This chapter should be cited as follows:
Liu B, Khalil A, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.412603
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 4
Fetal development and maternal adaptation
Volume Editor: Professor Asma Khalil, The Royal College of Obstetricians and Gynaecologists, London, UK; Fetal Medicine Unit, Department of Obstetrics and Gynaecology, St George’s University Hospitals NHS Foundation Trust, London, UK
Chapter
Selective Fetal Reduction in Multiple Pregnancies
First published: February 2021
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
Following the rise of assisted reproductive techniques, the incidence of higher order multiples has also increased in the recent decades. This results in complications for the pregnancy, such as miscarriage, extreme preterm deliveries, stillbirth, and pre-eclampsia. These have short- and long-term implications on the physical and mental health of the children, as well as the quality of life for the families. Here we discuss the evidence-based risks and benefits of selective fetal reduction in different types of multiple pregnancies, the different techniques used, and the ethical dilemmas faced by the families.
BACKGROUND
The incidence of multiple pregnancies has increased significantly in the recent years due to the popular use of assisted reproductive techniques.1 Following the peak incidence of higher order multiples in the United States in 1998 (1.935 : 1000 births), the incidence has now reduced to 1.30 : 1000 births.2,3 Despite the reduction of trichorionic triplets through the limitation of embryo transfer to two in the UK, the relative number of mixed chorionicity triplets has increased due to splitting of the embryo,4 as well as ovarian hyperstimulation through the use of gonadotropins in ovulation induction methods.5
Multiple pregnancies can have significant impacts on the health of mothers and fetuses antenatally, and in the long term, with higher order pregnancies being at an increased risk of complications than twin pregnancies. Mothers are predisposed to conditions such as hypertensive disorders of pregnancy, including pre-eclampsia, gestational diabetes, and postpartum hemorrhage.6 Miscarriage, preterm deliveries, and stillbirth are further increased in higher order multiple pregnancies, where one-third of triplets are predicted to be born before 32 weeks.7 This leads to cerebral palsy, developmental delay, learning and behavioral difficulties, chronic lung disease, and death.8 Complications specific to monochorionic pregnancies, such as twin-to-twin transfusion syndrome (TTTS), selective fetal growth restriction (sFGR), and twin anemia-polycythemia sequence (TAPS), can further impact the outcome of the pregnancy.
Social and financial implications can also adversely influence the families of multiples, with higher financial demands, stress and depression of the parents, leading to higher divorce rates and poorer family relationships.9
It is therefore recommended by the Royal College and the American College of Obstetricians and Gynecologists, that in all higher order pregnancies (triplets or more), selective fetal reduction should be discussed.9,10
RISKS AND BENEFITS OF SELECTIVE FETAL REDUCTION: CURRENT EVIDENCE
Trichorionic-triamniotic triplets
Clinicians counseling expectant parents of triplets about selective fetal reduction should be familiar with the current evidence of the risks and benefits of expectant management, and reducing the pregnancy to two, or one fetus. Patient choice can be dependent on their socioeconomic situation, fertility, fetal well-being, and background medical condition.9
A retrospective study analyzed the rates of miscarriage, preterm births before 33 weeks, and survival rates of 528 trichorionic triplets (TCT). It was found that if expectantly managed, 3.9% of women miscarried, and 34.5% delivered very prematurely. The rate of at least one survivor in this group was 94.8%. Miscarriage rates were increased with selective reduction – to 7.9% after reducing to two fetuses, and 14.7% after reducing down to one. Survival rate was also reduced following selective reduction – with chances of 91.7% after reducing to two fetuses, and 82.4% after reducing to one. Despite these negative impacts, significant benefits were seen with selective reduction in the rates of preterm births, where this was decreased to 14.8% after reducing to two fetuses, and only 6.9% after reducing to one. Further literature reviews of other similar studies have confirmed similar findings. It is estimated that five reductions to two fetuses were required to prevent one preterm birth, versus reductions four to one fetus. Whereas one miscarriage will occur following 24 reductions to two fetuses, and one of 12 will miscarriage if reduced to one fetus.7
Therefore, the higher the number of fetuses reduced can increase the rates of miscarriage, and reduce the survival rates of the fetuses, but will give significantly better prognosis in reducing preterm births and their complications.
