management had an increased rate of incomplete miscarriage at 2 weeks (RR 3.98), unplanned surgery (RR 7.35), increased days of bleeding and risk of blood transfusion (RR 6.45).8 Women should also be advised regarding analgesia use and to use sanitary towels rather than tampons whilst they are bleeding.
In those women who do miscarry spontaneously, a home pregnancy test is usually performed a week following resolution of miscarriage symptoms to ensure that this is negative. A positive test can indicate persistent pregnancy tissue. Following on from a negative pregnancy test, periods usually resume after 4–6 weeks after which the woman can try to conceive should she wish to do so.
Medical management
Misoprostol is a synthetic prostaglandin analog. It is used in the management of both early and late miscarriage as well as part of the regimen together with mifepristone (an anti-progestogen drug) in medical termination procedures. Misoprostol is used to bring on the onset of miscarriage symptoms – both cramps and bleeding usually within 24 hours of administration. The route of administration can vary based on local unit practices (oral or vaginal). Success rates vary in the literature and can be up to 85% successful. Women must be counseled similarly to expectant management – symptoms can last up to 2 weeks, risk of bleeding, infection and risk of emergency surgery. Simple analgesics are usually sufficient to provide symptom relief, although occasionally some women may require opiate based medications such as codeine for pain management. No routine follow up is required however patients must be advised to seek medical attention if symptoms persist for longer than 2 weeks or if they have a positive pregnancy test 3 weeks after medical management.
Current NICE guidance states that misoprostol alone is effective in the treatment of miscarriage; however, recent research and ongoing trials are assessing whether mifepristone in conjunction with misoprostol leads to more successful outcomes.9
Surgical management
Surgical management with dilatation and suction curettage is the most common method of management of miscarriage worldwide. The procedure can be performed either under general anesthesia with a rigid suction curette or under local anesthesia with a manual vacuum aspiration kit (MVA). Misoprostol can be used pre-operatively to prime the cervix in nulliparous patients. Ultrasound should be used intraoperatively whenever possible to confirm removal of miscarriage tissue as well to enable gentle guidance of instruments into the cavity under direct vision and without undue pressure, reducing the risk of uterine perforation.
Common risks include bleeding, infection and retained products of conception (3–5%) requiring repeat surgery. Serious risks associated with surgery include uterine perforation (5 : 1000), trauma to the cervix or intrauterine adhesion formation impacting future fertility (Asherman’s syndrome is rare, however, the general pooled prevalence of adhesions after miscarriage is up to 20%, although the significance of this is not known).10 Surgical management can be useful in women who have experienced recurrent miscarriage and choose to have tissue karyotyping as it enables optimal collection of pregnancy tissue. It is also the procedure of choice in women who are bleeding heavily, hemodynamically unstable or where sepsis or molar pregnancy are suspected. The surgery is a short procedure lasting up to 20 minutes usually and patients are safe to be discharged from the hospital the same day. Routine administration of syntocinon or postoperative full blood count is not necessary unless significant blood loss has occurred or is anticipated. Anti D immunoglobulin is given to all rhesus negative women postprocedure.
Other circumstances: pregnancy of unknown location
A pregnancy of unknown location (PUL) is a diagnosis in women with a positive pregnancy test and no scan evidence of an intrauterine or extrauterine pregnancy. The clinical history in some cases can point towards the correct diagnosis – such as very heavy bleeding with clots and cramps, which subsequently resolves in a complete miscarriage. A PUL will be the result of one of three possible scenarios:
- It is too early to see the pregnancy;
- It is too late and the pregnancy has already failed (regardless of its location);
- The pregnancy cannot be found, i.e. it is an ectopic that has been missed or an intrauterine pregnancy in an anomalous uterus, e.g. uterine anomaly or fibroids.
A hospital’s PUL rate can be a useful indicator of scan quality and should be regularly audited and reviewed.
For safe management blood tests for βhCG and progesterone are taken to guide further follow up – specific “PUL” protocols are used to guide ongoing assessment and management.4 Women with blood tests reflecting a resolving pregnancy must also be told that it cannot be known with certainty whether this was a failed intrauterine pregnancy or a failed extrauterine pregnancy.
ECTOPIC PREGNANCY
An ectopic pregnancy occurs when the fertilized egg implants outside of the uterine cavity – this occurs in up to 1–3% of pregnancies depending on the patient population.11 There are numerous risk factors for an ectopic pregnancy; however, ectopic pregnancies can also arise in their absence. Over 90% of ectopic pregnancies are located in the Fallopian tube (Table 6). Less commonly ectopic pregnancies can be found in the interstitial portion of the fallopian tube, rudimentary horns in an anomalous uterus (cornual), ovary, abdomen, cervix, myometrium and cesarean scar. These special cases of ectopic pregnancy are outside of the scope of this chapter.
