Toward Perinatal Electronic Medical Record For Obstetrics
Authors
INTRODUCTION
Computerized perinatal database systems have been integral parts of clinical and research programs at academic obstetrics/gynecology departments since the 1970s.1 These relational databases optimally link all obstetric data with both short- and long-term neonatal outcomes They are episodic and longitudinal databases designed to enhance clinical care and expedite epidemiologic research2. Specifically, the ability to develop large perinatal datasets has facilitated the study of infrequent but critically important pregnancy complications. Clinically, they have traditionally been used for obstetric risk assessment for improved recognition of high-risk conditions (i.e., preterm birth, congenital anomalies) in order to target effective interventions or alter management. Over the last decade there has been a shift in the direction of perinatal databases from being used as risk-assessment tools to more of a computerized patient record. This chapter identifies some of the issues that are involved in this transition of the perinatal database to a perinatal electronic medical record (EMR) and provides examples of key issues confronting clinician-scientists who use these systems for both patient care and research.
PAST AND PRESENT
At Wayne State University/Hutzel Hospital, the Problem Oriented Perinatal Risk Assessment System (POPRAS) forms for perinatal risk assessment have been in use since 1985.3 Demographic and antenatal data were recorded at prenatal care sites and then sent to Hutzel Hospital for direct entry by trained technicians who batch-enter data after checks for completeness and internal consistency. It supported immediate availability of ultrasound reports and other key clinical information at multiple sites where care was provided. It has captured extensive obstetric and neonatal outcome data for more than 130,000 consecutive births. The perinatal database was a single relational database in the Microsoft Access format and its data could be converted into one of many different statistical programs and is thus accessible to faculty and fellows for research purposes.
Although this database was an exceptional source of resources for clinical care and clinical research, a need arose in the last few years to replace it. This decision was made for several indications. Because of the explosion of different facets of medical information and technology in the field of perinatal medicine, the need to provide additional detail in specific subspecialties became apparent. Areas that required extensive modernization included clinical and research data for patients with human immunodeficiency virus (HIV) infection, critical care disorders, thrombophilia disorders, genetic disorders including those undergoing invasive procedures such as cordocentesis, fetal bladder shunting, chorionic villous sampling, amniocentesis, and fetal surgery. Technological advances of two-dimensional (2D; improved resolution) pulsed-wave and color Doppler, three-dimensional (3D), and four-dimensional (4D) ultrasound all required updates to our current ultrasound system. Another reason for the need to redesign the database included the increased importance of postobstetric outcomes. With the performance of outcomes-based research, the requirement to be able to link obstetric data to both neonatal short-term (neonatal intensive care unit [NICU] outcomes) and longer term (neurodevelopmental follow-up through 3 to 5 years of age) became necessary. The increasing number of different practice sites (prenatal or delivery) as well as the turnover/changes in these sites made offsite data collection more difficult because the records were transferred to our main hospital as paper documents. This affected the timeliness of delivery of the data, and increased the risk of missing data. Also, because the number of providers who were not centrally located was increasing and therefore less monitoring of data collection occurred, this affected the amount of missing data as well as its validity. Last, issues of the performance, reliability, life span, and cost effectiveness of the software and hardware that we had been using were becoming increasingly problematic.
TECHNOLOGY ISSUES
Because of the significant manpower costs associated with the type of offline data entry we had used throughout the life span of the perinatal database (three full-time data entry personnel and one data entry supervisor), the feasibility of financially supporting a team of specific data entry personnel only for obstetrics services was decreasing. The costs associated with attempting to network this Access-based application over multiple sites were another problem. Finally, the limitation of Access as a platform that includes difficulties with larger records sets, multiple users, and frequent crashes or slower speeds was readily apparent.