Dichorionic-triamniotic triplets
These triplets pose further dilemmas in the decisions required to be made by expectant parents and clinicians, due to the chorionicity. A retrospective study showed that such triplets have a 5.5-fold increased risk of perinatal mortality than TCT triplets, and are therefore, considered at higher risk of poor outcomes.11 Reduction of the dichorionic triplet, leaving behind monochorionic twins, could still expose them to the risks of TTTS, TAPS, and sFGR. However, reduction of one of the monochorionic triplets, leaving dichorionic diamniotic (DCDA) twins, could have more implications for the remaining monochorionic triplet, such as neurological deficits.
A systematic review of 331 dichorionic triplets (DCT) revealed a miscarriage rate of 8.9% and a preterm birth (before 32 weeks) rate of 33.3% in expectantly managed triplets. When one fetus of the monochorionic pair was reduced, the miscarriage rate remained the same, but the preterm birth rate was significantly lower at 11.8%. The miscarriage rate following reduction of the dichorionic triplet was higher at 23.5%, and preterm birth 17.6%. Reduction of both the monochorionic pair – retaining the dichorionic fetus, resulted in a miscarriage rate of 14.5% and a preterm birth rate of 5.5%. It was calculated that four fetuses of the monochorionic pair needed to be reduced to prevent one preterm birth, and five of the dichorionic fetus for the same outcome.12
These outcomes were similar to those of the TCT pregnancies, where more preterm births were decreased with the increasing number of fetuses reduced, with higher miscarriage rates. However, it appears that the outcomes were improved following the reduction of one of the monochorionic fetuses, than the dichorionic fetus.
1
Risk of miscarriage and preterm birth (PTB) following reduction in triplets according to chorionicity and number reduced.
Miscarriage (%) | PTB <34 weeks (%) | |
TCTA expectant | 3 | 52 |
TCTA SR to 2 | 7 | 21 |
TCTA SR to 1 | 12 | 10 |
DCTA expectant | 9 | 67 |
DCTA SR to 2 | 13 | 31 |
DCTA SR to 1 | 17 | 9 |
TCTA, trichorionic triamniotic triplets; SR, selective reduction; DCTA, dichorionic triamniotic triplets.
Monochorionic triplets
Monochorionic triamniotic (MCT) and monochorionic monoamniotic (MCM) triplets are exceedingly rare. These pregnancies are often complicated by TTTS, TAPS, sFGR, and fetal loss. MCM pregnancies also have a risk of cord entanglement.
One reported study looking into selective reduction of monochorionic pregnancies consisted of two cases of MCT triplets. Both reductions took place at 13 weeks' gestation, and neither of the cases resulted in miscarriages or fetal loss. Both sets of resulting twins were delivered live at gestations of 36 and 38 weeks.13 There is currently no literature on selective reduction of MCM triplets, mostly likely due to their rarity and early poor outcomes.
Twins
Selective reduction in twins is often offered when there is an abnormality in one twin, or in complications such as TTTS or twin reversed arterial perfusion sequence (TRAP). In these cases the prognosis of the affected twin is explained to the expectant parents, and its effect on the other twin, if any. Other less common indications for offering this in twin pregnancies may include maternal medical concerns such as previous severe pre-eclampsia, or a history of cervical incompetence or preterm deliveries (Figure 1).9 One retrospective cohort study analyzed the adverse pregnancy outcomes in ongoing twin pregnancies versus twin pregnancies that were reduced to singletons. Of the 501 ongoing twin pregnancies and 63 that were reduced to singletons, the rate of preterm deliveries before 37 weeks was reduced from 43% to 10% in the singletons, but no difference was found in preterm delivery rates before 34 weeks. The reduction group was also found to have less babies with a low birth weight below the 10th centile than the twin group (23% and 48%, respectively), but no significant difference in weights below the 5th centile. It was also noted that there was no difference in stillbirth rates between the two groups.14

1
Two-dimensional ultrasound image displaying dichorionic diamniotic (DCDA) twins at 12 weeks' gestation, with the characteristic lambda sign.
Selective reduction of twins due to the multiple nature of the pregnancy is, however, a controversial issue. Some patients may wish for this due to social or psychological reasons. These patients must be carefully counseled regarding the risks to the pregnancy, the long-term psychological impacts, and be provided with any written information that is required.9
2
Risk of preterm birth (PTB), small for gestational age (SGA), and intrauterine death (IUD) in twin pregnancies versus reduction to singletons.