6
Risk factors for ectopic pregnancy.
Risks factors for ectopic pregnancy |
Previous ectopic pregnancy Contraceptive-related factors
Fertility-related factors
Other risk factors
|
Symptoms and signs
Common symptoms of an ectopic pregnancy include localized pain and light bleeding or spotting. Other symptoms, such as gastrointestinal disturbance, are also common. Irritation of the peritoneum, from blood in the abdominal cavity in a ruptured ectopic pregnancy, can lead to shoulder tip pain, collapse and altered bowel function. Signs of an ectopic pregnancy that may be elicited during the clinical examination include localized tenderness. Rebound tenderness and guarding may be present in those with hemoperitoneum. On internal vaginal examination, there may be cervical excitation and adnexal tenderness; however, these signs are fairly non-specific and vaginal examination rarely adds to the assessment of ectopic pregnancy.
In the clinically stable patient with an unruptured ectopic pregnancy, all observations for blood pressure and pulse may be normal. In those that are bleeding internally, signs such as tachycardia, hypotension and increased respiratory rate may be present; however, in young healthy women these can be rather late signs and a high index of suspicion is required. Patients who are clinically stable and have mild symptoms can await investigation with a TVS. Patient who are hemodynamically unstable or with severe symptoms must be resuscitated appropriately and have definitive management. Intravenous access, fluid resuscitation and blood tests for crossmatch and full blood count must be arranged in those who are unwell. Surgical treatment must not be delayed in these compromised patients by waiting for an ultrasound scan.
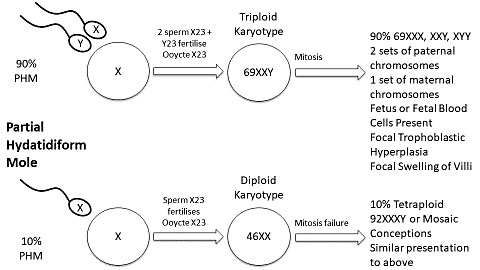
Ultrasound findings
Transvaginal ultrasound is the gold standard for diagnosis of an ectopic pregnancy. The ultrasound appearance of an ectopic pregnancy can vary: inhomogeneous conglomerate mass, echogenic-ringed vascular structure (“bagel sign”) with visible gestational sac with or without a yolk sac or an embryo with no fetal heart action, or an embryo with heart action (a “live ectopic”). Other findings can include an intact midline endometrial echo or pseudosac (anechoic fluid in the midline of the endometrial cavity) and hemoperitoneum (free fluid of low level echogenicity in the pouch of Douglas). Transvaginal scan is highly sensitive in identifying most tubal ectopic pregnancies at the first scan (Figure 3).12
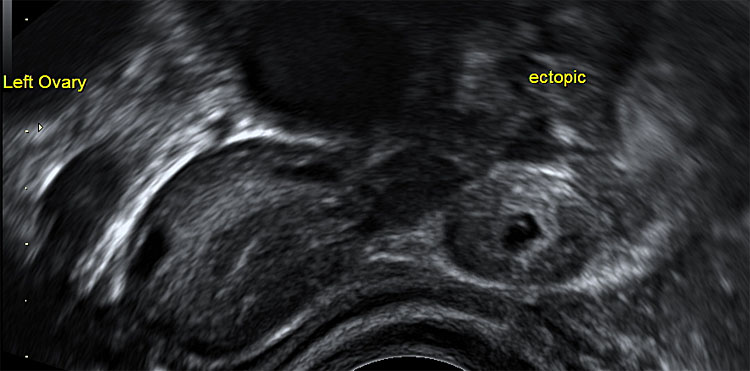
3
Ultrasound of a tubal ectopic pregnancy.
Explaining the diagnosis
It is important that a clear explanation of the diagnosis is given to all women. Written information including diagrams if necessary must also be provided. Reproductive outcomes for future pregnancies must be discussed ensuring that the woman understands that she is at increased risk of an ectopic pregnancy in the future – these women require an early scan in the next pregnancy to confirm location. Women who do not wish to become pregnant again soon, should be offered appropriate contraception once the ectopic has been treated.
Treatment of an ectopic pregnancy
Treatment of an ectopic pregnancy must be guided first and foremost by how clinically unwell the woman is. If hemodynamically compromised, then surgical treatment is the best option to remove the ectopic pregnancy and stop the bleeding. In women who are asymptomatic or have mild symptoms and are clinically well, then all treatment options can be discussed. As recommended in the NICE guidance, a blood test taken for βhCG can help in guiding management.5 Women must be made aware that for expectant and medical management of ectopic pregnancy, they will need to be compliant and attend for potentially prolonged follow up.