For these reasons, WSU decided to invest in the development and application of an EMR that runs over the Internet. There are several potential advantages and disadvantages to this approach (Table 1). First, if the perinatal EMR is maintained through an Application Service Provider (ASP), there is limited computer and network infrastructure costs. As long as there is access to high-speed Internet connections, which are available at relatively low costs at most health care sites, standard desktop computers can readily be used. Because the EMR application is administrated and maintained over the Internet at the server level, there is a low burden on the local client computer, which further decreases the departmental burden on in-house information technology support. The second advantage is immediate and widespread access to data from different health care sites. Although a patient may have antenatal encounters at her prenatal care clinic or an offsite ultrasound unit, these data may be input into the same database that ultimately contains all inpatient data, thus providing a potentially more seamless integration of antenatal outpatient and inpatient data. Furthermore, if the same EMR is used within a medical center but at different hospitals, there is the potential for more uniform data collection, more consistent data definitions, and subsequently improved clinical care. This may be increased further if disease-specific clinical pathways as well as a quality assurance program are part of the EMR.
Table 1. Potential advantages and disadvantages of an Internet-based perinatal database
Advantages | Disadvantages |
Limited computer and network costs | Unknown future down time of Internet |
Immediate and widespread access | Security of system or data from “hackers,” denial of service attacks, or viruses. |
More standardized collection of data across health care system | Unknown effect of future governmental regulations |
Lower in-house IT costs |
IT, information technology.
There are currently few entirely Web-based perinatal database systems in clinical use. Concern over the stability and reliability of Internet access coupled with unknown security risks are major reasons for this hesitation. Although high-speed Internet access is relatively easy and inexpensive to obtain, the unknown risk of system downtime because of a virus or denial of service attacks still plague potential users. Furthermore, security and privacy of sensitive patient data is another issue. The potential for unauthorized remote access by hackers to patient information such as genetic testing or HIV results remains of concern. Despite the use of security measures such as user name and password protection, role-based security, IP address restriction, and data encryption, administrators and risk managers remain wary. Anticipated governmental guidelines for the electronic transmission of patient information are a further potential burden that affects initiation of an Internet-based system. This is because of the fear of an inability to be compliant with these regulations and the potential punitive action from the government.4
EXAMPLES
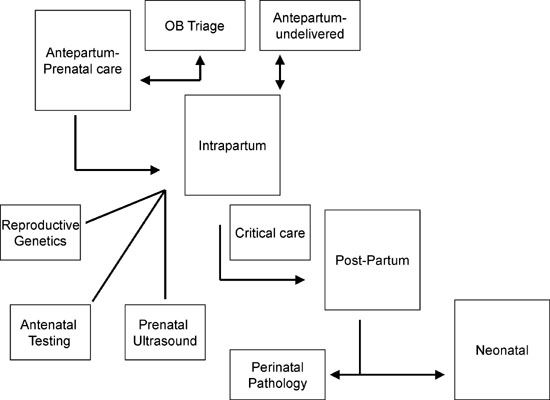
Regardless of the technology used, careful planning must be done to ensure that the perinatal EMR, whether purchased as an off-the-shelf product or developed as a “home-grown product,” has adequate performance and features to justify the large financial commitment that is often required. In the following section, we describe the architecture and framework for one section of a perinatal EMR (Fig. 1) to illustrate key concepts. They include a First Trimester Genetic Screening Module and Multidisciplinary Dysmorphology Database Module. We have chosen these as examples because they combine several aspects of data (clinical, biochemical laboratory results, ultrasound images) and are important for both clinical patient care and research.