Twin pregnancies (n = 501) | Twins reduced to singletons (n = 63) | |
Spontaneous PTB <37 weeks | 43% | 10% |
Spontaneous PTB <34 weeks | 12% | 5% |
Spontaneous PTB <28 weeks | 2% | 3% |
SGA <10th centile | 49% | 23% |
SGA <5th centile | 28% | 16% |
IUD >24 weeks | 0.4% | 0% |
PROCEDURE AND TECHNIQUES
Several methods for selective fetal reduction have been described, which are chosen based upon chorionicity, risk profile, and expertise of the practitioner. The timing of reduction impacts the rates of miscarriage and preterm birth, where earlier reduction, particularly in the first trimester, can result in a smaller rate of fetal loss.
Parents can be offered late reductions in the third trimester if the diagnoses of single fetal anomaly was made in the second trimester, reducing the risk to the remaining fetus(es) to preterm delivery only.15
Late reductions, however, may not be permitted by the law in some countries, and could be more distressing to the parents; therefore, careful and sensitive counseling should be taken to balance all the risks and benefits.
Intrathoracic potassium chloride
Chorionicity should be determined using ultrasound by 13+6 weeks' gestation.15
Chorionicity is usually determined during the routine combined screening for trisomies and other fetal abnormalities, but can sometimes be detected earlier if an early scan was performed for other indications. Selective fetal reduction should be offered to the expectant parents at the earliest availability, after counseling and with consent.
In cases of TCT triplets, or DCT triplets where the decision has been made to reduce the dichorionic triplet, or to reduce both the monochorionic fetuses, intrathoracic potassium chloride (KCl) is the preferred method.15
Intrathoracic KCl is performed under ultrasound guidance, with a single injection into the thorax of the fetus until asystole is witnessed. This has been reported to have a 99.5–100% success rate with minimal maternal complications.16
Bipolar cord coagulation
In monochorionic pregnancies, i.e. reduction of one of the monochorionic fetuses in DCT triplets, or in MC twins or triplets, KCl injection could result in the death or neurological impairment of the other fetus(es) sharing the placenta, due to its leakage through the placental vascular anastomoses, and to acute hypotension and hypoxia as blood is shunted through the placental vasculature of the dying twin.17
Therefore, selective reduction in monochorionic pregnancies should be performed using bipolar cord coagulation, radiofrequency ablation, or intrafetal laser ablation.15
Bipolar cord coagulation is commonly performed using regional anesthetic, under ultrasound guidance. 10-F trocars are inserted into the uterus and cord occlusion is performed with bipolar forceps, at 30–50 W, for 30 seconds.18 Prophylactic antibiotics are given prior to the procedure, and a tocolytic agent given after. Studies investigating the outcomes following this procedure in twin pregnancies reported survival rates of the remaining fetus to be as high as 82%,19 with a preterm premature rupture of the membranes (PPROM) rate of 21.9%, and preterm birth rate of 44% following the procedure.20
Radiofrequency ablation
Radiofrequency ablation is an alternative technique to bipolar cord coagulation, used for the same types of monochorionic triplets and twins. This can be performed under local anesthesia, under ultrasound guidance; a radiofrequency needle is inserted adjacent to the umbilical cord insertion into the fetal abdomen as demonstrated in Figure 2. Radiofrequency energy is then applied to generate 100°C for several minutes, and may need to be repeated, until no further blood flow is seen.18
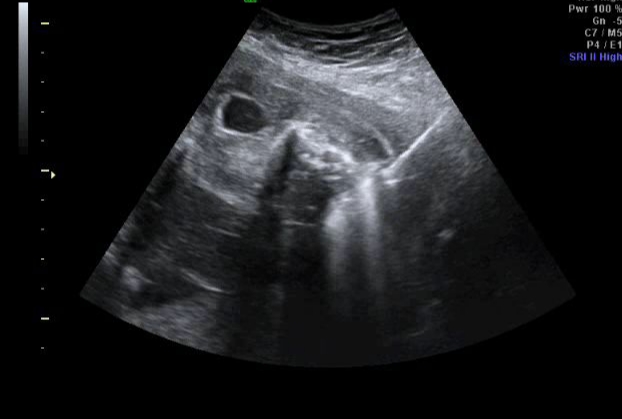
2
Two-dimensional ultrasound image demonstrating radiofrequency ablation of twin arterial perfusion sequence (TRAP mass).