Expectant management
One-third of women with an ectopic pregnancy can be managed without intervention.13 Expectant management is a suitable option for women with relatively low βhCG levels (less than 1500 IU/liter in our population) and minimal symptoms. Regular monitoring of βhCG levels to ensure a downward trend until negative confirms successful expectant management. Research has shown that medical management should not be routinely used in these women as the success is no greater than for expectant management.14
Medical management
Methotrexate is a folate antagonist which inhibits synthesis of purines and pyrimidines therefore interfering with cell proliferation. The RCOG recommend that systemic methotrexate (a chemotherapy agent given intramuscularly as a single dose 50 mg/m2) can be used in suitable women with an ectopic pregnancy – the guidance stipulates that methotrexate should not be given at the first visit unless absolutely certain of the diagnosis and only if an intrauterine pregnancy has been excluded.11 It should also not be given in women with a falling βhCG.
NICE guidance recommends that methotrexate can be offered to women who are able to return for regular follow up, do not have significant pain, have an unruptured ectopic with an adnexal mass smaller than 35 mm and no heartbeat, a serum βhCG of less than 1500 IU/liter and no intrauterine pregnancy. It can also be considered in cases where the βhCG is between 1500 and 5000 IU/liter.5
The woman must provide written consent to the injection as it also comes with adverse risks which include: photosensitivity, rash, abdominal pain, stomatitis, conjunctivitis, gastrointestinal disturbance, renal/liver/bone marrow dysfunction, risk of failure, and a high risk of teratogenicity in the next pregnancy if conception occurs within 3 months of the injection. Patients who opt for medical management must have regular blood tests for full blood count, renal and liver profile and βhCG on the day of the injection, day 4 and day 7. If the βhCG falls between day 4 and day 7 by 15% then it confirms the methotrexate is working; however, weekly monitoring must continue until negative. If at any point the βhCG plateaus or rises then the woman must be reassessed and managed accordingly. A second injection can be considered.
Surgical management
In women who are unable to come for regular blood test monitoring, surgery may be the best option. It is also recommended in cases where the βhCG is over 5000 IU/liter or where there is a “live” ectopic and in unstable women or those with a hemoperitoneum on ultrasound. A woman may also choose surgical management and this choice should be respected provided adequate counseling is provided. The laparoscopic approach is recommended over the open approach in the majority of cases and salpingectomy is preferred over salpingotomy where the contralateral tube is healthy as there is no significant difference in fertility outcomes.11 In women with fertility-reducing factors, a salpingotomy may be considered – in these cases women must be informed of the risk of persistent trophoblastic disease and the need for ongoing monitoring with blood tests for βhCG and the potential need for subsequent methotrexate or salpingectomy. Women should be counseled that there is an up to 5% negative histology rate that will require further follow up of βhCG levels and reassessment.15 Women should also be informed of future pregnancy outcomes depending on mode of management (Table 7).16
7
Outcomes following ectopic pregnancy.
Outcomes in presence of healthy contralateral tube | ||
Mode of management | Salpingotomy | Salpingectomy |
Ongoing pregnancy | 60.7% | 56.2% |
Persistent trophoblast | 7% | <1% |
Repeat ectopic | 8% | 5% |
GESTATIONAL TROPHOBLASTIC DISEASE
Molar pregnancy with a complete or partial hydatidiform mole arises as a consequence of an abnormal amount of genetic material within the fertilized ovum – complete moles arise from an empty ovum which has been fertilized by a duplicated single sperm; a partial mole arises from a triploid pregnancy where an egg is fertilized by two spermatozoon (Figure 4). Gestational trophoblastic disease includes molar pregnancy, choriocarcinoma and placental site trophoblastic tumors. The risk of progression to gestational trophoblastic neoplasia (GTN) is 15% after a complete molar pregnancy and 0.5% after a partial molar pregnancy.17
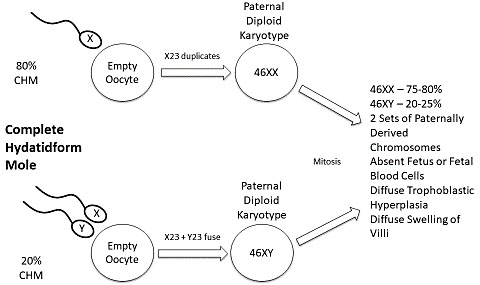
4
The genetics of complete and partial molar pregnancy. From Graham and Johns, 2017,18 with permission.