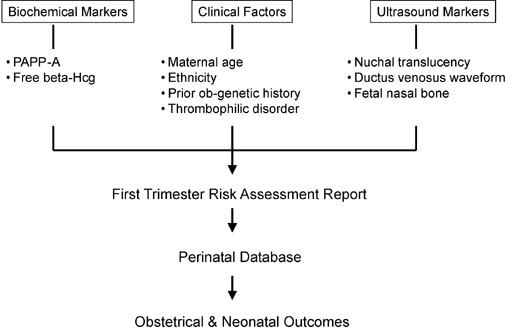
There is significant interest in the combined use of biochemical and ultrasound markers in the first trimester for the detection of aneuploidy and for the prediction of adverse pregnancy outcomes. Clinical guidelines have now been disseminated that advocates all eligible women should be offered the option for first trimester screening. In order to prospectively collect quality research data, as well integrate it with the available clinical information, an “Integrated” First Trimester Genetic Screening Module could be used. This module would combine maternal demographic and clinical data, maternal biochemical markers, first trimester ultrasound markers, and results of invasive genetic tests (Fig. 2). It would display maternal age, maternal serum free β-human chorionic gonadotropin (β-hCG) and pregnancy-associated plasma protein–A levels, ultrasound images of nuchal translucency measurement, ductus venosus waveform, and fetal profile for identification of the nasal bone in one report. It would also provide risk assessment based on these individual markers or in combination, as well as normative and/or adjusted values. For both quality-control purposes, a digital image of each ultrasound marker could be part of the report. Finally, consideration should be given for future expansion and incorporation of new tests (as they are developed).
|
Integration and dissemination of this information to genetic counselors, reproductive geneticists, maternal-fetal medicine specialists, and sonographers would promote collaboration between these disciplines and improved patient care. As more data are collected from ongoing clinical trials and clinical strategies are evaluated, this Integrated Genetic module could serve as a computer-based clinical support system that provides a specific patient risk which is based on ethnicity, maternal age, serum screening tests, and ultrasound markers.
The second example is a Multidisciplinary Dysmorphology Database. This Web-based database combines data input from maternal-fetal medicine, prenatal imaging, reproductive and pediatric genetics, pediatric dysmorphology, and perinatal pathology (Fig. 3). For each case, clinical information and cytogenetic results are linked with prenatal images from 2D ultrasound, 3D/4D ultrasound, and ultrafast fetal magnetic resonance imaging (MRI). Finally, perinatal pathologists contribute autopsy data including photographs of gross pathology, results of other postmortem imaging studies (radiography, dye studies, MRI), and histology findings. All cases are electronically archived and users with permission are able to search cases by ultrasound and/or cytogenetic findings, by diagnosis, and finally by key word(s). Interesting or difficult cases are presented at a monthly Dysmorphology Conference. This interdisciplinary approach has been successful at other institutions.5
SUMMARY
In summary, regardless of the manner in which data are collected as part of a perinatal database, a good system must have three basic features. It must link information from all obstetric encounters; antepartum and delivery information must be linked to all other clinical information, such as data from prenatal ultrasound and genetic testing. Second, obstetric conditions and outcomes must be actively linked to neonatal data; the disconnection of these data elements threatens the utility of having a perinatal database. Finally, data must able to be retrieved from the database, not merely collected, in order to be useful for research and vital statistics reporting. Most likely, future perinatal databases and/or EMRs will be accessed and used over the Internet. In fact there are several products already on the market. It is important to evaluate in detail the system requirements and features that one need’s in a database, whether pure clinical reporting, detailed outcomes-based research, risk management reduction, or a combination of these.
REFERENCES
Rosen MG, Sokol RJ, Chik L: Use of computers in the labor and delivery suite: An overview. Am J Obstet Gynecol 132:589, 1978 |
|
Chik L, Sokol J, Kooi R, et al: A perinatal database management system. Methods Inf Med 20:133, 1981 |
|
Sokol RJ, Chik L: Perinatal computing. An overview Acta Obstet Gynecol Scand Suppl 109:7, 1982 |
|
The buzz on HIPAA. How HIPAA will affect the electronic transmission of health information Health Devices 29:472, 2000 |
|
Tennstedt C, Hufnagl P, Korner H, et al: Fetal autopsy: The most important contribution of pathology in a center for perinatal medicine. Fetal Diagn Ther 6:384, 2001 |