A study has compared this technique with bipolar cord coagulation, where radiofrequency ablation has a lower, but statistically insignificant number of postprocedural complications, but a significantly lower rate of adverse perinatal outcomes. It was also reported that the mean gestational age of delivery was later in women who had undergone this technique rather than in the cord coagulation group, and the birth weight of the remaining babies were also higher.18
Fetoscopic and intrafetal laser ablation
Fetoscopic and intrafetal laser ablation can also be used for monochorionic pregnancies. Fetoscopic laser ablation is used similarly to in TTTS, where following the insertion of the fetoscope into the uterus under local anesthesia, laser coagulation is used to ablate the umbilical cord of the fetus, until no color pulsations are seen (Video 1). Intrafetal laser ablation is a more recently described technique, where the laser needle is inserted into the fetal abdomen adjacent to the pelvic vessels, and laser coagulation applied until no color flow is seen in the iliac arteries and umbilical vein as demonstrated in Video 2.17 The latter technique, however, had a co-twin death rate of 46% within 2 weeks following the procedure, likely secondary to bleeding into the placenta of the dead fetus.17
1
Fetoscopic video demonstrating cord ablation using CO2 laser.
2
Two-dimensional ultrasound video demonstrating intrafetal laser ablation of twin reversed arterial perfusion (TRAP).
New developments
Potential new techniques of selective fetal reduction are currently being developed. Microwave ablation has been tried on a small number of pregnancies, where a coaxial antenna emitting microwave energies is inserted into the fetal abdomen, and the energy applied for 3 minutes. It has potential advantages over laser ablation in that the coagulation effect is seen immediately, a larger area can be covered, and a minimal heat sink effect means less ablation zone distortion.21
High intensity focused ultrasound aims to bring a non-invasive technique into fetal therapy. A transducer is placed on the women’s abdomen and targeted ultrasound energy is transmitted through the abdominal wall and uterus to cause vessel occlusion. Currently this has been limited to animal studies, and small numbers of TRAP sequence and TTTS cases, however, due to a high number of incomplete vascular occlusions, it has not yet been proven to be superior to other methods.22
ETHICS OF PATIENT COUNSELING
As demonstrated above, the decision making required by the expectant parents is extremely difficult, given the risks of miscarriage associated with the procedure, balanced against the benefits of risk reduction for preterm births and adverse maternal outcomes.
The clinician providing the information must be able to counsel the parents in a non-biased manner, explaining the factual information including the risks and benefits, and be respectful of the parents’ autonomy and values in this dilemma. It is important to individualize each case according to the woman’s background situation, such as health, social and financial status, religion, fertility, and most importantly, her wishes.
This is aimed at maximizing the benefits, and minimizing the risks. The information should be provided promptly following the diagnosis of a higher order pregnancy, and time given for the parents to process and make their decision on this matter.9
It is recommended that these women are referred to a tertiary fetal medicine center where they can undergo frequent ultrasound surveillance, with the procedure being performed by an experienced fetal medicine specialist. The counseling must be provided by a clinician with appropriate skill and knowledge in this area.10,9
Research has shown that even after 1 year following the selective reduction procedure, one-third of mothers still suffered from depressive symptoms of sadness and guilt.23
CONCLUSION
Selective fetal reduction is a complex area where both risks and benefits to the pregnancy are well documented. Clinicians must be familiar with the facts involved in this area, and provide the counseling in a sensitive, non-judgmental manner. Referral to a fetal medicine center should be made, whether it is to carry out the procedure by a specialist, or to provide close monitoring of the complex higher order pregnancy.10 The patient’s decision must always be respected, and support provided where needed.
PRACTICE RECOMMENDATIONS
- In all higher order pregnancies, selective fetal reduction should be discussed.
- Clinicians counseling expectant parents of triplets about selective fetal reduction should be familiar with the current evidence of the risks and benefits of expectant management, and reducing the pregnancy to two, or one fetus.
- Parents wishing to undergo selective reduction in twin pregnancies must be carefully counseled regarding the risks to the pregnancy, the long-term psychological impacts, and be provided with any written information that is required.
- Chorionicity should be determined using ultrasound by 13+6 weeks 'gestation.
- Selective fetal reduction should be offered to the expectant parents at the earliest availability, after careful counseling, taking into account their individual circumstances.
- Decisions on the timing of selective reduction due to single fetal anomalies should be discussed, and careful and sensitive counseling should be taken to balance all the risks and benefits.
- Intrathoracic KCl injection should not be used in monochorionic pregnancies.