Symptoms and signs
Women with molar pregnancy typically present with heavy or irregular bleeding, hyperemesis, excessive uterine enlargement and an early non-viable pregnancy. Risk factors for gestational trophoblastic disease include extremes of reproductive age, previous molar pregnancy and ethnicity.17 The incidence in Europe and North America is approximately 0.2–1.5/1000 live births. The incidence has been reported to be higher in Asia and Africa.
Ultrasound diagnostic features
Ultrasound can be used to identify those with a suspected molar pregnancy; detection rates for partial molar pregnancy is in the range of 20–30% compared with a complete molar pregnancy detection rate of 57–95%.19,20 A definitive diagnosis can only be made with histological examination of the products of conception. On scan there may be a cystic mass with the classical “snow storm” appearance. One retrospective study has shown that the ultrasound features of a molar pregnancy differ with gestation – polypoidal tissue at 5–7 weeks and hydropic villous tissue from 8 weeks (Figure 5).21 The diagnosis is not always clear on scan as a molar pregnancy may appear similar to a hydropic miscarriage.
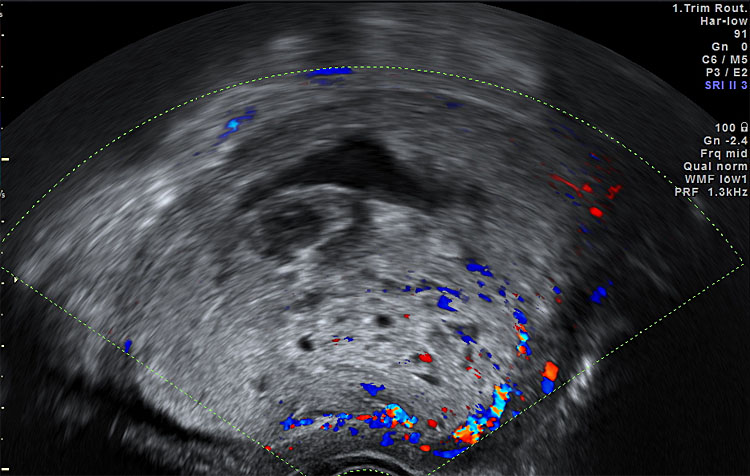
5
Ultrasound of a complete molar pregnancy.
Management
There is guidance from the RCOG detailing how best to manage suspected gestational trophoblast disease.17 Surgical management is the recommended treatment of a molar pregnancy and products of conception should be sent for histological analysis. Medical treatment of a molar pregnancy should be avoided as there is a potential risk of dissemination of trophoblastic tissue and histological diagnosis may not be possible. The use of oxytocin should be avoided; however, should there be significant hemorrhage then the risks/benefits should be assessed and it should be used accordingly. If the histopathology is confirmatory then in the UK women are referred to their nearest specialist gestational trophoblast disease center for βhCG follow up and treatment if required.
Gestational trophoblastic neoplasia
Gestational trophoblastic neoplasia (GTN) can occur after any pregnancy event – the need for chemotherapy is determined following FIGO staging. The risk of GTN is low once the βhCG has normalized following a molar pregnancy.
USE OF PROPHYLACTIC ANTI D IMMUNOGLOBULIN
Anti D IgG prophylaxis is used to reduce the risk of hemolytic disease of the newborn. With reference to early pregnancy, it should be given to all women who experience bleeding close to or after 12 weeks' gestation or if she has surgical management of miscarriage at any gestation or surgery for an ectopic pregnancy (Table 8). Routine Kleihauer testing is not required and a standard dose of Anti D IgG is sufficient for adequate prophylaxis.22 Women may decline administration of the injection if the blood group of their partner is known and he is also rhesus negative.
8
Use of anti D immunoglobulin (Ig).
Sensitizing events prior to 12 weeks | Anti D Required and dose |
Termination of pregnancy
| 250 IU minimum dose prophylactic anti D Ig within 72 hours of event if previously non-sensitized (BSH 201422) |
Ectopic pregnancy
| 250 IU minimum dose prophylactic anti D Ig within 72 hours of event if previously non-sensitized (NICE 20195, RCOG 2016,11) |
Molar pregnancy | 250 IU minimum dose prophylactic anti D Ig within 72 hours of event if previously non-sensitized (BSH 201422) |
Miscarriage
| 250 IU minimum dose prophylactic anti D Ig within 72 hours of event if previously non-sensitized (NICE 20195) |
Other
| 250 IU minimum dose prophylactic anti D Ig within 72 hours of event if previously non-sensitized (BSH 201422) |
PRACTICE RECOMMENDATIONS
- In early pregnancy, clear communication both verbal and written is key. Detailed explanation of scan findings and further management is important taking in to account the woman own circumstances and dealing with these issues sensitively with appropriate language.
- Early pregnancy diagnoses can be challenging for the clinician and confusing for the patient – explaining that repeat scans or blood tests are required to enable accurate diagnose and treatment is important.
- Follow local and national standardized protocols and ensure that senior advice has been sought before arranging either medical or surgical management of an ectopic pregnancy.
- Counsel women regarding future pregnancies and outcomes where possible.
CONFLICTS OF INTEREST
Author(s) statement awaited.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Jurkovic D et al. Ultrasound features of normal early pregnancy development. Current Opinion in Obstetrics and Gynaecology 1995;7:493–504. | |
World Health Organization, UNICEF, United Nations Population Fund. Vaginal bleeding in early pregnancy. In: Managing complications in pregnancy and childbirth: a guide for midwives and doctors, 2nd edn, 2017 [internet publication]. | |
Royal College of Obstetricians and Gynaecologists. The Investigation and Treatment of Couples with Recurrent First trimester and Second-trimester Miscarriage Green-top Guideline No. 17, 2011. | |
Ross JA. Diagnostic protocols for the management of pregnancy of unknown location. 2019;126(2):199. DOI: 10.1111/1471–0528.15441. Epub 2018 Sep 20. | |
National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guideline NG126, 2019 April [internet publication]. | |
Information for health professionals. Films and Good Practice Guides. Miscarriage Association. miscarriageassociation.org.uk. | |
Trinder J et al. MIST Management of miscarriage: expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial). BMJ 2006;332(7552):1235–40. | |
Nanda K et al. Expectant care versus surgical treatment for miscarriage. Cochrane Database of Systematic Reviews 2012;Issue 3. Art. No.: CD003518. DOI: 10.1002/14651858.CD003518.pub3. | |
Schreiber CA et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med 2018;378(23):2161–70. DOI: 10.1056/NEJMoa1715726. | |
Hooker AB et al. Systematic review and meta-analysis of intrauterine adhesions after miscarriage: prevalence, risk factors and long-term reproductive outcome, Human Reproduction Update 2014;20(2):262–78. | |
Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy Green-top Guideline No. 21, 2016. | |
Kirk E et al. The diagnostic effectiveness of an initial transvaginal scan in detecting ectopic pregnancy. Hum Reprod 2007;22:2824–8. | |
Mavrelos D et al. Efficacy and safety of a clinical protocol for expectant management of selected women diagnosed with a tubal ectopic pregnancy. Ultrasound Obstet Gynecol 2013;42:102–7. | |
Jurkovic D et al. Single-dose systemic methotrexate vs. expectant management for treatment of tubal ectopic pregnancy: a placebo-controlled randomized trial. Ultrasound Obstet Gynecol 2017;49(2):171–6. DOI: 10.1002/uog.17329. Epub 2017 Jan 6. | |
Farahani L et al. Negative histology with surgically treated tubal ectopic pregnancies – a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 2017;213:98–101. DOI: 10.1016/j.ejogrb.2017.04.001. Epub 2017 Apr 2. | |
Mol F et al. Salpingotomy versus salpingectomy in women with tubal pregnancy (ESEP study): an open-label, multicenter, randomized controlled trial. Lancet 2014;383(9927):1483–9. DOI: 10.1016/S0140-6736(14)60123-9. Epub 2014 Feb 3. | |
Royal College of Obstetricians and Gynaecologists. The management of gestational trophoblastic disease. Green-top Guideline No. 38, 2010. | |
Graham A, Johns J. Book chapter. Gestational Trophoblastic disease. In: Kirk E. (ed.) Early pregnancy ultrasound: a practical guide. Cambridge University Press, 2017. | |
Johns J, Greenwold N, Buckley S, Jauniaux E. A prospective study of ultrasound screening for molar pregnancies in missed miscarriages. Ultrasound Obstet Gynaecol 2005;25:493–7. | |
Kirk E et al. The accuracy of first trimester ultrasound in the diagnosis of hydatidiform mole. Ultrasound Obstet Gynecol 2007;29:70–5. | |
Jauniaux E et al. New insights in the pathophysiology of complete hydatidiform mole. Placenta 2018;62:28–33. DOI: 10.1016/j.placenta.2017.12.008. Epub 2017 Dec 16. | |
Qureshi H et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med 2014;24(1):8–20. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards programme CLICK HERE)