CONFLICTS OF INTEREST
Author(s) statement awaited.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Blondel B, Kaminski M. Trends in the occurrence, determinants, and consequences of multiple births. Semin Perinatol 2002;26:239 e49. | |
Martin JA, Hamilton BE, Osterman MJ. Three decades of twin births in the United States, 1980–2009. HCS data brief 2012;(80):1–8. | |
Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep 2017;66:1. | |
Schachter M, Raziel A, Friedler S, Strassburger D, Bern O, Ron-El R. Monozygotic twinning after assisted reproductive techniques: a phenomenon independent of micromanipulation. Hum Reprod 2001;16:1264–. | |
Gleicher N, Oleske DM, Tur-Kaspa I, Vidali A, Karande V. Reducing the risk of high order pregnancy after ovarian stimulation with gonadotrophins. N Engl J Med 2000;343:2–7. | |
Luke B, Brown MB. Contemporary risks of maternal morbidities and adverse outcomes increasing maternal age and plurality. Fertil Steril 2007;88:283–93. | |
Chaveeva P, Kosinski P, Puglia D, Poon LC, Nicolaides KH. Trichorionic and dichorionic triplet pregnancies at 10–14 weeks: outcome after embryo reduction compared to expectant management. Fetal Diagn Ther 2013;34:199–. | |
Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Practice Bulletin No 169. American College of Obstetricians and Gynaecologists. Obstet Gynecol 2016;128:e131–46. | |
ACOG Committee Opinion. Multifetal Pregnancy Reduction. The American College of Obstetricians and Gynecologists. 2017;719. | |
Royal College of Obstetricians and Gynaecologists. Management of Monochorionic Twin Pregnancy. Green-top guideline No.51. London: RCOG 2016. | |
Adegbite AL, Ward SB, Bajoria R. Perinatal outcome of spontaneously conceived triplet pregnancies in relation to chorionicity. AJOG 2005;194(4):1463–71. | |
Morlando M, Ferrara L, D’Antonio F et al. Dichorionic triplet pregnancies: risk of miscarriage and severe preterm delivery with fetal reduction versus expectant management. Outcomes of a cohort study and systematic review. BJOG 2015. DOI: 10.1111/1471-0528.13348. | |
Paramasivam G, Wimalasundera R, Wiechec M et al. Radiofrequency ablation for selective reduction in complex monochorionic pregnancies. BJOG 2010. DOI: 10.1111/j.1471-0528.2010.02624.x. | |
Gupta S, Feinberg J, Fox N et al. Adverse pregnancy outcomes in twin pregnancies reduced to singleton pregnancies and ongoing twin pregnancies. AJOG 2015;212(1):S416–7. | |
ISUOG Practice Guidelines: The role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol 2016;47:247–63. | |
Sfakianaki AK, Davis KJ, Copel JA et al. Potassium Chloride induced fetal demise – A retrospective cohort study into efficacy and safety. J Ultrasound Med 2014;33:337–41. | |
Chaveeva P, Peeva G, Pugliese SG, Shterev A, Nicolaides KH. Intrafetal laser ablation for embryo reduction from dichorionic triplets to dichorionic twins. Ultrasound Obstet Gynecol 2017;50:632–4. | |
Yinon Y, Ashwal E, Weisz B et al. Selective reduction in complicated monochorionic twins: prediction of obstetric outcome and comparison of techniques. Ultrasound Obstet Gynecol 2015;46:670–7. | |
Rossi C, D’Addario V. Umbilical cord occlusion for selective feticide in complicated monochorionic twins: systematic review of literature. Am J Obstet Gynecol 2009;200:123–9. | |
Bebbington MW, Danzer E, Moldenhauer J, Khalek N, Johnson MP. Radiofrequency ablation vs. bipolar umbilical cord coagulation in the management of complicated monochorionic pregnancies. Ultrasound Obstet Gynecol 2012;40:319–24. | |
Prefumo F, Cabassa P, Fichera A et al. Preliminary experience with microwave ablation for selective feticide in monochorionic twin pregnancies. Ultrasound Obstet Gynecol 2013;41(4):470–1. | |
Seo K, Ichizuka K, Okai T et al. Twin-Reversed arterial perfusion sequence using high-intensity focused ultrasound therapy. Ultrasound Obstet Gynecol 2018. | |
Garel M, Stark C, Blondel B et al. Psychological reactions after multifetal pregnancy reduction: a 2-year follow up study. Hum Reprod 1997;12(3):617–22. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards programme CLICK HERE)


